Copyright
©2010 Baishideng Publishing Group Co.
World J Cardiol. Nov 26, 2010; 2(11): 377-390
Published online Nov 26, 2010. doi: 10.4330/wjc.v2.i11.377
Published online Nov 26, 2010. doi: 10.4330/wjc.v2.i11.377
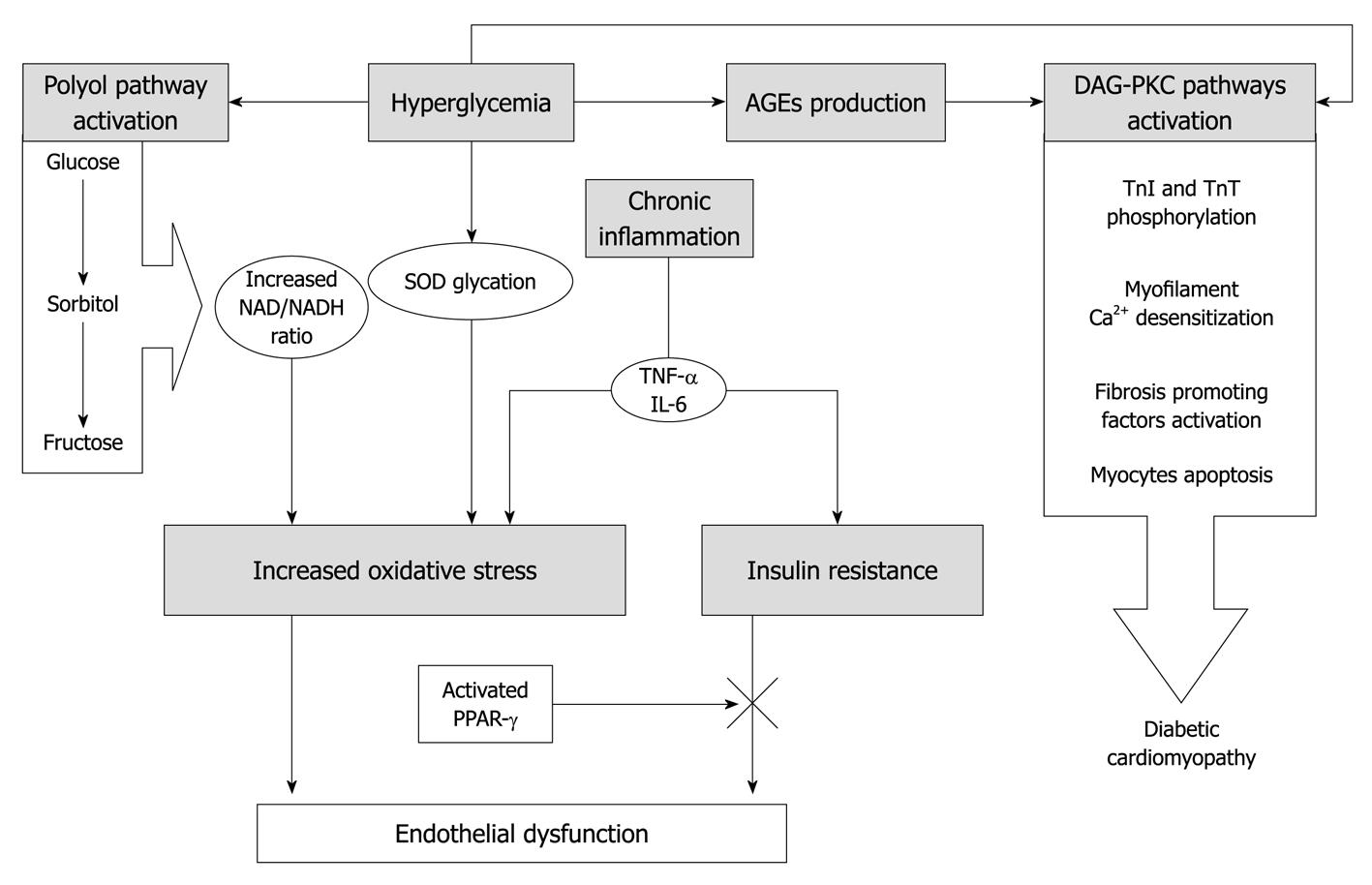
Figure 1 Etiology of mechanisms involved in coronary vascular dysfunction in diabetes.
Increased oxidative stress is the unifying element common to all pathways through which the various mechanisms described interact to cause endothelial dysfunction and cardiomyopathy in diabetes. Hyperglycemia acts directly through the glycation of the scavenger enzyme superoxide dismutase (SOD) and other antioxidant enzymes, and indirectly through the cross activation of advanced glycation end product (AGE)/advanced glycation end product receptor (RAGE) interaction and of the polyol pathway. The latter raises the NADH/NAD+ ratio, modifying the redox state of the cells and leading to the production of superoxide anions. Tumor necrosis factor-α (TNF-α) has been shown to affect intracellular insulin signaling, promoting insulin resistance and consequently impairing the insulin-mediated endothelial function in coronary arterioles. The insulin-resistance mediated endothelial dysfunction can be restored by the activation of peroxisome proliferator-activated receptor-γ by thiazolidinediones and rosiglitazone. Then, if we consider diabetes as a chronic, subclinical inflammatory disease, it acts through TNF-α and Interleukin (IL)-6, increasing the cellular oxidative stress. AGE/RAGE interaction and hyperglycemia can in turn activate the diacylglycerol (DAG)-protein kinase C (PKC) pathway, thus promoting fibrosis, myofilament desensitization, and apoptosis, and finally leads to diabetic cardiomyopathy. TnI: Troponin I; TnT: Troponin T.
- Citation: Picchi A, Capobianco S, Qiu T, Focardi M, Zou X, Cao JM, Zhang C. Coronary microvascular dysfunction in diabetes mellitus: A review. World J Cardiol 2010; 2(11): 377-390
- URL: https://www.wjgnet.com/1949-8462/full/v2/i11/377.htm
- DOI: https://dx.doi.org/10.4330/wjc.v2.i11.377