Published online Apr 26, 2024. doi: 10.4330/wjc.v16.i4.173
Peer-review started: November 28, 2023
First decision: January 17, 2024
Revised: January 28, 2024
Accepted: March 1, 2024
Article in press: March 1, 2024
Published online: April 26, 2024
Coronary artery anomaly is known as one of the causes of angina pectoris and sudden death and is an important clinical entity that cannot be overlooked. The incidence of coronary artery anomalies is as low as 1%-2% of the general popu
Core Tip: The incidence of coronary artery anomalies is as low as 1%-2% in the general population, even when the various types are combined. Among these, the R-1 subtype in a single coronary artery is extremely rare. In this case report by Zhou et al, emission computed tomography showed that ischemia occurred in an area where the coronary artery was not visible to the naked eye. Meticulous follow-up is crucial because sudden death may occur owing to a single coronary artery. Furthermore, atherosclerosis prevention is important because percutaneous coronary intervention could pose a high risk when necessary for such anomaly.
- Citation: Ito S. Challenging situation of coronary artery anomaly associated with ischemia and/or risk of sudden death. World J Cardiol 2024; 16(4): 173-176
- URL: https://www.wjgnet.com/1949-8462/full/v16/i4/173.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i4.173
Like many organs, the coronary arteries have congenital anomalies. Anomalous origin, course, and termination of the coronary artery are often discovered by chance. In a single coronary artery as in this case[1], the origin of either the left or right coronary artery itself may not exist. Coronary artery anomaly is known as one of the causes of angina pectoris and sudden death and is an important clinical entity that cannot be overlooked. The frequency of coronary artery anomaly is often calculated based on data from catheter-based coronary angiography. On the other hand, coronary angiography is almost always performed for some reason, so there is a possibility that the statistics are biased to some extent. In recent years, multi-row coronary computed tomography (CT) has been increasingly performed as a first-line procedure[2], which makes it easier to perform anatomical analysis of the flow site and its relationship to other structures, and the range of indications is wider than that of a catheter[3,4]. The incidence of coronary artery anomalies is as low as 1%-2% of the general population[5], even when the various types are combined, and there is a natural limit to experience many types alone. Whenever you encounter unusual coronary arteries, you should always refer to the literature on congenital anomalies to evaluate their frequency and characteristics. It is important to consider whether the anomaly alone can cause ischemia or pose a risk of sudden death[6,7].
Coronary anomalies are practically problematic when the left and right coronary ostium are not found around their normal positions during coronary angiography with a catheter. It is easy to increase the amount of contrast agent used by repeating the test images many times. Particularly in the emergency setting of acute coronary syndromes, the operator may be distracted and repeat unnecessary contrast injection. Since there are cases of coronary artery occlusion at the entrance, it is more important to differentiate between the presence or absence of congenital abnormalities. If the ostium cannot be found during normal catheterization, it is important to remember the presence of the anomaly at an early stage. Contrast imaging of the sinuses of Valsalva/aortic root should be performed as soon as possible. If there is atherosclerotic stenosis of the coronary artery with an anomaly and percutaneous coronary intervention (PCI) is required, the suitability of the guiding catheter at the entrance and the adequate back up force of the guiding catheter are issues[8-10]. The level of PCI risk itself should also be considered on a case-by-case basis. PCI of a single coronary artery, as in this case[1], is difficult[5]. Suppose there is a significant stenosis in the proximal area. In this case, the risk of PCI will be considerably higher than in the left main with normal coronary structure, since it includes the perfusion zone of all coronary arteries.
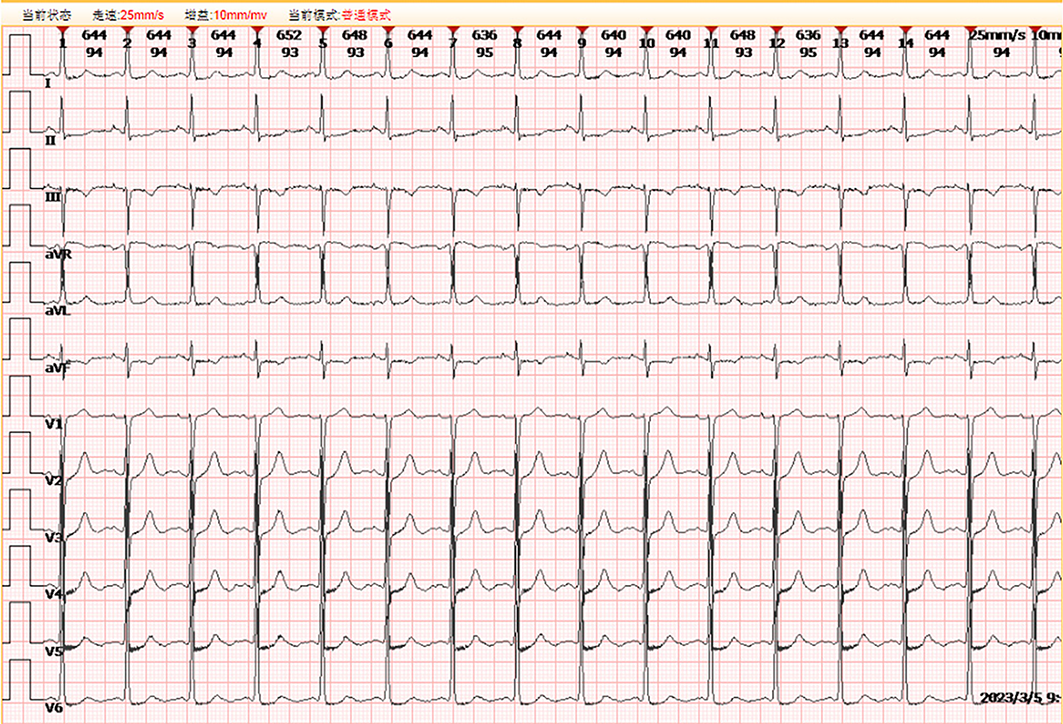
This case is very rare, and even a single case report contributed to the world "encyclopedia" of coronary anomalies as a valuable accumulation of cases[1]. Emission CT in the R-1 subtype single coronary artery proved that ischemia occurred in an area where the coronary artery was not visible to the naked eye, confirming the report of Chaikriangkrai et al[7]. In a 62-year-old female patient with diabetes mellitus, hypertension, and dyslipidemia presented with decreased exercise tolerance and poor blood pressure control, which began 2 wk before presentation. On a physical examination, her vital signs were as follows: body temperature, 37.3 °C; heart rate, 92 beats per minute; blood pressure, 151/86 mmHg; and body mass index, 23.4 kg/m2. Laboratory tests were negative for cardiac troponin I. Blood testing revealed low-density lipoprotein, high-density lipoprotein, and total cholesterol levels of 3.16, 1.19, and 4.96 mmol/L, respectively. The patient’s fasting blood glucose level was 9.49 mmol/L, while her 2-h postprandial blood glucose level was 22.54 mmol/L. Her glycosylated hemoglobin A1c level was 7.51%. Electrocardiography showed a normal sinus rhythm with mild depression in leads I, II, III, aVF, and V4-V6 (Figure 1). Coronary angiography detected no left coronary artery (Figure 2A and D) and that a single large coronary artery from the right sinus continued in the coronary sulcus (Figure 2B) and extended to the anterior base of the heart, terminating in a small vessel supplying the territory of the left anterior descending coronary artery (Figure 2C).
Although the presence of a single coronary artery was identified as the cause of decreased exercise tolerance only 2 wk prior, it is not easy to understand that this patient had no symptoms until she was 62 years old, because this anomaly is congenital. Thus, in addition to the ischemia associated with the anomaly, it cannot be ruled out that the increase in double products associated with increased blood pressure and/or the appearance of microcirculatory disorders[11] may have had an effect. Meticulous follow-up would be crucial, because it has been pointed out that sudden death may occur in single coronary arteries[7]. It is also mandatory to prevent atherosclerosis with their full efforts, as the authors indicated admirably.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Glumac S, Croatia S-Editor: Zhang H L-Editor: A P-Editor: Guo X
| 1. | Zhou YP, Wang LL, Qiu YG, Huang SW. R-I subtype single right coronary artery with congenital absence of left coronary system: A case report. World J Cardiol. 2023;15:649-654. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 2. | Pandey NN, Sinha M, Sharma A, Rajagopal R, Bhambri K, Kumar S. Anomalies of coronary artery origin: Evaluation on multidetector CT angiography. Clin Imaging. 2019;57:87-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Krishan S, Dhiman RK, Kalra N, Sharma R, Baijal SS, Arora A, Gulati A, Eapan A, Verma A, Keshava S, Mukund A, Deva S, Chaudhary R, Ganesan K, Taneja S, Gorsi U, Gamanagatti S, Madhusudan KS, Puri P, Shalimar, Govil S, Wadhavan M, Saigal S, Kumar A, Thapar S, Duseja A, Saraf N, Khandelwal A, Mukhopadyay S, Shetty N, Verma N. Corrigendum to "Joint Consensus Statement of the Indian National Association for Study of the Liver and Indian Radiological and Imaging Association for the Diagnosis and Imaging of Hepatocellular Carcinoma Incorporating Liver Imaging Reporting and Data System" [J Clin Expt Hepatol 9 (2019) 625-651]. J Clin Exp Hepatol. 2020;10:188. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 4. | Şahin T, Ilgar M. Investigation of the Frequency of Coronary Artery Anomalies in MDCT Coronary Angiography and Comparison of Atherosclerotic Involvement between Anomaly Types. Tomography. 2022;8:1631-1641. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 5. | Vijayvergiya R, Kasinadhuni G, Vemuri KS, Gupta A, Kumar B, Lal A, Revaiah PC, Rajan P, Uppal L. Percutaneous Coronary Revascularization in Patients With Single Coronary Artery. Cardiovasc Revasc Med. 2021;29:32-37. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 6. | Rosenthal RL, Carrothers IA, Schussler JM. Benign or malignant anomaly? Very high takeoff of the left main coronary artery above the left coronary sinus. Tex Heart Inst J. 2012;39:538-541. [PubMed] [Cited in This Article: ] |
| 7. | Chaikriangkrai K, Kassi M, Polsani V, Chang SM. Case report: single coronary artery with ischemia and sudden cardiac arrest. Methodist Debakey Cardiovasc J. 2014;10:121-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Cocco N, Madonna R, Cammalleri V, Cocco G, De Stefano D, Ricciardi D, Grigioni F, Ussia GP. Percutaneous treatment of a CTO in an anomalous right coronary artery: A rupture paved the way for new insights. Front Cardiovasc Med. 2022;9:916616. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 9. | Khanal S, Vijayvergiya R, Singhal M. PCI in a single coronary artery from right aortic sinus: A rare case. Indian Heart J. 2015;67:141-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Sharma S, Pillai GM, Potdar A, Malavia G. Percutaneous Coronary Intervention in Anomalously arising Coronary Arteries. J Assoc Physicians India. 2022;70:11-12. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 11. | Del Buono MG, Montone RA, Camilli M, Carbone S, Narula J, Lavie CJ, Niccoli G, Crea F. Coronary Microvascular Dysfunction Across the Spectrum of Cardiovascular Diseases: JACC State-of-the-Art Review. J Am Coll Cardiol. 2021;78:1352-1371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 149] [Cited by in F6Publishing: 183] [Article Influence: 61.0] [Reference Citation Analysis (0)] |