Published online Feb 26, 2024. doi: 10.4330/wjc.v16.i2.92
Peer-review started: October 19, 2023
First decision: January 6, 2024
Revised: January 11, 2024
Accepted: February 1, 2024
Article in press: February 1, 2024
Published online: February 26, 2024
Spontaneous coronary artery rupture (SCAR) is a rare and life-threatening complication after lung cancer surgery. We present a case of SCAR following left upper lobectomy, successfully managed through emergency thoracotomy and coronary artery ligation.
A 61-year-old male patient underwent left upper lobectomy and mediastinal lymph node dissection for lung cancer. The surgery was performed using single-port video-assisted thoracoscopic surgery, and there were no observed complications during the procedure. However, 19 h after surgery, the patient experienced chest discomfort and subsequently developed severe symptoms, including nausea, vomiting, and a drop in blood pressure. Urgent measures were taken, leading to the diagnosis of SCAR. The patient underwent emergency thoracotomy and coronary artery ligation, successfully stopping the bleeding and stabilizing the condition. Despite postoperative complications, the patient made a successful recovery and was discharged from the hospital.
SCAR is a rare but life-threatening complication following lung cancer surgery. Immediate thoracotomy has been shown to be a life-saving measure, while stenting is not the preferred initial approach.
Core Tip: Spontaneous coronary artery rupture (SCAR) is a rare but life-threatening complication that may arise following lung cancer surgery. Close monitoring of patients for acute chest pain after resection is paramount. Rapid evaluation, timely intervention, and thorough examinations are critical in attaining favorable treatment outcomes. In cases where SCAR is suspected, immediate thoracotomy should be considered as an emergency life-saving procedure, while stent implantation is not the preferred initial approach. Maintaining awareness of SCAR as a potential complication and taking prompt action by thoracic surgeons can significantly enhance patient survival and facilitate recovery.
- Citation: Ruan YD, Han JW. Spontaneous coronary artery rupture after lung cancer surgery: A case report and review of literature. World J Cardiol 2024; 16(2): 92-97
- URL: https://www.wjgnet.com/1949-8462/full/v16/i2/92.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i2.92
Coronary artery rupture (CAR) has various causes, including atherosclerosis, aneurysm, trauma, infection, and vascular anomalies[1-11]. Spontaneous CAR (SCAR) denotes unexplained CAR, with unclear etiology and pathology[12]. Consequently, SCAR has limited literature coverage[8,13-22]. Only two reports discuss coronary bleeding after pulmonary surgery[18,22]. One case involved a 68-year-old man with left circumflex coronary artery bleeding on postoperative day 4, managed successfully through left thoracotomy[22]. The other concerned a 58-year-old man experiencing SCAR 3 mo after surgery; emergency thoracotomy revealed a ruptured left coronary artery ramus branch, and the patient succumbed to it[18].
No reports have documented survival after SCAR within 24 h of lung cancer surgery. This study presents the first such case: A patient with significant pericardial effusion and cardiogenic shock who underwent emergent left thoracotomy, proximal left anterior descending branch ligation, and suturing. As a result, the patient successfully recovered and was discharged without complications.
A 61-year-old Chinese man presented to the thoracic surgery clinic with left-sided chest pain lasting 1 mo.
The patient has had intermittent left-sided chest pain for 1 mo. A nodule was found in the upper lobe of the left lung during the thoracic surgery clinic evaluation, suggesting a possible tumor.
The patient denied any surgeries or comorbidities.
The patient denied any family history of malignant tumors.
On physical examination, the vital signs were as follows: Body temperature, 36.4°C; blood pressure, 135/94 mmHg; heart rate, 79 beats/min; respiratory rate, 20 breaths/min. The patient has no palpable lymph nodes in the neck and supraclavicular region. The chest wall appeared normal, without tenderness. The breath sounds in both lungs were clear, and the heartbeat was regular without any audible murmurs. The patient had normal limb mobility. Digital anal examination was not performed.
Blood chemistry, cardiac enzymes, tumor markers were normal.
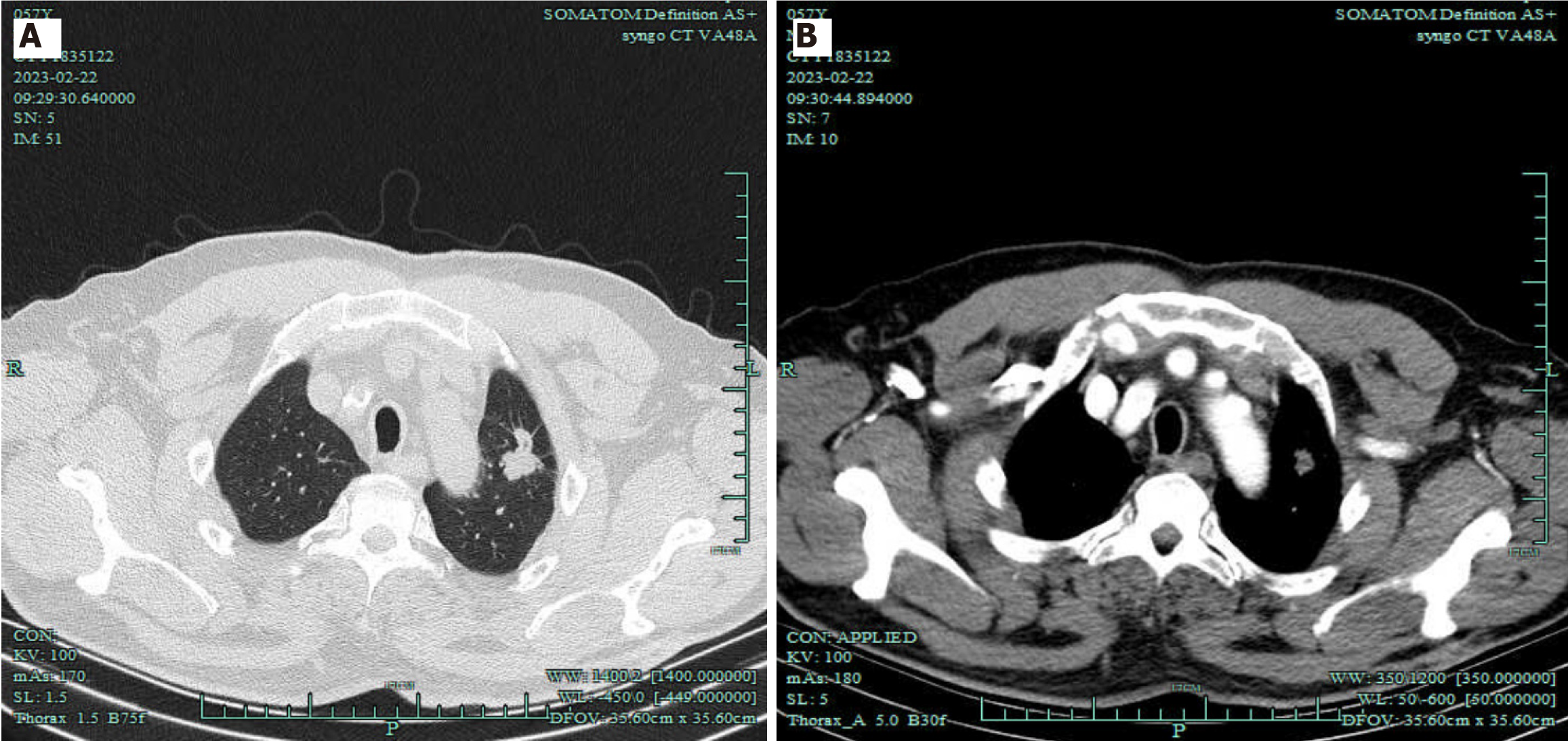
Computed tomography (CT) revealed a 25.4 mm × 19 mm solid nodule in the left lung apex. Electrocardiography (ECG) and 24-h Holter monitoring were normal. Echocardiography found 69.7% left ventricular ejection fraction and no other issues (Figure 1).
Based on the patient’s medical history, the primary diagnosis was malignant lung tumor (adenocarcinoma, sT1bN0M0/IA2). Additionally, the patient was diagnosed with SCAR.
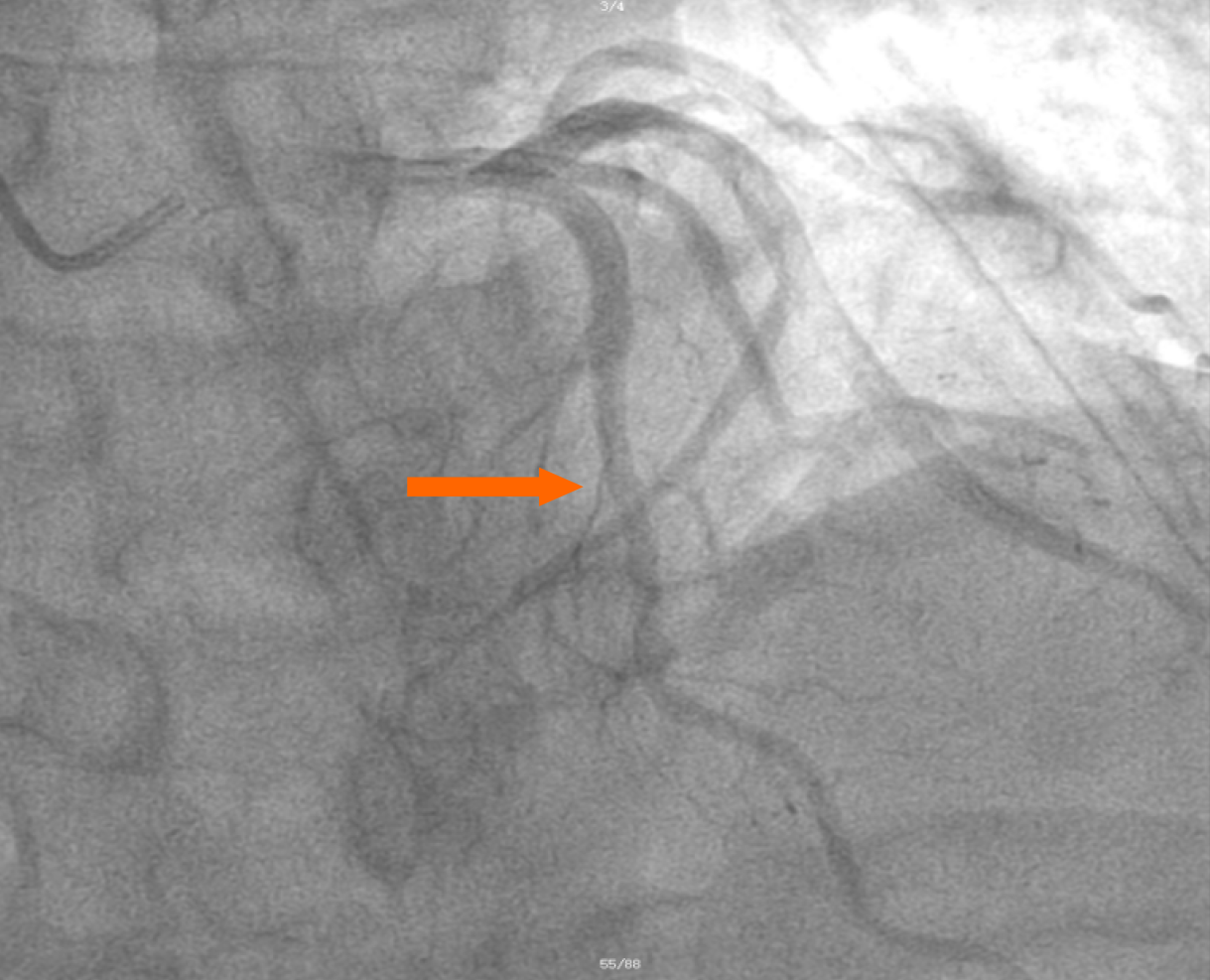
On postoperative day 2, bedside echocardiography indicated no pericardial bleeding or myocardial ischemia, and coronary angiography displayed no issues (Figure 2). The patient experienced postoperative complications, including pulmonary infection, acute renal failure, and gastrointestinal infection. However, with active treatment, the patient successfully recovered and was discharged from the hospital after 10 d.
The patient is still alive and in good health.
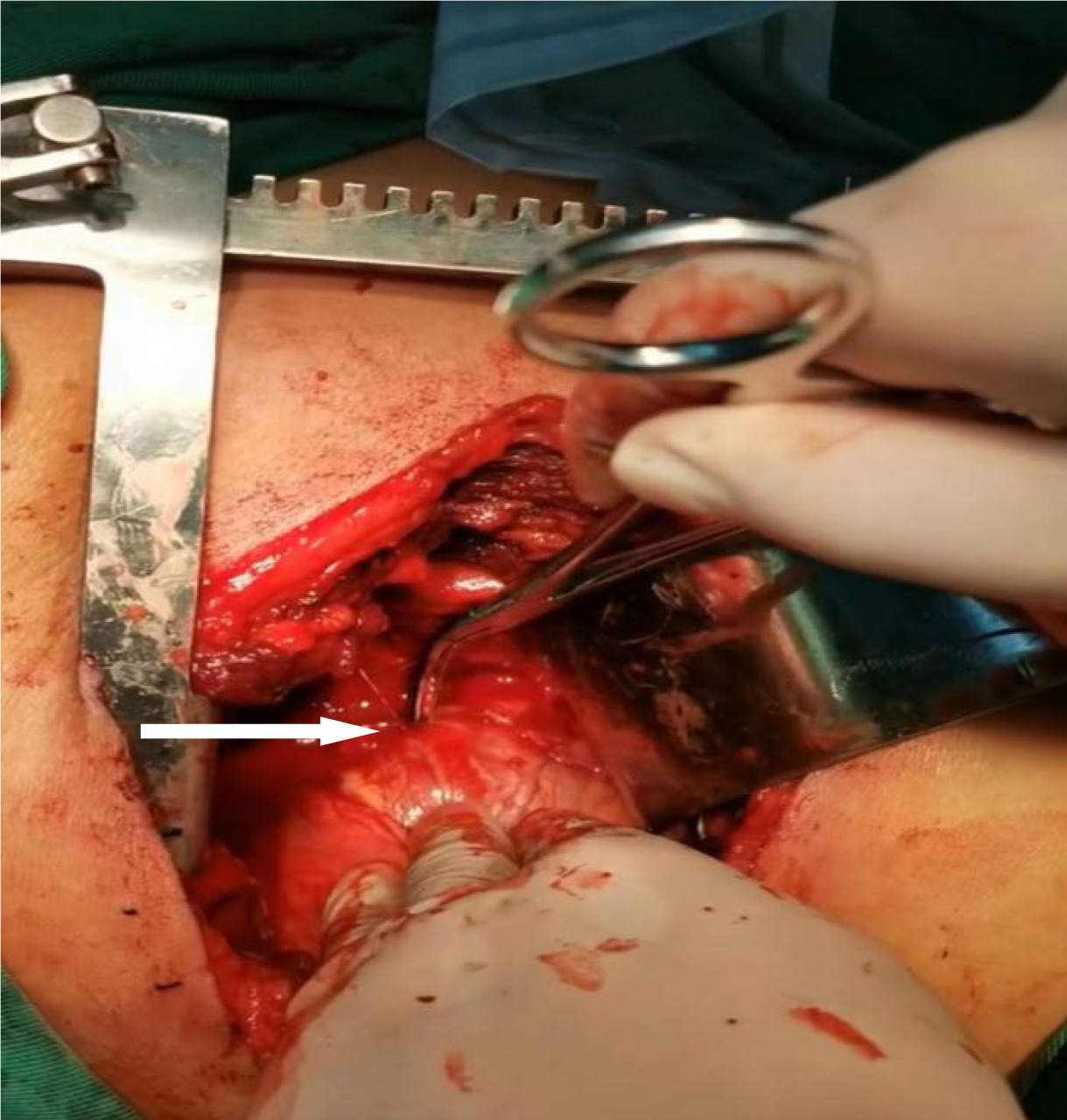
SCAR is a rare life-threatening condition that involves rupture of a normal coronary artery[13]. Symptoms vary based on rupture site; some patients quickly deteriorate due to cardiac tamponade and shock, leading to sudden death[1,13-14]. SCAR occurring within 24 h of video-assisted thoracoscopic left upper lobectomy, followed by successful rescue, is rarer. Our patient recovered and resumed a normal life (Figure 3 and Video).
Cardiac tamponade after lung resection has been documented. Causes include: (1) Residual pulmonary veins retracting into pericardial space, causing intrapericardial hemorrhage[23]; (2) division of aberrant bronchial arteries during surgery, retracting proximal ends into pericardium, causing tamponade[24]; and (3) injury to the ascending aorta during right upper mediastinal lymph node dissection, possibly causing pericardial bleeding[25]. Based on the clinical presentation and relevant examination results, we primarily attributed it to SCAR for the following reasons. Firstly, there was no evidence of coronary heart disease or a family history of the condition in the preoperative examination and medical history. During surgery, we observed no pericardial defects caused by sharp instruments, electrocautery burns, erosion, or local infection. Additionally, postoperative coronary angiography revealed no abnormalities, ruling out the possibility of hemorrhage caused by ruptured atherosclerotic coronary arteries. Since no underlying causes were identified, we consider the CAR to be spontaneous.
Prior research on coronary artery bleeding shows that pressure between the sternum and spine can rapidly raise coronary artery wall pressure. Excessive pressure beyond arterial compliance might trigger rupture[26]. In this case, symptoms like nausea, vomiting, chest discomfort, and hypotension arose 19 h after surgery. Hence, we theorize that the abrupt intrathoracic pressure surge from nausea and vomiting possibly caused SCAR.
Typical SCAR clinical features mimic acute coronary syndrome, aortic dissection, or cardiac tamponade[15,27]. Symptoms vary by rupture site. Left or distal right CAR leads to intrapericardial bleeding, causing tamponade and shock with hypotension, tachycardia, anxiety, altered consciousness, or sudden death. Proximal right CAR often results in subepicardial hematoma but not pericardial bleeding[15,28].
In this case, the patient primarily experienced acute chest pain and hypotension, which align with the acute clinical presentation of SCAR. Therefore, SCAR should be considered as a differential diagnosis for post-pulmonary resection pericardial tamponade.
Common diagnostic methods for CAR include chest X-ray, ECG, echocardiography, and cardiac enzyme profiles. Some cases exhibit abnormal ECG and positive cardiac biomarkers, but most have significant pericardial effusion[19]. Transthoracic echocardiography (TTE) and CT angiography (CTA) are key in diagnosing SCAR. TTE confirms pericardial tamponade post-pericardiocentesis, while CTA excludes aortic dissection and other cardiovascular ruptures[3,15,18]. Rapid SCAR progression and similarity to acute coronary syndrome can lead to overlooked or delayed diagnosis. Selective coronary angiography provides definitive diagnosis, but unstable patients cannot undergo the procedure. Thus, SCAR is often diagnosed during surgery.
Treating SCAR involves factors like bleeding site, severity, patient age and condition, and medical response plan. If angiography pinpoints rupture, stent implantation or coil embolization can manage bleeding[1,3,17,29]. However, as most SCAR patients have tamponade and shock, angiography might not work. Timely identification via TTE and chest CTA is crucial for rapid surgical intervention.
For emergency surgery, selecting the right incision matters. Urgent thoracotomy needs a left anterolateral approach; stable cases use midline sternotomy. Treatments include ligation, suturing, patch repair, and revascularization. Distal artery ruptures can be ligated, causing minor heart damage. Proximal ruptures may lead to extensive infarction and heart failure, so distal revascularization is vital[30].
If the bleeding artery is not found, pericardium or patches can cover, reinforced by medical glue[2,3,19]. Despite the grave outlook of SCAR, many recover well via emergency surgery or intervention[3]. Based on Ellis’ classification[31], this SCAR could be type III, linked to 63% tamponade incidence, requiring thoracotomy, with 19% mortality. Limited data exists on coronary bleeding treatment; some cases used cardiopulmonary bypass (CPB) and cardiac arrest[1,15,19]. Successful surgery removing hematoma, resolving symptoms, absence of severe plaques or artery stenosis permits safe on-beating-heart repair, avoiding the drawbacks of CPB.
Our patient had bedside echocardiography, confirming rising pericardial effusion. Emergency left anterolateral thoracotomy within 2 h revealed the bleeding site, preventing tamponade, and saving the patient’s life.
Although the patient was discharged safely and recovered his health, to date, there is a lack of large-scale research data regarding the treatment of SCAR. Therefore, it is important to determine the most appropriate medical intervention measures definitively.
Although SCRA is rare, it is vital for thoracic surgeons to watch for acute chest pain after lung resection. Monitoring vital signs, timely observation, and comprehensive examination aid rapid, accurate decisions. SCAR should be among post-resection differential diagnosis. If SCAR arises after surgery, immediate thoracotomy boosts survival, and stenting is not preferred initially.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Serafy AS, Egypt S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Butz T, Lamp B, Figura T, Faber L, Esdorn H, Wiemer M, Kleikamp G, Horstkotte D. Images in cardiovascular medicine. Pericardial effusion with beginning cardiac tamponade caused by a spontaneous coronary artery rupture. Circulation. 2007;116:e383-e384. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Kaljusto ML, Koldsland S, Vengen OA, Woldbaek PR, Tønnessen T. Cardiac tamponade caused by acute spontaneous coronary artery rupture. J Card Surg. 2006;21:301-303. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Motoyoshi N, Komatsu T, Moizumi Y, Tabayashi K. Spontaneous rupture of coronary artery. Eur J Cardiothorac Surg. 2002;22:470-471. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Manzo-Silberman S, Aelion H, Leprince P. Spontaneous rupture of a coronary artery. Arch Cardiovasc Dis. 2014;107:704-705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Gunduz H, Akdemir R, Binak E, Tamer A, Uyan C. Spontaneous rupture of a coronary artery aneurysm: a case report and review of the literature. Jpn Heart J. 2004;45:331-336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Dueholm S, Fabrin J. Isolated coronary artery rupture following blunt chest trauma. A case report. Scand J Thorac Cardiovasc Surg. 1986;20:183-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Fan CC, Andersen BR, Sahgal S. Isolated myocardial abscess causing coronary artery rupture and fatal hemopericardium. Arch Pathol Lab Med. 1994;118:1023-1025. [PubMed] [Cited in This Article: ] |
| 8. | Evans RH, Fraser AG. Spontaneous coronary artery rupture and cardiac tamponade in Ehlers-Danlos syndrome type IV. Int J Cardiol. 1996;54:283-286. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Brennan K, Shurmur S, Elhendy A. Coronary artery rupture associated with amphetamine abuse. Cardiol Rev. 2004;12:282-283. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Oshima T, Minatsuki S, Myojo M, Kodera S, Nawata K, Ando J, Akazawa H, Watanabe M, Ono M, Komuro I. Coronary Artery Aneurysm Caused by a Stent Fracture. Int Heart J. 2018;59:203-208. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | De Giorgio F, Abbate A, Capelli A, Arena V. Spontaneous rupture of coronary artery in human immunodeficiency virus-positive patient treated with highly active anti-retroviral therapy (HAART). Am J Forensic Med Pathol. 2005;26:197. [PubMed] [Cited in This Article: ] |
| 12. | Kar S, Webel RR. Diagnosis and treatment of spontaneous coronary artery pseudoaneurysm: Rare anomaly with potentially significant clinical implications. Catheter Cardiovasc Interv. 2017;90:589-597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Moonen ML, Hanssen M, Radermecker MA, Lancellotti P. The blue man: an unusual happy end of a spontaneous rupture of a coronary artery. Eur J Cardiothorac Surg. 2008;34:1265-1267. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | ADAMS CW, EDER G. Spontaneous rupture of the right coronary artery. Am J Cardiol. 1958;1:765-767. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 15. | Longobardi A, Iesu S, Baldi C, Di Maio M, Panza A, Mastrogiovanni G, Masiello P, Itri F, Lambiase C, Bossone E, Piscione F, Di Benedetto G. Spontaneous coronary artery rupture presenting as an acute coronary syndrome evolved in pseudoaneurysm and cardiac tamponade: Case report and literature review. Eur Heart J Acute Cardiovasc Care. 2017;6:666-669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Sayed AI. Case report: Spontaneous coronary artery rupture presenting with acute coronary syndrome: A rare diagnosis of common disease. Front Cardiovasc Med. 2022;9:922180. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 17. | Cheng ST, Liu CJ, Huang HL, Ko YL. Rescue Coilization for Spontaneous Coronary Artery Rupture. JACC Cardiovasc Interv. 2021;14:e149-e150. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 18. | He Z, Chen G, He X. Spontaneous Coronary Artery Rupture Causing Acute Cardiac Tamponade and Cardiogenic Shock. Int Heart J. 2019;60:1009-1012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Shrestha BM, Hamilton-Craig C, Platts D, Clarke A. Spontaneous coronary artery rupture in a young patient: a rare diagnosis for cardiac tamponade. Interact Cardiovasc Thorac Surg. 2009;9:537-539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Fujimoto D, Takami M, Kozuki A, Shite J. A case report of unusual clinical features of a spontaneous coronary artery rupture: pathologic findings in the rupture site. Eur Heart J Case Rep. 2019;3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Liang W, Yue H, Zhang T, Wu Z. Case Report: Hematoma Formation After Spontaneous Coronary Artery Rupture. Front Cardiovasc Med. 2021;8:801005. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Ozawa Y, Ichimura H, Sato T, Matsuzaki K. Cardiac tamponade due to coronary artery rupture after pulmonary resection. Ann Thorac Surg. 2013;96:e97-e99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Tovar EA. Pulmonary resection complicated by abrupt pericardial tamponade. Ann Thorac Surg. 1995;60:1864. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | McLean RH, Parandian BB, Nam MH. Pericardial tamponade: an unusual complication of lobectomy for lung cancer. Ann Thorac Surg. 1999;67:545-546. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Morimoto M, Ohashi M, Nobara H, Fukaya Y, Haniuda M, Iida F. Rupture of the ascending aorta after surgical resection for lung cancer--a case report. Jpn J Surg. 1991;21:476-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Trotter TH, Knott-Craig CJ, Ward KE. Blunt injury rupture of tricuspid valve and right coronary artery. Ann Thorac Surg. 1998;66:1814-1816. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Keskin M, Bozbay M, Kayacıoğlu İ, Koçoğulları C, Bozbay AY, Hayıroğlu Mİ, Gürkan U, Eren M. Spontaneous Right Coronary Artery Rupture and Acute Cardiac Tamponade in Behçet's Disease. Heart Lung Circ. 2016;25:e149-e151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Sevuk U, Ozyalcin S, Ayaz F, Kose K. Spontaneous coronary artery rupture without a pericardial effusion: a diagnostic challenge. BMJ Case Rep. 2016;2016. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Wiemer M, Horstkotte D, Schultheiss HP. [Non-surgical management of a perforated left anterior descending coronary artery following cardiopulmonary resuscitation]. Z Kardiol. 1999;88:675-680. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Wall MJ Jr, Mattox KL, Chen CD, Baldwin JC. Acute management of complex cardiac injuries. J Trauma. 1997;42:905-912. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 79] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 31. | Ellis SG, Ajluni S, Arnold AZ, Popma JJ, Bittl JA, Eigler NL, Cowley MJ, Raymond RE, Safian RD, Whitlow PL. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation. 1994;90:2725-2730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 460] [Cited by in F6Publishing: 430] [Article Influence: 14.3] [Reference Citation Analysis (0)] |