Published online Oct 27, 2016. doi: 10.4240/wjgs.v8.i10.693
Peer-review started: June 1, 2016
First decision: July 20, 2016
Revised: August 4, 2016
Accepted: August 27, 2016
Article in press: August 29, 2016
Published online: October 27, 2016
Processing time: 146 Days and 20.9 Hours
To investigate the epidemiology, treatment and outcomes of acute appendicitis (AA) in a large population study.
This is a retrospective cohort study derived from the administrative dataset of the Bergamo district healthcare system (more than 1 million inhabitants) from 1997 to 2013. Data about treatment, surgery, length of stay were collected. Moreover for each patients were registered data about relapse of appendicitis and hospital admission due to intestinal obstruction.
From 1997 to 2013 in the Bergamo district we collected 16544 cases of AA, with a crude incidence rate of 89/100000 inhabitants per year; mean age was 24.51 ± 16.17, 54.7% were male and the mean Charlson’s comorbidity index was 0.32 ± 0.92. Mortality was < 0.0001%. Appendectomy was performed in 94.7% of the patients and the mean length of stay was 5.08 ± 2.88 d; the cumulative hospital stay was 5.19 ± 3.36 d and 1.2% of patients had at least one further hospitalization due intestinal occlusion. Laparoscopic appendectomy was performed in 48% of cases. Percent of 5.34 the patients were treated conservatively with a mean length of stay of 3.98 ± 3.96 d; the relapse rate was 23.1% and the cumulative hospital stay during the study period was 5.46 ± 6.05 d.
The treatment of acute appendicitis in Northern Italy is slowly changing, with the large diffusion of laparoscopic approach; conservative treatment of non-complicated appendicitis is still a neglected option, but rich of promising results.
Core tip: Acute appendicitis is the most common surgical emergency around the world. In the Bergamo district, northern Italy its incidence is 89/100000 inhabitants per year with a negative trend during the last years. Percent of 95 patients were treated with appendectomy, 48% of whom laparoscopically; 1.3% of operated patients had an intestinal obstruction during the follow-up. Conservative treatment resulted in a reduced length of stay but 23% of patients had a relapse during follow up. Cumulative length of stays during the study period was similar for the two treatment option.
- Citation: Ceresoli M, Zucchi A, Allievi N, Harbi A, Pisano M, Montori G, Heyer A, Nita GE, Ansaloni L, Coccolini F. Acute appendicitis: Epidemiology, treatment and outcomes- analysis of 16544 consecutive cases. World J Gastrointest Surg 2016; 8(10): 693-699
- URL: https://www.wjgnet.com/1948-9366/full/v8/i10/693.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i10.693
Acute appendicitis is probably the most common surgical emergency worldwide. Since its first accurate description by Fitz[1] in 1886 and the first appendectomy performed by Treves[2] in England, appendectomy became the preferred treatment of acute appendicitis. Although appendicitis is a very common disease, nowadays it has a still poorly understood etiology, with a very heterogeneous clinical pattern of presentation, varying from simple uncomplicated appendicitis to generalized peritonitis due to perforation. For each clinical pattern the proposed treatment is the same: Appendectomy. This results in an overtreatment with a described rate of negative appendectomy (a hystopathological diagnosis of normal appendix) ranging from 6% to 20%[3,4]. Appendectomy has also a complication rate ranging from 8% to 11%, depending on the surgical technique[5]. Several reports described spontaneous resolution of uncomplicated appendicitis without the need of an operation and, since the high rate of negative appendectomy and the significative complications rate, some authors proposed and advised conservative management for uncomplicated appendicitis[6,7]. Conservative management for appendicitis has been described in 1930 by the “Ochsen-Sherren delayed[8] treatment”, which consisted of resting and fasting followed by delayed elective appendectomy; nowadays, a conservative approach based on antibiotic therapy is gaining popularity, as documented by several randomized studies and meta-analyses that analyze this peculiar issue[9-17]. Conservative treatment has been shown to be safe and effective as primary treatment compared to surgical treatment with a significative reduction in morbidity, even with a considerable one year recurrence rate of 23%[17].
Despite this positive evidence, great uncertainty and skepticism remain concerning conservative treatment among surgeons.
The aim of the study was to describe the epidemiology of acute appendicitis in a large population study during the last seventeen years in order to analyze the evolution of the treatment throughout the years - appendectomy or conservative treatment, open or laparoscopic surgery - and to study the long term follow up of patients, in order to investigate the relapse rate of acute appendicitis in conservatively-treated patients and the incidence of intestinal occlusion after surgery.
This is a retrospective analysis of patients discharged from the hospital between 1997 and 2013 with a diagnosis of acute appendicitis. Data were extracted from the administrative health care database of Bergamo’s district, a large area (2723 km2) in Northern Italy with 1094062 inhabitants. This database collects all discharge records for each citizen of the district from any hospital, public and private, intra and extra-district. On the basis of this register, patients are assigned to the respective DRG, and reimbursements are supplied to the hospitals from the regional health care system.
Patients were retrieved on the basis of the concomitant presence of an unplanned hospital admission, with a ICD9-CM code of AA (ICD9-CM code 540.X, 541.X, 542.X, 543.X) in the first three diagnostic fields and with an Italian DRG code of Acute Appendicitis.
For each patient tracked, data regarding age, sex, Charlson’s comorbidity index, surgical procedures (ICD9-CM code 47.X), length of hospital stay, time intervals between admission and operation and mortality were recorded.
For each patient further data on hospitalization related to acute appendicitis (same code) and bowel occlusion (ICD9-CM code 560.X) were collected, as well as the number of further hospitalizations, interventions, length of stay of each hospitalization and cumulative length of stay during the study period.
Continuous variables were expressed as mean ± SD and were compared with the Mann-Withney U test; association was tested with the Pearson’s χ2 test. Correlations were calculated with the Pearson’s correlation test. Multivariate analyses were performed with the logistic regression method. Survivals were calculated with the Kaplan Meier method. Statistical analysis was performed with SPSS software (SPSS version 20, IBM, United States). Trends were studied with the Jointpoint model: Joinpoint regression analysis was performed using the Joinpoint software from the Surveillance Research Program of the United States National Cancer Institute (Joinpoint Regression Program, Version 4.1.1 - August 2014; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute). Trends were summarized with Average Annual Percent Change (AAPC). Calendar years started from 1997, until 2013. Crude rates are per 100000 inhabitants.
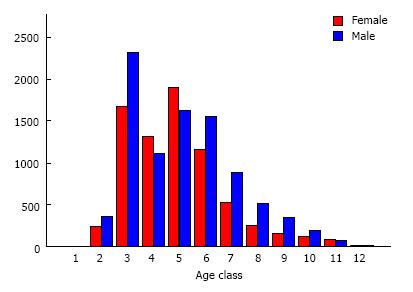
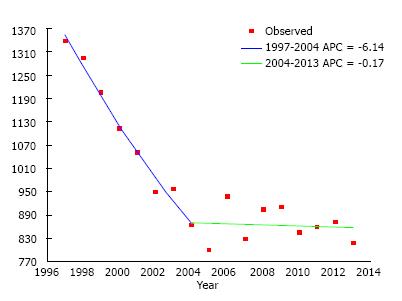
From 1997 to 2013 in the Bergamo district we collected 16544 cases of AA, with a crude incidence rate of 89/100000 per year; mean age was 24.51 ± 16.17, 54.7% were male and mean Charlson comorbidity index was 0.32 ± 0.92. Mortality was recorded for 7 patients (< 0.0001%). Table 1 and Figure 1 show the distribution of age categories and sex: differences among sex in the different age categories were statistically significant (P < 0.001). The incidence of AA decreased during the years starting from 120/105 in 1997 to 73/105 in 2013 with a statistically significant negative value (AAPC = -2.8, P < 0.001) (Figure 2).
| Age category | Sex | Total | ||
| F | M | n | Among total | |
| 0-1 | 1 | 0 | 1 | 0.01% |
| 100.00% | 0.00% | |||
| 1-6 | 239 | 369 | 608 | 3.68% |
| 39.30% | 60.70% | |||
| 7-13 | 1673 | 2322 | 3995 | 24.15% |
| 41.90% | 58.10% | |||
| 14-17 | 1314 | 1119 | 2433 | 14.71% |
| 54.00% | 46.00% | |||
| 18-25 | 1904 | 1628 | 3532 | 21.35% |
| 53.90% | 46.10% | |||
| 26-35 | 1167 | 1556 | 2723 | 16.46% |
| 42.90% | 57.10% | |||
| 36-45 | 529 | 889 | 1418 | 8.57% |
| 37.30% | 62.70% | |||
| 46-55 | 255 | 514 | 769 | 4.65% |
| 33.20% | 66.80% | |||
| 56-65 | 165 | 352 | 517 | 3.13% |
| 31.90% | 68.10% | |||
| 66-75 | 135 | 205 | 340 | 2.06% |
| 39.70% | 60.30% | |||
| 76-85 | 89 | 79 | 168 | 1.02% |
| 53.00% | 47.00% | |||
| > 85 | 23 | 17 | 40 | 0.24% |
| 57.50% | 42.50% | |||
| Total | 7494 | 9050 | 16544 | 100.00% |
| 45.30% | 54.70% | |||
An appendectomy was performed in 94.7% of the patients: Mean age was 24.39 ± 15.98, mean Charlson’s comorbidity index was 0.31 ± 0.90 and 53.1% were male. Patients were operated after a mean of 0.85 ± 1.46 d and the mean length of stay was 5.08 ± 2.88 d with a negative trend over the considered period, starting from 6.09 ± 2.94 in 1997 to 4.58 ± 2.33 in 2013 (AAPC -1.5, P < 0.001). Mortality was < 0.0001%.
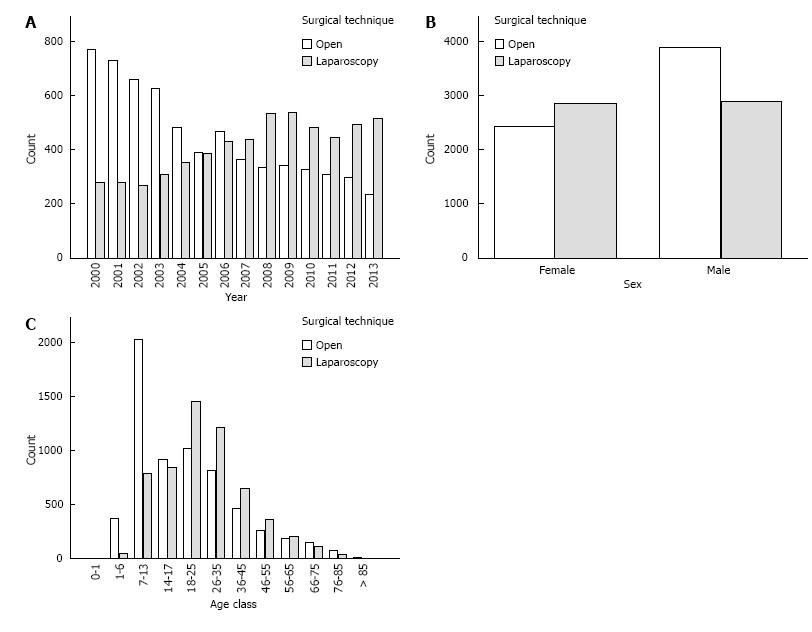
Data about laparoscopic procedures was available only after the year 2000: 48% of the patients were operated with the laparoscopic technique with a positive trend during the years, starting from 26% in 2000 to 68.8% in 2013 (AAPC 5.2, P < 0.001) (Figure 3A) and with a mean length of stay of 4.47 ± 2.66 d (compared to 5.43 ± 2.94 with the open technique, P < 0.001). Laparoscopy was associated with a higher age, female sex and year in both univariate and multivariate analysis (P < 0.0001) (Table 2, Figure 3B and C).
| Open appendectomy | Laparoscopic appendectomy | Total | Univariate analysisP value | Multivariate analysis | ||
| OR | P value | |||||
| n (%) | 6321 (52) | 5734 (48) | 12055 | |||
| Age | 22.79 (17.01) | 27.57 (15.19) | 25.06 (13.55) | < 0.0001 | 1.018 (1.018-1.0121) | < 0.0001 |
| Sex | M: 61.5% | M: 50.2% | M: 54.6% | < 0.0001 | 1.80 (1.66-1.94) | < 0.0001 |
| Charlson's | 0.33 (0.97) | 0.35 (0.87) | 0.34 (0.92) | 0.385 | ||
| Year | 0.277 (Pearson Correlation) | < 0.0001 | 1.15 (1.14-1.16) | < 0.0001 | ||
| Time to surgery (d) | 0.66 (1.35) | 0.97 (1.53) | 0.81 (1.45) | < 0.0001 | ||
| Lenght of stay (d) | 5.28 (3.00) | 4.47 (2.66) | 4.89 (2.85) | < 0.0001 | ||
| Mortality | 5 (0.1%) | 1 (0.001%) | 6 (< 0.0001) | 0.13 | ||
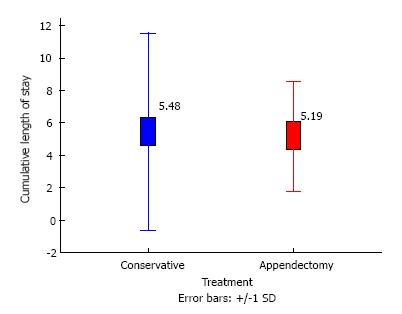
The cumulative hospital stay during study period was 5.19 ± 3.36 d with a mean of 1.01 ± 0.13 hospital admissions. One hundred and ninty-two patients (1.2%) had at least one further hospitalization due intestinal occlusion after a mean of 30.53 ± 41.23 mo (median 11 mo) and 59.9% of them were operated on (Figures 4 and 5).
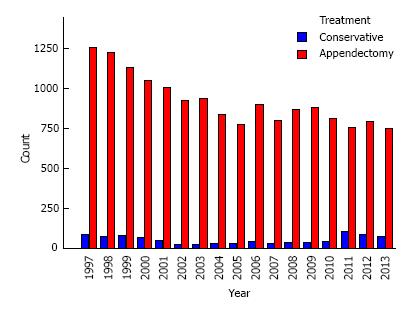
In general, 5.34% of the patients were treated conservatively: Mean age was 26.68 ± 19.04; 56.1% were male and mean Charlson’s comorbidity index was 0.51 ± 1.26; mean length of stay was 3.98 ± 3.96 d; mortality was 0.1%. The proportion of patients treated conservatively increased during the years, from 6.1% in 1997 to 8.7% in 2013, although the trend was not significant (P = 0.6) (Figure 6).
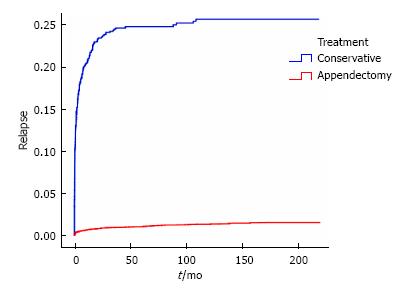
Overall, relapse rate was 23.1% and a new episode of acute appendicitis occurred after a mean of 6.5 ± 15 mo (median 32 d); 89% of patients were operated on at relapse. The mean number of hospital admissions was 1.26 ± 0.47 with a cumulative hospital stay during the study period of 5.46 ± 6.05 d (Figures 4 and 5).
After univariate analysis, conservative treatment was associated with higher age, higher comorbidity index, and year of treatment (P < 0.0001); after multivariate analysis only Carlson’s comorbidity index (P = 0.004) and year of treatment (P < 0.0001) remained significant (Table 3).
| Total | Treatment | Univariate analysis P value | Multivariate analysis | |||
| Appendectomy | Conservative | OR (95%CI) | P value | |||
| n (%) | 16544 | 15661 (94.7) | 883 (5.3) | |||
| Age | 24.51 (16.17) | 24.39 (15.98) | 26.68 (19.04) | < 0.0001 | 1.006 (0.999-1.013) | 0.095 |
| Sex | M: 54.7% | M: 54.6% | M: 56.1% | 0.424 | ||
| Charlson's | 0.32 (0.92) | 0.31 (0.90) | 0.51 (1.26) | < 0.0001 | 0.826 (0.703-0.868) | < 0.0001 |
| Year | -0.33 (Pearson Correlation) | < 0.0001 | 0.973 (0.959-0.986) | < 0.0001 | ||
| Time to surgery (d) | 0.85 (1.46) | |||||
| Length of stay (d) | 5.02 (2.92) | 5.08 (2.88) | 3.98 (3.46) | < 0.0001 | ||
| Mortality | 7 (< 0.0001%) | 6 (< 0.0001%) | 1 (0.1%) | 0.292 | ||
| Relapse | 1.20% | 23.10% | < 0.0001 | |||
| Time to relapse (mo) | Mean | 30 (45) | 6.5 (15) | < 0.0001 | ||
| Time to relapse (mo) | Median | 11 (1.17-49) | 1 (0.16-6.63) | |||
| number of hospitalization | 1.03 (0.18) | 1.01 (0.13) | 1.26 (0.47) | < 0.0001 | ||
| Cumulative LOS | 5.20 (3. 56) | 5.19 (3.36) | 5.47 (6.05) | 0.02 | ||
Acute appendicitis in Northern Italy has a crude rate of 89 cases per 100000 inhabitants per year, and this data is comparable to similar studies in other country worldwide[18-21]. Surprisingly, during the study period the incidence decreased significantly, from 120 to 73 cases per 100000 inhabitants. This data contrasts with the data reported by Buckius et al[20] in the United States over a similar period of time. Acute appendicitis is already a poorly understood disease and its diagnosis is still based on clinical judgment, with great variability among surgeons. Clinical scores have been developed and proposed in the last years to help surgeons reaching a diagnosis of acute appendicitis, such as the Alvarado and the Andersson score[22,23]: The decrease in the incidence rate could be explained by the diffusion of these scores and a consequent increased attention in the diagnosis of acute appendicitis, in order to reduce the rate of negative appendectomies. As expected, acute appendicitis is more frequent in young and male patients (Figure 1), as reported by the literature[18-20], with augmented incidence among patients in the 7-25 years categories. In the years categories 14-25, acute appendicitis is more frequent in females: A possible reason is the starting of childbearing ages and the sexual transmitted disorders that could mime acute appendicitis - with lower quadrant abdominal pain - and a consequent higher rate of negative appendectomies, as reported by Seetahal et al[3]. Unfortunately there are no data available on the rate of negative appendectomies to confirm this hypothesis. The possibility of a diagnosis other than appendicitis in women justifies the higher frequency in this subgroup of the laparoscopic technique, which give the possibility to thoroughly explore the peritoneal cavity, as shown in Figure 3B. Laparoscopic appendectomy was performed in 48% of the cases, with an enormous increase across the years, from 26% to 69% (Figure 3). This data demonstrates the gradual diffusion of the laparoscopic technique, as shown by a similar study in the same contest for acute cholecystitis[24]. After multivariate analysis, the laparoscopic approach was correlated to the year of treatment, female sex and older age: Figure 3C demonstrates that open appendectomy is still the preferred technique for children.
Conservative treatment for acute appendicitis in Northern Italy is still a neglected option, with only 5% of patients treated not operatively; however, over the period of study there was a small increase in the proportion of patients treated conservatively. Despite the small number, conservative treatment seems to be an effective treatment option, showing a reduced length of stay and, notwithstanding an overall relapse rate of 23%, a similar cumulated length of stay and number of hospital admissions during the study period, with a clinically not significant difference (Figure 4). Conservative treatment, as shown in Figure 5, fails after a median of 32 d and leads to an operative treatment in the majority of cases. Factors involved in the choice of this approach are represented by the comorbidities of the patient and the year of treatment, showing that this option is slowly spreading, but still depends on the surgeon’s preference. Conservative treatment resulted in 77% reduction of surgical procedures for appendicitis during the study period, maintaining a similar length of stay; moreover, appendectomy exposes patients to the risk of intestinal obstruction due to adherences in 0.7%-10.7%[25-27]: In our group of patients, 1.3% of the patients needed a further hospitalization due to bowel obstruction after a median of 11 mo and required a further surgical operation in 60% of cases. Laparoscopic appendectomy has been shown to reduce the risk of intestinal obstruction[28] and our results confirm this evidence, although the clinical effect is not significant (Table 2). A cost-effectiveness study demonstrated that conservative treatment, with a failure rate of less than 40% is more cost effective than operative management: Our results on a large population study during a long period show that treating a patient with acute appendicitis conservatively could be considered the better treatment option.
The study was performed retrieving data from an administrative register that allows for a long-term follow up for each patient included; unfortunately, administrative registries do not include data about histopathological diagnosis. Moreover, figures about failure of conservative treatment could be slightly underestimated, considering the lack of data about the immediate failure during the first hospital admission.
In conclusion the treatment of acute appendicitis in Northern Italy is slowly changing, with the large diffusion of laparoscopic approach; conservative treatment of non-complicated appendicitis is still a neglected option, but full of promising results.
Acute appendicitis is the commonest surgical emergency. Despite appendectomy is considered the definitive treatment there is great interest in the conservative management.
Epidemiology and treatment of acute appendicitis.
The study outlines the current epidemiology of acute appendicitis giving an overview on the state of the art of the treatment’s choice in the daily clinical practice.
The study gives the state of the art of the treatment of acute appendicitis and its changes during the last years.
Conservative treatment: Medical therapy based on antibiotics administration.
This is a well-written article with good statistical analysis.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Handra-Luca A, Papes D S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Fitz RH. Perforating inflammation of the vermiform appendix with special reference to its early diagnosis and treatment. Am J Med Sci. 1886;92:321-246. [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Treves F. The Cavendish lecture on some phases of inflammation of the appendix: Delivered before the West London Medico-Chirurgical Society on June 20th, 1902. Br Med J. 1902;1:1589-1594. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W, Cornwell EE, Chang DC, Siram SM. Negative appendectomy: a 10-year review of a nationally representative sample. Am J Surg. 2011;201:433-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 4. | Bhangu A, Søreide K, Saverio S Di, Hansson Assarsson J, Drake FT. Emergency surgery 1 Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 535] [Cited by in F6Publishing: 633] [Article Influence: 70.3] [Reference Citation Analysis (0)] |
| 5. | Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, Pietrobon R. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004;239:43-52. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 327] [Cited by in F6Publishing: 341] [Article Influence: 17.1] [Reference Citation Analysis (1)] |
| 6. | Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect (Larchmt). 2008;9:481-488. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Coccolini F, Pisano M, Magnone S, Colaianni N, Campanati L, Catena F, Ansaloni L. Antibiotics as first-line therapy for acute appendicitis: evidence for a change in clinical practice. World J Surg. 2012;36:2952-2953. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Bailey H. The ochsner-sherren (delayed) treatment of acute appendicitis: indications and technique. Br Med J. 1930;1:140-143. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Ansaloni L, Catena F, Coccolini F, Ercolani G, Gazzotti F, Pasqualini E, Pinna AD. Surgery versus conservative antibiotic treatment in acute appendicitis: a systematic review and meta-analysis of randomized controlled trials. Dig Surg. 2011;28:210-221. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 10. | Paajanen H, Grönroos JM, Rautio T, Nordström P, Aarnio M, Rantanen T, Hurme S, Dean K, Jartti A, Mecklin JP. A prospective randomized controlled multicenter trial comparing antibiotic therapy with appendectomy in the treatment of uncomplicated acute appendicitis (APPAC trial). BMC Surg. 2013;13:3. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Imha W, Denm DH, Dc DV, Hmj J. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Collab. 2011;11:CD008359. [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, Tuominen R, Hurme S, Virtanen J, Mecklin JP. Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis: The APPAC Randomized Clinical Trial. JAMA. 2015;313:2340-2348. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 502] [Cited by in F6Publishing: 508] [Article Influence: 56.4] [Reference Citation Analysis (0)] |
| 13. | Solomon CG, Flum DR. Clinical practice. Acute appendicitis--appendectomy or the “antibiotics first” strategy. N Engl J Med. 2015;372:1937-1943. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 123] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 14. | Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156-e2156. [DOI] [Cited in This Article: ] [Cited by in Crossref: 256] [Cited by in F6Publishing: 250] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 15. | Liu K, Fogg L. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and meta-analysis. Surgery. 2011;150:673-683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 98] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 16. | Rocha LL, Rossi FM, Pessoa CM, Campos FN, Pires CE, Steinman M. Antibiotics alone versus appendectomy to treat uncomplicated acute appendicitis in adults: what do meta-analyses say? World J Emerg Surg. 2015;10:51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, Agoritsas T, Heels-Ansdell D, Guyatt GH, Tikkinen KA. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016; Mar 17; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 133] [Cited by in F6Publishing: 174] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 18. | Lin KB, Lai KR, Yang NP, Chan CL, Liu YH, Pan RH, Huang CH. Epidemiology and socioeconomic features of appendicitis in Taiwan: a 12-year population-based study. World J Emerg Surg. 2015;10:42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Addiss DG, Shaffer N, Fowler BS, Tauxe R V. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-925. [Cited in This Article: ] |
| 20. | Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012;175:185-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 186] [Cited by in F6Publishing: 161] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 21. | Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010;20:97-105. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 114] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 22. | Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15:557-564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 838] [Cited by in F6Publishing: 769] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 23. | Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008;32:1843-1849. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 219] [Cited by in F6Publishing: 207] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 24. | Ceresoli M, Zucchi A, Pisano M, Allegri A, Bertoli P, Coccolini F, Falcone C, Manfredi R, Montori G, Nita G. Epidemiology of acute cholecystitis and its treatment in Bergamo District, Northern Italy. Minerva Chir. 2016;71:106-113. [PubMed] [Cited in This Article: ] |
| 25. | Zbar RI, Crede WB, McKhann CF, Jekel JF. The postoperative incidence of small bowel obstruction following standard, open appendectomy and cholecystectomy: a six-year retrospective cohort study at Yale-New Haven Hospital. Conn Med. 1993;57:123-127. [PubMed] [Cited in This Article: ] |
| 26. | Riber C, Søe K, Jørgensen T, Tønnesen H. Intestinal obstruction after appendectomy. Scand J Gastroenterol. 1997;32:1125-1128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Tsao KJ, St Peter SD, Valusek PA, Keckler SJ, Sharp S, Holcomb GW, Snyder CL, Ostlie DJ. Adhesive small bowel obstruction after appendectomy in children: comparison between the laparoscopic and open approach. J Pediatr Surg. 2007;42:939-942; discussion 942. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 28. | Markar SR, Penna M, Harris A. Laparoscopic approach to appendectomy reduces the incidence of short- and long-term post-operative bowel obstruction: systematic review and pooled analysis. J Gastrointest Surg. 2014;18:1683-1692. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |