Published online May 27, 2015. doi: 10.4240/wjgs.v7.i5.82
Peer-review started: November 3, 2014
First decision: December 12, 2014
Revised: January 2, 2015
Accepted: April 10, 2015
Article in press: April 14, 2015
Published online: May 27, 2015
Pseudocyst formation is a common complication of acute and chronic pancreatitis. Most common site of pseudocyst is lesser sac; mediastinal extension of pseudocyst is rare. Other possibilities of posterior mediastinal cyst must be considered. This patient presented with computed tomography abdomen with thorax showing a large thoraco-abdominal pseudocyst with right sided pleural effusion. It was confirmed to be pancreatic pseudocyst by analyzing fluid for amylase and lipase during surgery. In our patient, the pseudocyst was accessible transabdominaly. Cystogastrostomy was not possible as it was causing twisting of cardio-esophageal junction; we did retrocolic and retrogastric Roux-en-Y cystojejunostomy. Only two such cases were reported in literature.
Core tip: Thoraco-abdominal pseudocyst is rare location of pancreatic pseudocyst. Other possibilities of posterior mediastinal cyst must be considered. Internal drainage is a definitive management but will be difficult. Retrocolic retrogastric Roux-en-Y cystojejunostomy is feasible option. Only two such cases were reported in literature.
- Citation: Kamble RS, Gupta R, Gupta AR, Kothari PR, Dikshit KV, Kekre GA, Patil PS. Thoracoabdominal pseudocyst of pancreas: An rare location, managed by retrocolic retrogastric Roux-en-Y cystojejunostomy. World J Gastrointest Surg 2015; 7(5): 82-85
- URL: https://www.wjgnet.com/1948-9366/full/v7/i5/82.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i5.82
Posterior mediastinal cysts can be foregut duplication cyst, pancreatic pseudocyst, lymphatic malformation, cystic teratoma, and cystic neuroblastoma. Pseudocyst formation is a common complication of acute and chronic pancreaitis. Mostly pseudocyst occurs in lesser sac or peripancreatic region. Mediastinal extension of pseudocyst is rare.
We report this case of rare location of pseudocyst i.e., thoraco-abdominal without any ductal communication. About 50 cases of mediastinal pseudocyst has been reported in literature[1]. In our patient, the pseudocyst was accessible from transabdominaly. Cystogastrostomy was not possible as it was causing twisting of cardio-esophageal junction; we did retrocolic retrogastric Roux-en-Y cystojejunostomy.
A 10-year-old girl was referred from peripheral center. She was investigated there for dull aching pain in epigastrium, which was for 3 to 4 mo, and pain on right side of chest. She had undergone a computed tomography (CT) scan abdomen and thorax there, which shows 7.3 cm × 4.6 cm × 4.1 cm large loculated collection in posterior mediastinum, right paravertebral region, extending through esophageal hiatus abutting the posterior surface of Right atrium, Inferior vena cava, causing displacement of esophagus. Pancreas was smaller and duct was dilated without any obvious ductal communication (Figures 1 and 2). Patient has also right sided moderate pleural effusion on chest X-ray. She was treated conservatively there. Pleural fluid study was normal, fluid amylase and lipase were within normal limit. Patient referred to us after 2 mo for recurrent abdominal pain. Hematological investigations were normal. Serum amylase and lipase were within normal limit. As possibility of esophageal duplication cyst can’t be ruled out we did barium swallow study which revealed lesion is indenting lower esophagus (Figure 3). Ultrasonography showed similar findings about paraesophageal collection, and right sided mild pleural collection. We did magnetic resonance cholangiopancreatography (MRCP), which showed mild dilatation of multiple side branches of pancreatic duct in tail region without any peripancreatic collection with features of resolving pancreatitis and large loculated collection in right paravertebral region, with a tail extending down (Figure 4).
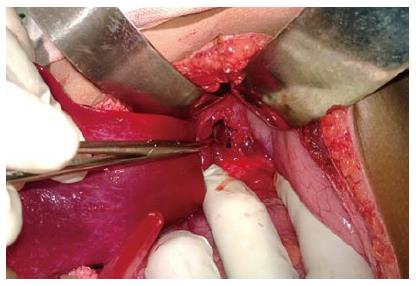
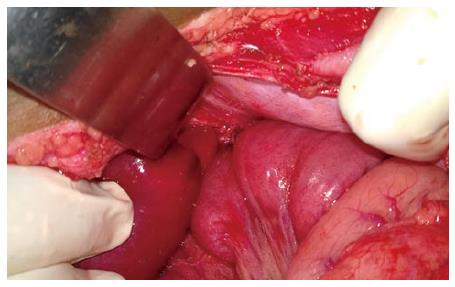
As the radiological investigations didn’t demonstrate definitive communication with pancrease or esophagus, nature of cyst could not be confirmed. Hence exploratory laparotomy followed by sos procedure was planed. After optimization, patient is posted for exploratory laparotomy. On exploration, there was no collection in lesser sac or peripancreatic region. Pancreas was firm on palpation. Dissection was done at the esophageal hiatus. On deep palpation, we felt a fluid filled structure at hiatus, structure delineated, cardio-esophageal junction formed one of the cyst walls and fluid was aspirated. Aspirate fluid was deep amber colored and sent for analysis intraoperative, (fluid amylase-1735 somogyi U, fluid lipase-101436 IU). So it was confirmed to be a pancreatic pseudocyst. A 2 cm × 2 cm cyst wall was cut (Figure 5). Then we had two option either gastrocystostomy or jejunocystostomy. We thought of doing gastrocystostomy but it was not possible as it was causing twisting of cardio-esophageal junction. Hence decided to do cystojejunostomy. Roux-en-Y loop of jejunum brought retrocolic and retrogastric up to the cyst and cystojejunostomy done (Figure 6). Cyst wall biopsy was suggestive of pseudocyst of pancreas without any evidence of malignancy. Patient was given somatostatin perioperative period. Post op recovery was uneventful, pleural effusion resolved in 15 d. Patient is on pancreatic enzymes supplementation and is asymptomatic, in regular follow up.
Posterior mediastinal cysts can be foregut duplication cyst, pancreatic pseudocyst, lymphatic malformation, cystic teratoma, and cystic neuroblastoma.
Pseudocyst formation is a common complication of acute and chronic pancreatitis. Common site of pseudocyst are lesser sac and peripancreatic region. Thoracic/ mediastinal extension of pseudocyst is a rare. About 50 cases have been reported in literature of mediastinal extension[1]. Mediastinal pancreatic pseudocyst was first described in 1951[2]. In acute pancreatitis, fluid gets collected and due to inflammatory process, it gets walled up with granulation tissue and connective tissue. Pancreatic fluid in retroperitoneal space tracts into mediastinal space through aortic, esophageal hiatus and forms mediastinal, thoraco-abdominal pseudocyst. In our patient, it was a thoraco-abdominal. Most of such patients have pleural effusion. Ectopic pancreatic tissue with formation of pseudocyst is also reported in literature[3].
The most common causes of pseudocyst in children are trauma and infection, other causes are congenital anomalies, drug induced[4]. Anomalous pancreatic duct, anomalous pancreaticobiliary junction, pancreatic divisum, annular pancrease causes recurrent pancreatitis.
Symptoms are mainly due to compression or invasion of adjacent structures by pseudocyst, i.e., chest or abdominal pain, dysphagia, dyspnea, pseudo achalasia, weight loss[1,5].
In absence of any peripancreatic collection/communication, these cysts are difficult to say as a pseudocyst of pancrease. Chest X-ray is not diagnostic but can show pleural effusion. For diagnosis CT is better than Ultrasonography, and MRCP is necessary for ductal anatomy. Endoscopic ultrasound gives more information about pancreas and duct if any communication. Endoscopic ultrasound guided aspiration of fluid and fluid analyses will the definitive diagnostic measure[6].
In all patients primary management of pancreatitis, stabilization of patient is must. Spontaneous resolution pseudocyst occurs in about 50% of case and complications can occur in 5%-40% cases[7]. If any ductal obstruction or communication with cyst is there it should be managed first with ERCP stenting. Surgical options available for management of pseudocyst are internal/external drainage. Internal drainage includes cystogastrostomy, Roux-en-Y cystojejunostomy (open/laparoscopic/endoscopic). For Mediastinal pseudocyst these options are not available. A newer technique of endoscopic transmural stenting is reported with variable success rate[7,8]. Endoscopic/thoracoscopic aspiration of pseudocyst is also reported[8]. Endoscopic ultrasound is now increasingly being used for transmural endoscopic drainage. Cysto-gastrostomy for complex mediastinal cyst was reported by Sadat et al[9].
Only two cases of transdiaphragmatic Roux-en-Y cysto-jejunostomy in adult for mediastinal pseudocyst were reported in literature[10,11]. Kotsis et al[10] used thoraco- abdominal approach.
In our patient the nature and etiology of cyst could not be confirmed preoperatively by radiological investigation. Due to presence of major vessels near the cyst and thoraco-abdominal extension of cyst, radiologist could not get a safe window for percutaneous needle aspiration. Endoscopic ultrasound or endoscopic needle aspiration might be helpful, but as such facility was not available at our hospital, diagnostic laparotomy was decided.
On exploration the diagnosis of pseudocyst of pancrease was confirmed. Though the major part was intrathoracic lower part of the cyst in accessible through abdomen. Abdominal part was the most dependent part and cystojejunostomy with Roux-en-Y loop was feasible.
We report this case of rare location of pseudocyst of pancrease, i.e., thoraco-abdominal in 10 years girl managed successfully with retrocolic retrogastric Roux-en-Y cystojejunostomy.
Ten years female child had dull aching pain in epigastrium for 3-4 mo.
Patient had dull aching pain in abdomen, per abdominal examination was normal and had decreased air entry on right side.
Pseudocyst of pancrease, esophageal duplication.
Hematological investigations, serum amylase and lipase were within normal limit. intraoperative fluid analysis- fluid amylase-1735 somogyi U, fluid lipase-101436 IU.
Computed tomography suggested 7.3 cm × 4.6 cm × 4.1 cm size collection in posterior mediastinum, extending through esophageal hiatus likely to be pseudocyst of pancrease or esophageal duplication.
Cyst wall biopsy was suggestive of pseudocyst of pancreas without any evidence of malignancy.
Patient undergone surgery-exploratory laparotomy with retrocolic retrogastric Roux-en-Y cystojejunostomy and postoperative patient is on pancreatic enzymes supplementation.
Only two cases of transdiaphragmatic Roux-en-Y cysto-jejunostomy in adult for mediastinal pseudocyst were reported in literature, Kotsis et al used thoraco- abdominal approach.
Retrocolic retrogastric Roux-en-Y cystojejunostomy is measure to treat thoraco-abdominal pseudocyst.
In the patient the though the major part was intrathorasic lower part of the cyst in accessible through abdomen and retrocolic retrogastric cystojejunostomy with Roux-en-Y loop was feasible.
The author reported a case who had a pseudocyst locating retoroperitoneo-retormediastinal space and managed by retrocolic retrogastric Roux-en-Y cystojejunostomy. The manuscript is very interesting.
P- Reviewer: Iso Y, Klinge U, Mizuguchi T S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Rose EA, Haider M, Yang SK, Telmos AJ. Mediastinal extension of a pancreatic pseudocyst. Am J Gastroenterol. 2000;95:3638-3639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Topa L, László F, Sahin P, Pozsár J. Endoscopic transgastric drainage of a pancreatic pseudocyst with mediastinal and cervical extensions. Gastrointest Endosc. 2006;64:460-463. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Gong N, Fang G. Ectopic pancreas in within thorax: two case reports. Chin J Thorac Cardiovasc Surg. 1997;13:308. [Cited in This Article: ] |
| 4. | Uretsky G, Goldschmiedt M, James K. Childhood pancreatitis. Am Fam Physician. 1999;59:2507-2512. [PubMed] [Cited in This Article: ] |
| 5. | Chettupuzha AP, Harikumar R, Kumar SK, Thomas V, Devi SR. Pancreatic pseudocyst presenting as odynophagia. Indian J Gastroenterol. 2004;23:27-28. [PubMed] [Cited in This Article: ] |
| 6. | Groeneveld JH, Tjong A Lieng JG, de Meijer PH. Resolution of a complex mediastinal pseudocyst in a patient with alcohol-related chronic pancreatitis following abstinence from alcohol. Eur J Gastroenterol Hepatol. 2006;18:111-113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Vitas GJ, Sarr MG. Selected management of pancreatic pseudocysts: operative versus expectant management. Surgery. 1992;111:123-130. [PubMed] [Cited in This Article: ] |
| 8. | Beauchamp RD, Winsett M, Nealon WH. Operative strategies in the management of mediastinal pancreatic pseudocyst. Surgery. 1989;106:567-570. [PubMed] [Cited in This Article: ] |
| 9. | Sadat U, Jah A, Huguet E. Mediastinal extension of a complicated pancreatic pseudocyst; a case report and literature review. J Med Case Rep. 2007;1:12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Kotsis L, Agócs L, Kostic S, Vadász P. Transdiaphragmatic cyst-jejunostomy with Roux-en-Y loop for an exclusively mediastinal pancreatic pseudocyst. Scand J Thorac Cardiovasc Surg. 1996;30:181-183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Baker CR, Gossage JA, Mason RC. An unusual cause of dysphagia: transabdominal Roux-en-Y cyst-jejunostomy in the surgical management of a symptomatic mediastinal cyst. J Surg Case Rep. 2013;2013. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |