Published online Nov 27, 2013. doi: 10.4240/wjgs.v5.i11.309
Revised: November 23, 2012
Accepted: December 20, 2012
Published online: November 27, 2013
Malignant pheochromocytoma accounts for approximately 10% of pheochromocytoma cases. The main site of distant metastasis is the liver. Hypertensive crisis due to catecholamine oversecretion is potentially fatal. We present a case of malignant pheochromocytoma with multiple liver metastases. A 60-year-old female with repeated hypertensive episodes was diagnosed with malignant pheochromocytoma. She underwent a left adrenalectomy and partial hepatectomy with resection of segment 6. Catecholamine levels remained high after surgery and she received repeated cycles of chemotherapy. Four months after surgery, multiple liver metastases were detected. In spite of ongoing chemotherapy, catecholamine levels eventually became uncontrollable. Serum and urine noradrenaline and vanillylmandelic acid levels increased, but adrenaline and dopamine levels stayed within the normal range. Preoperative liver imaging revealed multiple metastases in all segments except segment 4. Percutaneous transhepatic portal vein embolization (PTPE) of the right and lateral branches of the portal vein was performed. The functional liver volume of segment 4 increased after PTPE. Right hepatectomy, lateral segmentectomy and partial resection of segment 1 were performed 10 mo after the initial surgery. Intraoperative ultrasonography detected two small tumors in segment 4, which were treated with intraoperative microwave coagulation therapy. Noradrenaline levels normalized immediately after the second hepatectomy. As there was increased telomerase activity in the resected specimen, she received adjuvant chemotherapy. She remained in good health for 2 years. However, further metastases eventually occurred and she subsequently died due to a brain hemorrhage. Hepatectomy may be a therapeutic option for reduction of tumor mass in pheochromocytoma with liver metastases.
- Citation: Hori T, Yamagiwa K, Hayashi T, Yagi S, Iida T, Taniguchi K, Kawarada Y, Uemoto S. Malignant pheochromocytoma: Hepatectomy for liver metastases. World Journal of Gastrointestinal Surgery 2013; 5(11): 309-313
- URL: https://www.wjgnet.com/1948-9366/full/v5/i11/309.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i11.309
Pheochromocytoma is an endocrine tumor. Malignant pheochromocytoma is diagnosed if a distant metastasis is detected, which occurs in approximately 10% of cases. Hence, pheochromocytoma is commonly called a “10% disease”. Hypertension due to the oversecretion of catecholamines may be fatal[1,2]. The main site of distant metastasis is the liver. We present a case of malignant pheochromocytoma treated by hepatectomy to reduce tumor mass. To our knowledge, this is the first case of aggressive hepatectomy for liver metastases requiring preoperative percutaneous transhepatic portal vein embolization (PTPE).
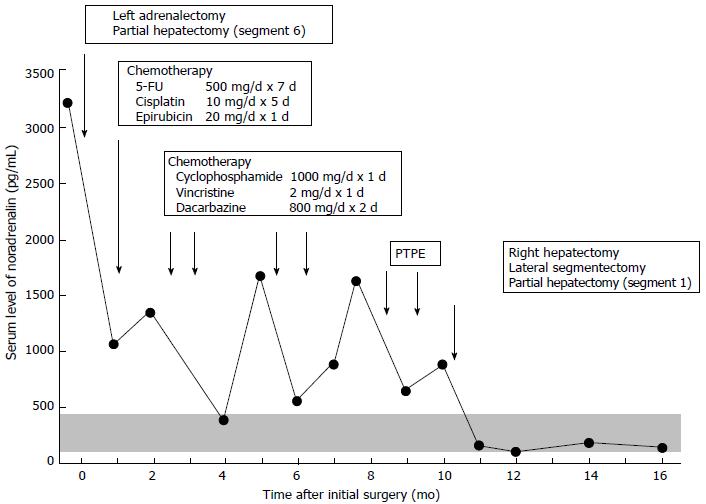
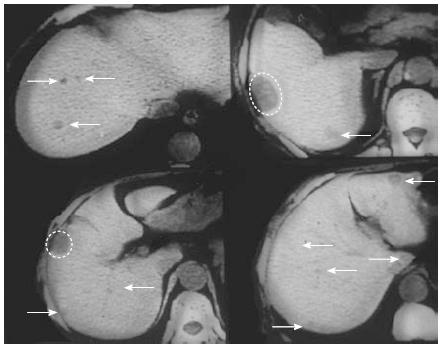
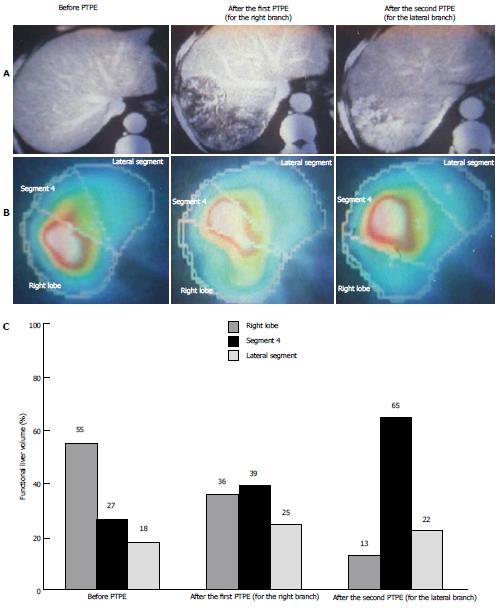
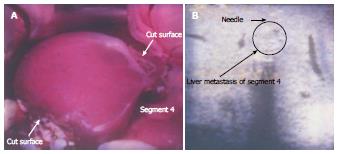
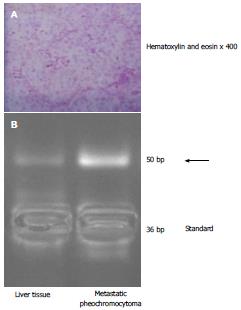
A 60-year-old female with repeated hypertensive episodes was diagnosed with malignant pheochromocytoma. She underwent a left adrenalectomy and partial hepatectomy with resection of segment 6. Since her catecholamine levels stayed high after surgery, she received repeated cycles of chemotherapy (5-FU, cisplatin and epirubicin, followed by cyclophosphamide, vincristine and dacarbazine) (Figure 1). Four months later, multiple liver metastases were detected (Figure 2). Even with ongoing cycles of chemotherapy (cyclophosphamide, vincristine and dacarbazine), catecholamine levels eventually became uncontrollable. She was admitted to our institution for surgical therapy. Angio-computed tomography and magnetic resonance imaging findings were consistent with liver metastases, with the tumors showing uptake on meta-iodobenzylguanidine scintigraphy. Serum and urine levels of noradrenaline and vanillylmandelic acid increased, but adrenaline and dopamine levels stayed within the normal range. As preoperative imaging studies revealed multiple metastases in all liver segments except segment 4, PTPE of the right and lateral branches of the portal vein was performed. The functional liver volume of segment 4 increased after PTPE (Figure 3). She underwent a right hepatectomy with lateral segmentectomy and partial resection of segment 1 (Spiegel lobe) at 10 mo after her initial surgery (Figure 4A). Intraoperative ultrasonography detected two small nodules in segment 4, which were treated with intraoperative microwave coagulation therapy (Figure 4B). Intraoperative examination did not detect tumor in the right adrenal gland. Histopathological examination of the surgical specimens was consistent with pheochromocytoma (Figure 5A). The patient’s noradrenaline level normalized immediately after the second operation. Telomerase activity in the resected tumor, measured by a modified telomeric repeat amplification protocol, was clearly elevated (Figure 5B). She received adjuvant chemotherapy (5-FU, cisplatin and epirubicin) and was able to return to her normal physical and social activities. She remained in good health for 2 years after the second operation. However, she eventually developed further distant metastases. The metastatic tumors enlarged and catecholamine levels increased in spite of ongoing cycles of chemotherapy (cyclophosphamide, vincristine and dacarbazine). She finally died due to a brain hemorrhage triggered by a hypertensive crisis 3 years after the second operation.
Pheochromocytoma is an endocrine tumor arising from the chromaffin cells of the adrenal medulla[1]. Distant metastasis occurs in approximately 10% of cases, resulting in a diagnosis of malignant pheochromocytoma. It is important to consider the possibility of malignant disease even if imaging only detects a primary tumor, but it is difficult to predict malignant potential[3,4]. A previous report documented that the expression of telomerase activity clearly suggests malignant behavior of the component cells[3]. We speculate that analysis of telomerase activity in the biopsy or resected specimens may predict the disease course and may be useful for deciding therapeutic strategies, including surgical procedures and postoperative therapy. We understand that liver metastasis should be considered as the systemic disease. We speculate that more aggressive adjuvant chemotherapy will be required in cases with increased telomerase activity, even in the pheochromocytoma without distant metastasis.
Pheochromocytoma may lead to a fatal hypertensive crisis during anesthesia and other stresses[5]. Surgery to resect tumors can cause unexpected oversecretion of catecholamines and severely raise systolic blood pressure[2,5,6], and it is important to try to avoid such hypertension. In our institution, the drainage vein (i.e., the adrenal vein) is ligated as soon as possible during surgery, followed by ligation of the adrenal artery. We suggest that this isolation technique is useful for the prevention of hypertension and in this case, systolic blood pressure stayed less than 200 mmHg.
Close follow-up is crucial for adequate induction of additional therapies after surgery[2,3]. In our institution, catecholamine levels are checked monthly and image studies are scheduled every three months. In this case, we followed this patient more closely, based on the expression of telomerase activity. Malignant potential based on the expression of telomerase activity may be informative for the follow-up schedule in each case.
The fatal manifestation of pheochromocytoma is hypertension due to the oversecretion of catecholamines[1,2]. Current therapies for pheochromocytoma and close long-term follow-up can result in good survival rates[6-8], even although patients with recurrence eventually die due to hypertensive crisis. The liver is the most common site of pheochromocytoma metastasis. Safe techniques for extended hepatectomy and preoperative PTPE are well established. Hepatectomy is a therapeutic option for reduction of tumor mass in patients with liver metastases, even if preoperative PTPE is required for postoperative safety, and may prolong survival or the symptom-free period.
P- Reviewers: Klinge U, Wakai T S- Editor: Wen LL L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Tischler AS. Pheochromocytoma and extra-adrenal paraganglioma: updates. Arch Pathol Lab Med. 2008;132:1272-1284. [PubMed] [Cited in This Article: ] |
| 2. | Manger WM, Gifford RW. Pheochromocytoma. J Clin Hypertens (Greenwich). 2002;4:62-72. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 104] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Kubota Y, Nakada T, Sasagawa I, Yanai H, Itoh K. Elevated levels of telomerase activity in malignant pheochromocytoma. Cancer. 1998;82:176-179. [PubMed] [Cited in This Article: ] |
| 4. | Rebai W, Kacem M, Jouini M, Bedioui H, Fterich F, Ayadi S, Daghfous A, Chebbi F, Makni A, Chouikh T. Malignant extra-adrenal pheochromocytoma--a diagnostic dilemma. Tunis Med. 2010;88:684-685. [PubMed] [Cited in This Article: ] |
| 5. | Widimský J. Recent advances in the diagnosis and treatment of pheochromocytoma. Kidney Blood Press Res. 2006;29:321-326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Honda M, Uesugi K, Yamazaki H, Dezawa A, Mizuguchi K, Yamaji T, Ishibashi M. Malignant pheochromocytoma lacking clinical features of catecholamine excess until the late stage. Intern Med. 2000;39:820-825. [PubMed] [Cited in This Article: ] |
| 7. | Fukuoka M, Taki J, Mochizuki T, Kinuya S. Comparison of diagnostic value of I-123 MIBG and high-dose I-131 MIBG scintigraphy including incremental value of SPECT/CT over planar image in patients with malignant pheochromocytoma/paraganglioma and neuroblastoma. Clin Nucl Med. 2011;36:1-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Sanford TH, Storey BB, Linehan WM, Rogers CA, Pinto PA, Bratslavsky G. Outcomes and timing for intervention of partial adrenalectomy in patients with a solitary adrenal remnant and history of bilateral phaeochromocytomas. BJU Int. 2011;107:571-575. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |