Published online Nov 27, 2012. doi: 10.4240/wjgs.v4.i11.251
Revised: August 27, 2012
Accepted: November 1, 2012
Published online: November 27, 2012
AIM: To assess the physical and mental health of fissure patients before and after topical treatment with diltiazem.
METHODS: Consecutive patients were enrolled prospectively into the study. Quality of life was measured with the short-forum 36 health survey (SF-36) before and after 6-wk treatment with diltiazem. Patients scored symptoms of pain, bleeding, and irritation using numeral rating scales at the initial and follow-up visits. Fissure healing was assessed and side effects were noted.
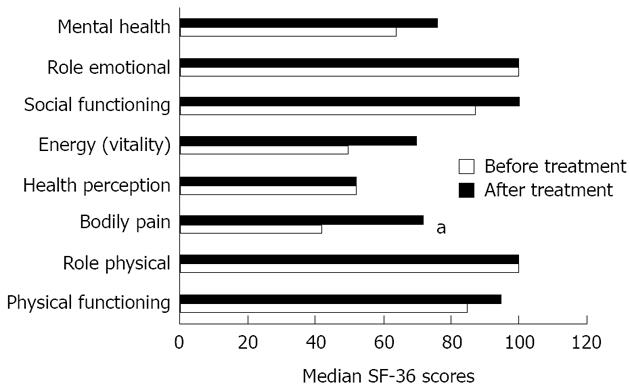
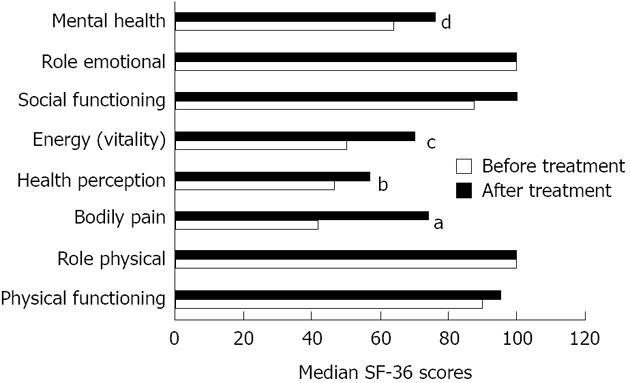
RESULTS: Fissures healed in 21 of 30 (70%) patients. There were significant reductions in the scores of pain, bleeding, and irritation after 1 wk of treatment, respectively. Four patients experienced perianal itching and one patient reported headache. When measured at baseline, pain and irritation showed a negative impact on two of the eight subscales on the SF-36, respectively (bodily pain and social functioning for pain; vitality and mental health for irritation). Repeating the SF-36 showed an improvement in bodily pain (P = 0.001). Patients whose fissures healed reported an improvement in bodily pain, health-perception, vitality, and mental health (P < 0.05).
CONCLUSION: Successful treatment of chronic anal fissure with topical diltiazem leads to improvement in health-related quality of life.
- Citation: Tsunoda A, Kashiwagura Y, Hirose KI, Sasaki T, Kano N. Quality of life in patients with chronic anal fissure after topical treatment with diltiazem. World J Gastrointest Surg 2012; 4(11): 251-255
- URL: https://www.wjgnet.com/1948-9366/full/v4/i11/251.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v4.i11.251
Anal fissure is a common problem that causes significant morbidity. It is characterized by a linear ulcer of the anoderm, mostly in the distal one third of the anal canal, and can cause pain during defecation and for three to four hours afterwards[1]. Majority of fissures is acute and resolve within 6-8 wk of conservative treatment. However, a significant minority of fissures becomes chronic and remains a continuing problem for months or even years. Chronic anal fissures are associated with hypertonia of the anal canal[2] and a reduction in mucosal blood flow, with microcirculatory disturbance and a poor healing tendency[3]. Knowledge of the ischemic nature of anal fissures and the high complication rate of surgical treatment were the basis in the search for nonsurgical treatment options, resulting in the topical application of novel agents such as, nitric oxide donors, calcium channel blockers, and local injection of botulinum toxin[4-6]. These treatments can create a reversible chemical reduction of sphincter pressure until the fissure has healed.
Little is known about the quality of life in patients with distressing symptoms of chronic anal fissure. In this study, the physical and mental health of fissure patients before and after topical treatment with diltiazem gel was assessed.
Consecutive adult patients with symptomatic chronic anal fissure attending the proctology clinic in a district hospital were enrolled in the study. Chronic anal fissure was defined as clinical examination when induration at the edge was visible and horizontal fibers of the internal anal sphincter could be seen in the base of the lesion. A history of anal pain on defecation for at least 2 mo that had failed to resolve with stool softeners was required. Exclusion criteria were (1) presumed or confirmed pregnancy; (2) allergy to diltiazem; and (3) associated complications warranting surgery (abscess, fistula and cancer). Concomitant first-degree to second degree hemorrhoids were not considered the exclusion criteria.
A prospective study was performed. Written informed consent was given by each participant. The study was approved by the ethics committee of the Kameda Medical Center in Chiba, Japan. The aim of the study was to test the efficacy of local application of 2 percent diltiazem gel in healing chronic anal fissure and evaluate the quality of life in patients with chronic anal fissure.
Patients were advised to squeeze 2 cm of the diltiazem gel onto a finger and to apply this 1 cm inside the anus and to the anal margin. Each patient was given a 6-wk course of the diltiazem gel for twice-daily application, as close to every 12 h as possible. Objective changes were assessed by the inspection of the anus to determine the extent of fissure healing (recorded as “healed” or “persistent”) at baseline and weeks 1, 3 and 6. Anoscopy was performed at baseline and on week 6. Healing of chronic anal fissure was defined at anoscopy when epithelialization or formation of a scar was achieved at week 6 of therapy.
Global quality of life was assessed using the validated Japanese version of short-forum 36 health survey (SF-36)[7]. SF-36 is a general health questionnaire which examines eight dimensions of health from the patient’s viewpoint. These dimensions are physical functioning, general mental health, role limitations due to emotional problems, bodily pain, vitality, social functioning and general health perception. SF-36 questionnaires were administered at baseline and on week 6.
Patients scored the severity of their symptoms of pain, bleeding, or perineal irritation at baseline and weeks 1, 3 and 6, on numeral rating scales (NRS) (range: 0-10); it was explained that 0 represented no symptoms and 10 the worst imaginable. Side effects such as itching, headache, and dizziness were recorded at every visit.
The dose of diltiazem used in this study was chosen on the basis of dose-response studies reported in the literature, in which concentrations of diltiazem gel greater than 2% had no additional effect on anal pressure[8]. At the completion of the trial, patients who did not heal were given the option of either an additional course of topical diltiazem gel or surgical treatment.
Data are presented median (range) unless otherwise indicated. For each of the eight dimensions on the SF-36, items scores were coded, summed and transformed on to a scale of 0 (worst) to 100 (best). A stepwise regression analysis was used to establish which variables best predicted quality of life as measured at baseline. In the regression analyses, the SF-36 subscales were selected for the dependent variables. The symptom scores of pain, bleeding or irritation at baseline were the independent variables. Age, sex, co-morbidity, employment (not in work vs employed), and duration of disease were analyzed as additional covariates. Variables were entered in the stepwise multiple regression at a P-value < 0.05, and were removed from the model at a P-value ≥ 0.05. Wilcoxon signed-rank test was used to compare baseline and follow-up paired data. Mann-Whitney U test was conducted on the cross-sectional data. SPSS 11.0 J for Windows statistical software (SPSS Japan Institute, Tokyo, Japan 2001) was used for all data analyses.
Thirty consecutive patients who fulfilled inclusion and exclusion criteria were recruited. Thirteen were male, and the median age was 54 years (18-84 years). Patients had experienced symptoms for a median of 4.5 mo (2-360 mo) at the time of inclusion in the study. There were 7 anterior fissures, 22 posterior fissures, and one patient who had both anterior and posterior fissures. Before treatment with diltiazem, no patient had received topical treatment such as glyceryl trinitrate (GTN) or isosorbite dinitrate.
The first application of diltiazem was uneventful in all patients, but 5 (17%) developed side effects subsequently. Four patients reported perianal itching; one patient discontinued diltiazem because of delayed onset of headache after 4 wk. No other side effects were reported. Overall, the median compliance rate was 100% (67%-100%). Pain, bleeding and irritaion were significantly reduced after 1 wk of treatment, respectively (Table 1).
Of the 30 patients, 21 (70%) were healed primarily with diltiazem within 6 wk. The remaining nine patients did not respond to diltiazem. Six of them received additional course of diltiazem and three were healed subsequently. Two refused surgical treatment. Remaining one patient was offered sphincterotomy. Of the 21 patients whose anal fissures healed primarily, four patients developed a recurrent fissure within 6 mo. Two patients were again treated with diltiazem gel and one was healed subsequently, the remaining two patients underwent sliding skin graft[9]. Two of the 21 patients whose anal fissures healed primarily subsequently underwent excision for prolapsed polyp.
The percentage of missing data at the item level in the SF-36 was extremely low from 0% to 2.8% (only one patient did not respond to 1 item not only at baseline, but on follow-up). The median scores of the SF-36 subscales were not significantly different regarding sex, co-morbidity, or employment. Senior patients reported significantly less physical functioning, more vitality, and more social functioning on the SF-36 scale. The patients with shorter duration of disease reported significantly bodily pain on the SF-36 scale (Table 2). The results of stepwise regression analyses, done using symptom scores and clinical variables at baseline as independent variables, are shown in Table 3. Pain at baseline showed an impact on bodily pain and social functioning, respectively. Anal irritation at baseline showed an impact on vitality and mental health, respectively. Aging was a negative predictor of physical functioning but was associated with more vitality. Duration of disease was a negative impact on role emotional. Males rather than females were correlated with better mental health.
| Number of patients | Physical functioning | Role physical | Bodily pain | Health perception | Energy (vitality) | Social functioning | Role emotional | Mental health | |
| All patients | 30 | 85 (20-100) | 100 (0-100) | 42 (0-100) | 52 (25-97) | 53 (10-100) | 88 (25-100) | 100 (0-100) | 64 (28-100) |
| Age (yr) | |||||||||
| < 54 | 15 | 95 (45-100) | 100 (0-100) | 41 (0-100) | 52 (25-97) | 45 (10-100) | 75 (25-100) | 100 (0-100) | 64 (28-96) |
| ≥ 54 | 15 | 80 (20-95) | 100 (0-100) | 42 (0-100) | 52 (35-72) | 70 (50-100) | 100 (38-100) | 100 (0-100) | 64 (40-100) |
| P1 | 0.009 | 0.71 | 0.4 | 0.87 | 0.008 | 0.04 | 0.74 | 0.31 | |
| Duration of disease (mo) | |||||||||
| < 5 | 15 | 95 (40-100) | 10 (0-100) | 41 (0-100) | 52 (25-97) | 58 (10-100) | 75 (25-100) | 100 (0-100) | 62 (28-96) |
| ≥ 5 | 15 | 85 (20-100) | 88 (0-100) | 47 (10-100) | 50 (25-82) | 50 (25-95) | 94 (50-100) | 100 (0-100) | 64 (36-100) |
| P1 | 0.43 | 0.98 | 0.04 | 0.38 | 0.64 | 0.29 | 0.73 | 0.48 | |
| Variabales included in equation | Unstandardized regression weight | t value | P value | Variabales explained |
| Physical functioning | ||||
| Age (yr) | -0.49 | -2.63 | 0.01 | 21% |
| Bodily pain | ||||
| Pain2 | -7.45 | -5.24 | < 0.0001 | 51% |
| Energy (vitalit) | ||||
| Age (yr) | 0.64 | 3.47 | 0.002 | 39% |
| Irritation2 | -2.66 | -2.14 | 0.04 | |
| Social functioning | ||||
| Pain2 | -3.83 | -2.34 | 0.03 | 17% |
| Role emotional | ||||
| Duration of disease (mo) | -0.18 | -2.61 | 0.02 | 21% |
| Mental health | ||||
| Irritation2 | -2.94 | -3.05 | 0.005 | 32% |
| Sex (males vs females) | 12.90 | 2.11 | 0.04 |
Twenty-seven patients (90%) completed the SF-36 on week 6. Repeating the SF-36 scores showed an improvement in the pain scale (P = 0.001) (Figure 1). Comparison of responders (where fissure healed) to non responders showed that the healed group had significantly higher scores on bodily pain, health perception, vitality, and mental health subscales (P < 0.05) (Figure 2). In the group where the fissure had healed, the median pain scores on follow-up were significantly lower than for non responders (0 vs 2, P = 0.002).
This study demonstrates that fissure symptoms such as pain or irritation show a negative impact on quality of life on the SF-36 as measured before treatment, but successful treatment of the fissures leads to pain diminution and beneficially affects health-related quality of life.
It bas been suggested that chronic anal fissures have an ischemic origin because of poor blood supply[3] and that they are associated with increased pressure of the internal sphincter[2]. Reduced anal sphincter pressure has been shown to increase blood flow[10], and it seems likely that this improved perfusion of the anal mucosa probably facilitates fissure healing. GTN, a nitric oxide donor, and diltiazem, a calcium channel blocker, relax the internal anal sphincter via different pathways. In keeping with earlier reports[11-13], topical 2% diltiazem gel in this study provided earlier pain relief, with a significant reduction in pain after 1 wk and preceded the significant healing rate of chronic anal fissure observed at 6 wk of treatment. Although, GTN and diltiazem have similar healing rates, diltiazem has a superior side effect profile to GTN, with an incidence of mild headaches and pruritis ani with diltiazem use lower than that of headaches with GTN use[14]. Diltiazem acting systemically would be expected to affect diastolic blood pressure[11]. Only one patient reported a recognized side effect of systemic diltiazem (headache), and discontinued the treatment in this study, but an association seems unlikely because the headaches only occurred after 4 wk of treatment. Systemic absorption of the small doses applied locally was presumably low. Four patients reported perianal itching, but no patient discontinued the treatment. Perianal itching, if caused by diltiazem gel, is likely to be local and not a systemic effect. Diltiazem may become the preferred first-line treatment for chronic anal fissure[11,15].
The patients with chronic anal fissures often report post-defecatory pain, bleeding and irritation, and the impact of such fissure symptoms on the quality of life needs to be evaluated. Griffin et al[16] reported that pain seemed to affect all of the SF-36 subscales. In our study, the regression analyses showed that pain scores on the NRS assessed before treatment were associated with not only bodily pain, but also social function on the SF-36 scale. Similarly, irritation scores were correlated with vitality and mental health on the SF-36 scale, respectively. These results seem to indicate that symptom evaluation of pain or irritation may help the staff to support the patients’ well-being in the outpatient clinic. Not surprisingly, senior patients reported poor scores of physical functioning on the SF-36 scale, but it should be carefully interpreted that they reported higher scores of vitality on SF-36 scale. Unlike the finding’s of the previous study[15], the duration of the fissure was negatively associated with role emotional on the SF-36 scale in our study. Caution is necessary in interpreting the results that males reported better scores of mental health on the SF-36 scale, because the data were cross-sectional.
We were also interested in determining the effect of anal fissure on the physical, mental and emotional aspects of a patient’s life before and after medical intervention. Our study showed that successful treatment can lead to improvements not only in bodily pain, but also in mental health, vitality and general health. No significant improvement in mental health found in the healed patients of the study by Griffin et al[16] may be due to the heterogeneous treatments given. Their patients were given either diltiazem or GTN, and quality of life was not assessed in each treatment group. Because diltiazem has a different side effect profile from GTN, quality of life should be measured in the patients treated with the same gel.
Ortiz et al[17] reported that quality of life in patients with chronic anal fissure improved significantly after internal lateral sphincterotomy in six of eight subscales of SF-36. One possible reason why these results were more favorable than those of our study is that the sample size in this study was small, so that minor changes, for example in physical and social functioning, would have passed unnoticed. Alternatively, the more limited improvement reflects the reduced efficacy of chemical sphincterotomy in patients with chronic anal fissure[18]. Another potential limitation of this study was the use of a generic instrument to measure health-related quality of life. Unfortunately, a specific questionnaire for assessment of quality of life in patients with anal fissure is not available.
The problem with chemical sphincterotomy as opposed to surgical sphincterotomy is that after treatment, the anal resting pressure may revert to pretreatment levels, and further trauma to the anoderm is likely to produce recurrence. Of the 21 patients with healing fissures, four (19%) had recurrent fissures in our study. Quality of life in the recurrent patients needs to be evaluated in extended follow-up.
In conclusion, topical 2% diltiazem appears to be a well tolerated method of chemical sphincterotomy and successful treatment of chronic anal fissure leads to improvement in health-related quality of life. Long-term follow-up is needed to assess the risk of recurrent fissure and quality of life after initial healing with diltiazem.
The authors thank Yukari Miyazaki (pharmacist) for evaluating the symptom scores.
Anal fissure is a common problem that causes significant morbidity. It is characterized by a linear ulcer of the anoderm, mostly in the distal one third of the anal canal, and can cause pain during defecation and for 3-4 h afterwards. Majority of fissures is acute and resolve within 6-8 wk of conservative treatment. However, a significant minority of fissures becomes chronic and remains a continuing problem for months or even years. Chronic anal fissures are associated with hypertonia of the anal canal and a reduction in mucosal blood flow, with microcirculatory disturbance and a poor healing tendency
Consecutive adult patients with symptomatic chronic anal fissure attending the proctology clinic in a district hospital were enrolled in the study. Chronic anal fissure was defined as clinical examination when induration at the edge was visible and horizontal fibers of the internal anal sphincter could be seen in the base of the lesion. A history of anal pain on defecation for at least 2 mo that had failed to resolve with stool softeners was required.
Fissures healed in 21 of 30 (70%) patients. There were significant reductions in the scores of pain, bleeding, and irritation after 1 wk of treatment, respectively. Four patients experienced perianal itching and one patient reported headache. When measured at baseline, pain and irritation showed a negative impact on two of the eight subscales on the short-forum 36 health survey (SF-36), respectively (bodily pain and social functioning for pain; vitality and mental health for irritation). Repeating the SF-36 showed an improvement in bodily pain. Patients whose fissures healed reported an improvement in bodily pain, health-perception, vitality, and mental health.
The results suggest that successful treatment of chronic anal fissure with topical diltiazem leads to improvement in health-related quality of life.
This paper demonstrates the physical and mental health of fissure patients before and after topical treatment with diltiazem.
Peer reviewer: Tsukasa Hotta, MD, PhD, Department of Surgery, Wakayama Medical University, School of Medicine, 811-1, Kimiidera, Wakayama 641-8510, Japan
S- Editor Wen LL L- Editor A E- Editor Zheng XM
| 1. | Goligher JC. Surgery of the anus, rectum, and colon. 5th ed. London: Balliere Tindall 1984; . |
| 2. | Farouk R, Duthie GS, MacGregor AB, Bartolo DC. Sustained internal sphincter hypertonia in patients with chronic anal fissure. Dis Colon Rectum. 1994;37:424-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 117] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Schouten WR, Briel JW, Auwerda JJ, De Graaf EJ. Ischaemic nature of anal fissure. Br J Surg. 1996;83:63-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 143] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Lund JN, Scholefield JH. Glyceryl trinitrate is an effective treatment for anal fissure. Dis Colon Rectum. 1997;40:468-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Perrotti P, Bove A, Antropoli C, Molino D, Antropoli M, Balzano A, De Stefano G, Attena F. Topical nifedipine with lidocaine ointment vs. active control for treatment of chronic anal fissure: results of a prospective, randomized, double-blind study. Dis Colon Rectum. 2002;45:1468-1475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Maria G, Cassetta E, Gui D, Brisinda G, Bentivoglio AR, Albanese A. A comparison of botulinum toxin and saline for the treatment of chronic anal fissure. N Engl J Med. 1998;338:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 209] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 927] [Cited by in RCA: 970] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 8. | Carapeti EA, Kamm MA, Evans BK, Phillips RK. Topical diltiazem and bethanechol decrease anal sphincter pressure without side effects. Gut. 1999;45:719-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 66] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Takano M. Development and status of proctology in Japan. Dis Colon Rectum. 1997;40:S68-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Lund JN, Scholefield JH. Internal sphincter spasm in anal fissure. Br J Surg. 1997;84:1723-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Jonas M, Speake W, Scholefield JH. Diltiazem heals glyceryl trinitrate-resistant chronic anal fissures: a prospective study. Dis Colon Rectum. 2002;45:1091-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Carapeti EA, Kamm MA, Phillips RK. Topical diltiazem and bethanechol decrease anal sphincter pressure and heal anal fissures without side effects. Dis Colon Rectum. 2000;43:1359-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 104] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Knight JS, Birks M, Farouk R. Topical diltiazem ointment in the treatment of chronic anal fissure. Br J Surg. 2001;88:553-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 94] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 14. | Poh A, Tan KY, Seow-Choen F. Innovations in chronic anal fissure treatment: A systematic review. World J Gastrointest Surg. 2010;2:231-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 57] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Kocher HM, Steward M, Leather AJ, Cullen PT. Randomized clinical trial assessing the side-effects of glyceryl trinitrate and diltiazem hydrochloride in the treatment of chronic anal fissure. Br J Surg. 2002;89:413-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 83] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Griffin N, Acheson AG, Tung P, Sheard C, Glazebrook C, Scholefield JH. Quality of life in patients with chronic anal fissure. Colorectal Dis. 2004;6:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Ortiz H, Marzo J, Armendariz P, De Miguel M. Quality of life assessment in patients with chronic anal fissure after lateral internal sphincterotomy. Br J Surg. 2005;92:881-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Nelson R. A systematic review of medical therapy for anal fissure. Dis Colon Rectum. 2004;47:422-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 100] [Article Influence: 4.8] [Reference Citation Analysis (0)] |