Copyright
©The Author(s) 2024.
World J Gastrointest Surg. Jul 27, 2024; 16(7): 2167-2174
Published online Jul 27, 2024. doi: 10.4240/wjgs.v16.i7.2167
Published online Jul 27, 2024. doi: 10.4240/wjgs.v16.i7.2167
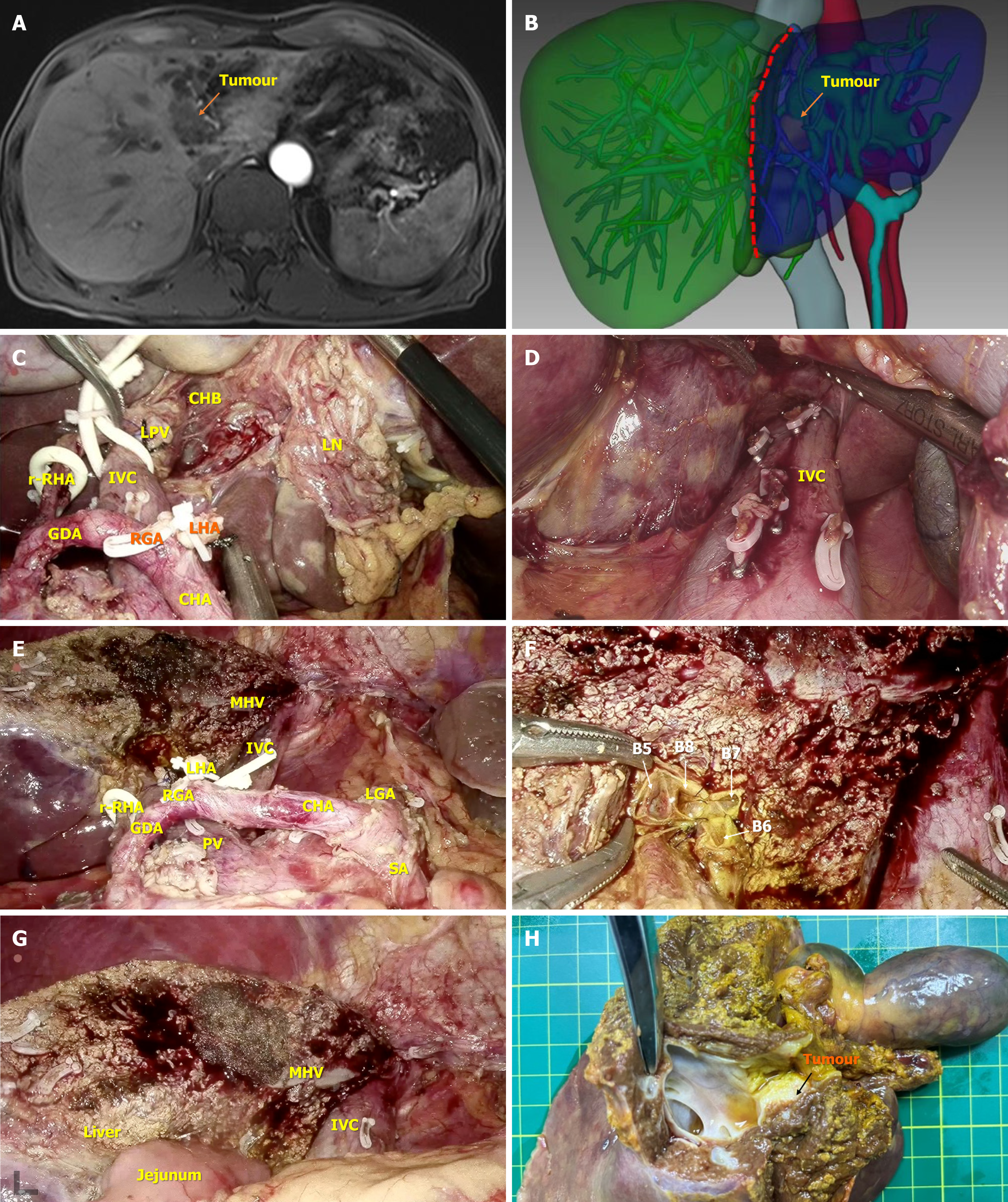
Figure 2 Typical case of the application of the strategy of “hepatic hilum area dissection priority, liver posterior separation first”.
A: Preoperative magnetic resonance imaging indicated that the patients was Bismuth-Corlette IIIb hilar cholangiocarcinoma with the invasion of the surrounding liver tissue; B: The pre-three-dimensional visualization further accurately evaluates the tumor and its surrounding adjacency, and assists in planning the surgical resection area; C: Surgical field after completion of the clearance of hepatic hilar region; D: Surgical field after completion of posterior liver ionization; E: Surgical field after completion of the left hepatic resection combined with caudate lobe resection; F: Surgical field after reconstructive operation of the right hepatic duct stump opening; G: Surgical field after completion of intrahepatic jejunal drainage; H: Display of isolated specimen. R-RHA: Replaced right hepatic artery; GDA: Gastroduodenal artery; IVC: Inferior vena cava; RGA: Right gastric artery; LPV: Left portal vein; CHB: Common hepatic bile; LHA: Left hepatic artery; CHA: Common hepatic artery; LN: Lymph node; MHV: Middle hepatic vein; PV: Portal vein; LGA: Left gastric artery; SA: Splenic artery.
- Citation: Hu XS, Wang Y, Pan HT, Zhu C, Chen SL, Zhou S, Liu HC, Pang Q, Jin H. “Hepatic hilum area priority, liver posterior first”: An optimized strategy in laparoscopic resection for type III-IV hilar cholangiocarcinoma. World J Gastrointest Surg 2024; 16(7): 2167-2174
- URL: https://www.wjgnet.com/1948-9366/full/v16/i7/2167.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i7.2167