Published online Mar 27, 2024. doi: 10.4240/wjgs.v16.i3.860
Peer-review started: October 16, 2023
First decision: January 12, 2024
Revised: January 18, 2024
Accepted: February 6, 2024
Article in press: February 6, 2024
Published online: March 27, 2024
Despite much work having been conducted on magnetic compression anastomo
To investigate the effect of different magnetic force magnets on the MCA of the digestive tract.
Two groups of magnets of the same sizes but different magnetic forces were designed and produced. A total of 24 Sprague-Dawley rats were randomly assigned into two groups (powerful magnet group and common magnet group), with 12 rats in each group. Two types of magnets were used to complete the colonic side-to-side anastomosis of the rats. The operation time and magnet discharge time were recorded. The anastomotic specimens were obtained 4 wk after the operation and then the burst pressure and diameter of the anastomosis were measured, and the anastomosis was observed via the naked eye and subjected to histological examination.
The magnetic forces of the powerful and common magnet groups at zero distance were 8.26 N and 4.10 N, respectively. The colonic side-to-side anastomosis was completed in all 24 rats, and the operation success rate and postoperative survival rate were 100%. No significant difference was noted in the operation time between the two groups. The magnet discharge time of the powerful magnet group was slightly longer than that of the common magnet group, but the difference was not statistically significant (P = 0.513). Furthermore, there was no statistical difference in the burst pressure (P = 0.266) or diameter of magnetic anastomosis (P = 0.095) between the two groups. The gross specimens of the two groups showed good anastomotic healing, and histological observation indicated good mucosal continuity without differences on healing.
In the rat colonic side-to-side MCA model, both the powerful magnet with 8.26 N and the common magnet with 4.10 N showed no significant impact on the anastomosis establishment process or its effect.
Core Tip: Magnetic compression anastomosis, which is a new type of anastomosis, has been extensively studied in digestive tract anastomosis in animals and humans. Previous studies have focused on the feasibility and safety of different magnetic designs for gastrointestinal anastomosis. Moreover, some scholars have proposed the hypothesis that magnetic force may affect the anastomosis effect. In this study, two groups of magnets matched for shape and size but with different magnetic forces were used in colonic side-to-side anastomosis experiments. The findings demonstrated that magnetic force in the range of 4.10-8.26 N did not affect the colonic side-to-side anastomosis.
- Citation: Tian BY, Zhang MM, Ma J, Lyu Y, Yan XP. Influence of different magnetic forces on the effect of colonic anastomosis in rats. World J Gastrointest Surg 2024; 16(3): 860-870
- URL: https://www.wjgnet.com/1948-9366/full/v16/i3/860.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i3.860
Since Obora reported the study of microvascular magnetic anastomosis in 1978, magnetic compression anastomosis (MCA) has attracted the attention of clinicians. The research on MCA and its clinical application in gastroenterology comprises esophageal[1-3], gastrointestinal[4-6], and small bowel[7-9] anastomosis. Other examples include vascular[10-11] and ureterovesical[12] anastomosis. During MCA of the digestive tract, the pathological process is ischemia-necrosis-shedding in the compressed tissues between the magnets and adherence-repair-healing in the surrounding tissues[13].
In MCA of the digestive tract, owing to differences in the materials, shape, size, and magnetic force of magnets used by various researchers, there is a lack of comparability in the quantitative indicators of the research findings (anastomosis establishment time, anastomosis size, and magnet discharge time). Some scholars also believe that there is an “optimal magnetic force” in MCA and have accordingly suggested that the magnetic force should be within this range when designing magnetic anastomosis devices[14,15]. Of course, the design of magnetic anastomosis device should also consider the tissue thickness, tissue edema, inflammation degree, and other related factors. However, there are only a few relevant studies, and, in the available studies, there are some flaws in the experimental design, which limit the results or obtained conclusions. Based on our cumulative research experience as a team, we believe that although magnetic devices used in digestive tract MCA should have a certain magnetic force, there might only be a lower limit for this force and not an optimal range. We propose this hypothesis based on our observation that the problem faced quite often is the magnetic force being too small to meet the demand, rather than it being too high.
In this study, a powerful magnet with a magnetic force more than two times that of common magnets was designed. The colon of Sprague-Dawley (SD) rats was used as a model to explore the influence of different magnetic forces on the MCA effect in the digestive tract.
The experimental protocol was approved by the Animal Ethics Committee of Xi’an Jiaotong University (license No. 2021-1534). A total of 24 SD albino rats (male = 12, female = 12) weighing 200-250 g were acquired from the Laboratory Animal Center of the Xi’an Jiaotong University (Xi’an, China) and used as experimental animals. The research protocol and all experimental procedures were conducted strictly in accordance with the Guidelines for the Care and Use of Experimental Animals issued by the Xi’an Jiaotong University Medical Center.
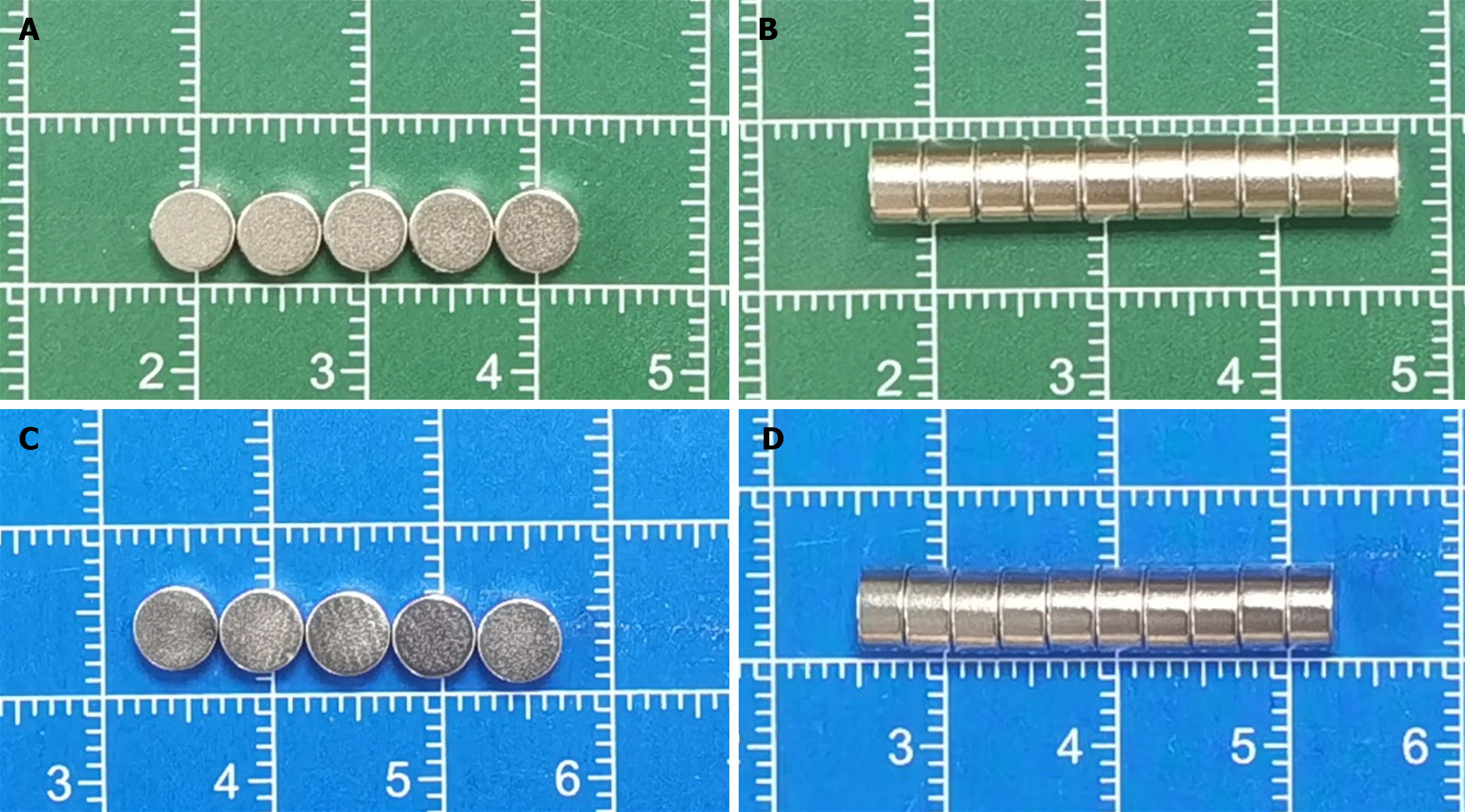
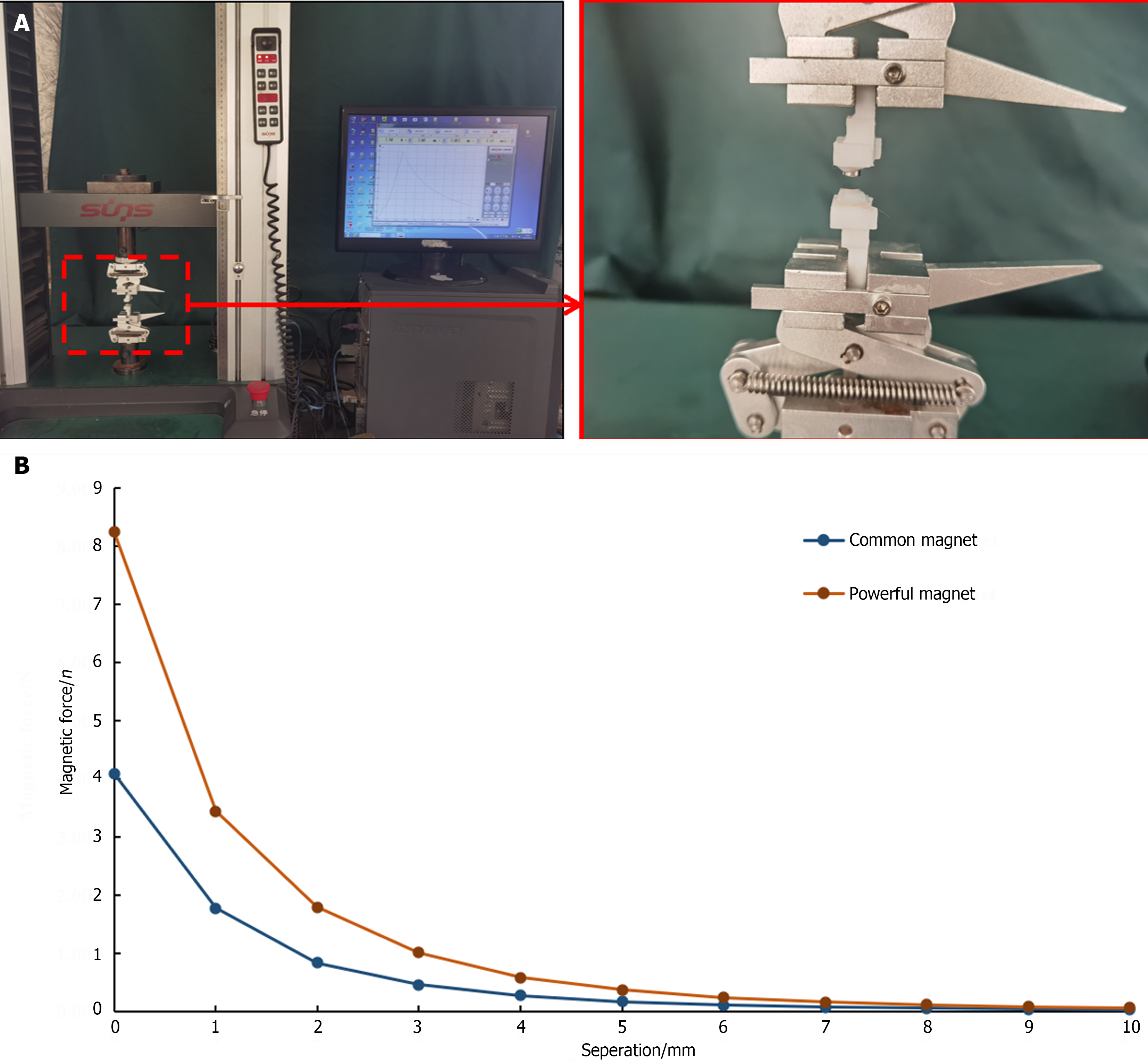
Two types of magnets were used in this study. One was a common magnet, which was processed using N 35 sintered-type neodymium-iron-boron (NdFeB). This magnet is a cylinder of diameter 5 mm and height 3 mm, and its surface is nickel-coated. The other one is a powerful magnet, which was processed using N 52 sintered NdfeB; its size and surface coating is the same as that of the common magnet. The two types of magnets are shown in Figure 1. At zero distance, the magnetic forces of the two types of magnets were 4.10 N and 8.26 N, respectively. The magnetic displacement curves of the two magnets are depicted in Figure 2, and their physical parameters are listed in Table 1.
This study aimed to investigate the effect of the magnetic force on the MCA of the digestive tract. A transanal colonic side-to-side anastomosis model with minimal effect on the outcome was used. The SD rats were randomly categorized into common and powerful magnet groups, and the two types of magnets were used to complete the colonic side-to-side anastomosis. The operation time and magnet discharge time were recorded. Anastomotic specimens were obtained by euthanizing the animals 4 wk after the operation. The burst pressure and diameter of the anastomosis were measured, and the formation of the anastomosis was observed via the naked eye and by using a light microscope (Nikon Eclipse E100, Nikon Corporation).
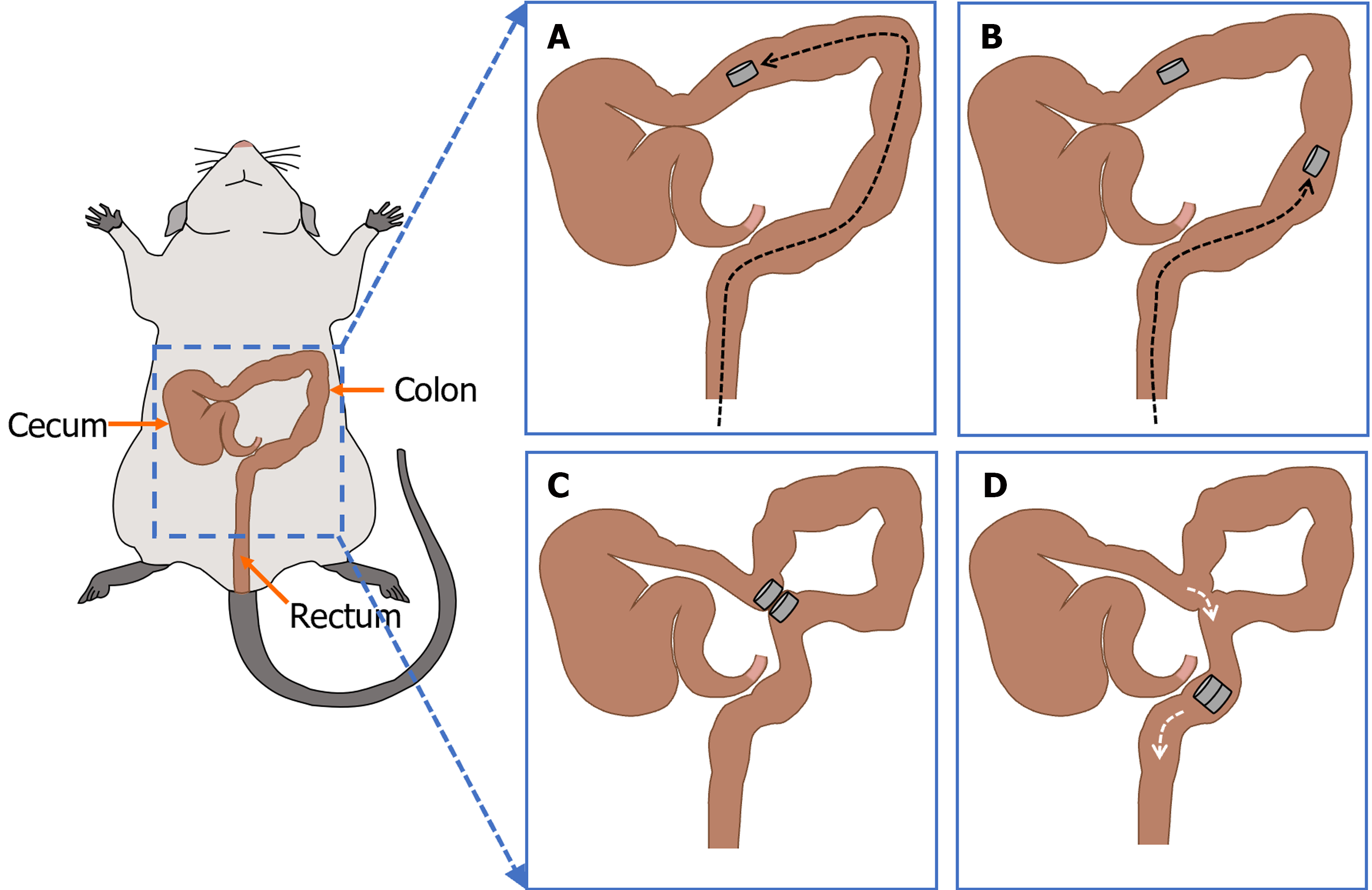
The SD rats were fed with a slag-free liquid diet 2 d before the surgery. In addition, they were fasted, and their water intake was restricted 4 h before the surgery. The animals were anesthetized via the intraperitoneal injection of pentobarbital sodium solution (30 mg/kg). After confirming the loss of the paw withdrawal reflex, the animals were fixed to a temperature-controlled operating table and their hypogastrium was shaved. The abdominal cavity was accessed via a 3 cm median incision in the skin of the lower abdomen and abdominal musculature in all rats. A magnet was pushed through the anus into the distal colon. A cotton swab was used to push it into the proximal colon under direct vision, at which time another magnet was pushed through the anus into the distal colon. After adjusting both magnets in their appropriate positions, they were attracted near the anti-mesenteric of the colon. The colon was placed back in the abdominal cavity, which was closed with a silk suture. The surgical procedure is illustrated in Figure 3.
After the recovery from anesthesia, the animals were fed normally. During the first 3 d after surgery, intramuscular pethidine (0.1 mg/100 g) was injected every 12 h. The mental state, feeding, and defecation of rats were closely monitored after the operation. The stool was checked daily until the magnet was expelled through the anus. The magnet discharge time was recorded for each rat.
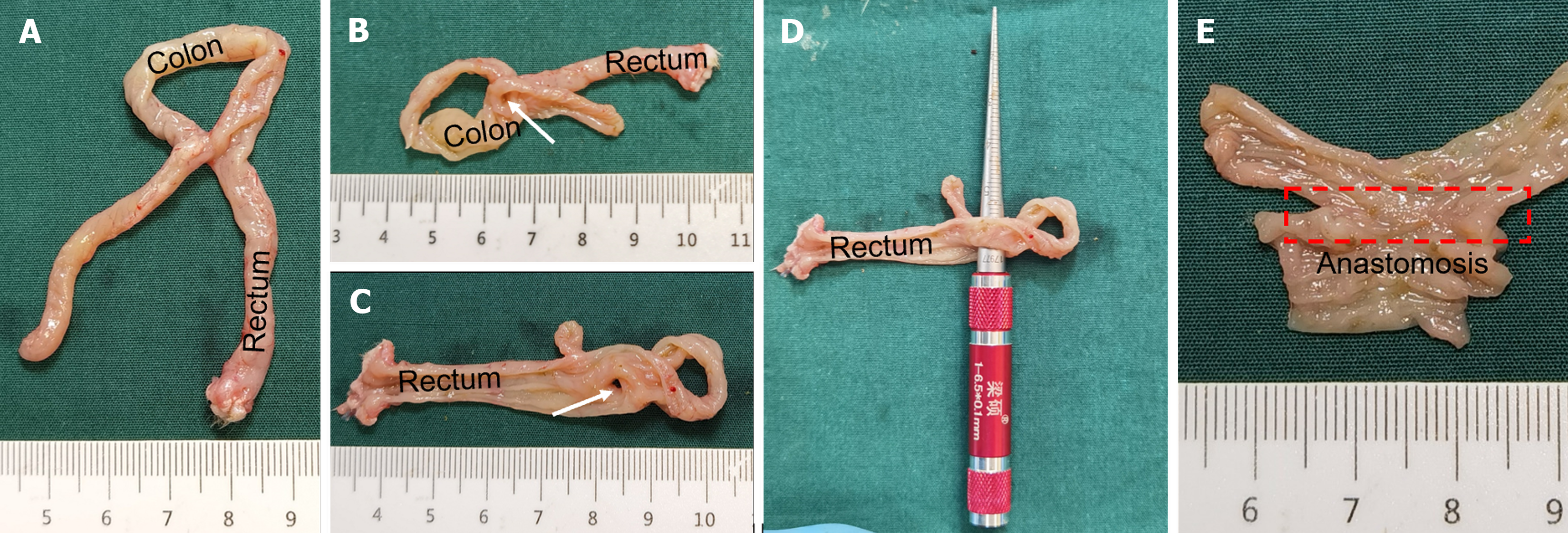
The rats were euthanized via an intraperitoneal injection of pentobarbital sodium solution (60 mg/kg) 4 wk after the surgery, and anastomotic gross specimens were obtained (the proximal end was colon bypass anastomosis with 3-5 cm of the proximal colon, and the distal end was the anus). A catheter was introduced through the other end and ligated using a single silk suture. The entire anastomosis segment was immersed in 0.9% saline. Subsequently, the intraluminal pressure was increased gradually, and the value was recorded when the first air bubble leaked from the colon and rose to the surface of the liquid. This pressure was considered the burst pressure.
The colon specimens were dissected longitudinally from both sides of the anastomosis, and the formation of the anastomosis was observed via the naked eye. The tip of the conical aperture scale was inserted into the colon anastomosis, and the intestinal anastomosis specimen was slid toward the end of the handle with appropriate force. When the resistance increased, the movement was stopped. At this time, the scale corresponding to the conical aperture scale indicated the magnetic anastomosis diameter.
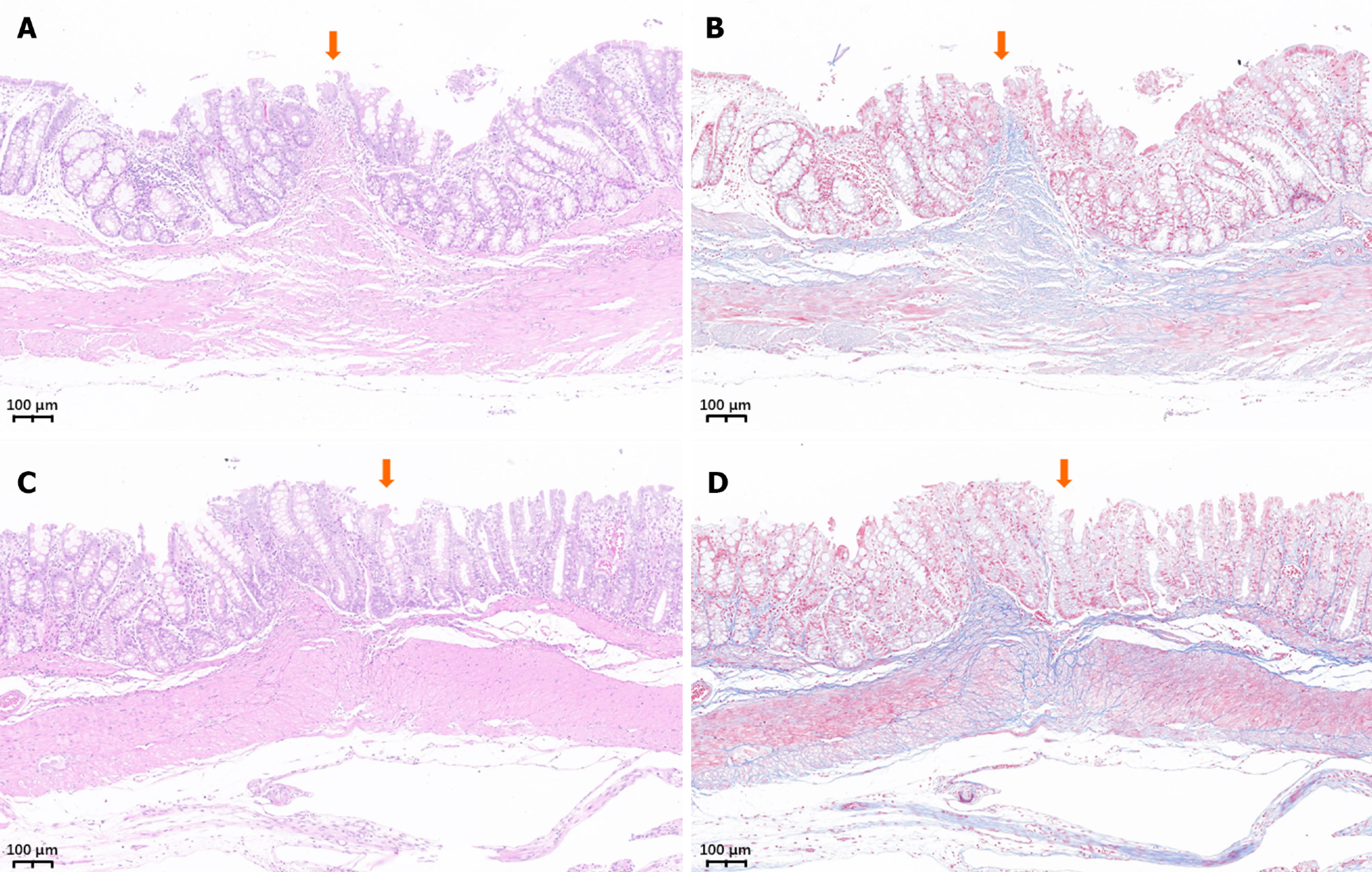
The anastomotic specimen was soaked overnight in 10% formalin for fixation and embedded in paraffin, and a 4 μm-thick section was prepared from the anastomosis. The sections were stained with hematoxylin and eosin (H&E) and Masson trichrome and examined under a bright-field microscope.
IBM SPSS statistical software version 20.0 was used for data analyses. Normally distributed quantitative data were described using mean and standard deviation, whereas non-normally distributed data were represented as median. Differences between the groups were compared using an independent samples t-test or a nonparametric test. P < 0.05 indicated a significant difference.
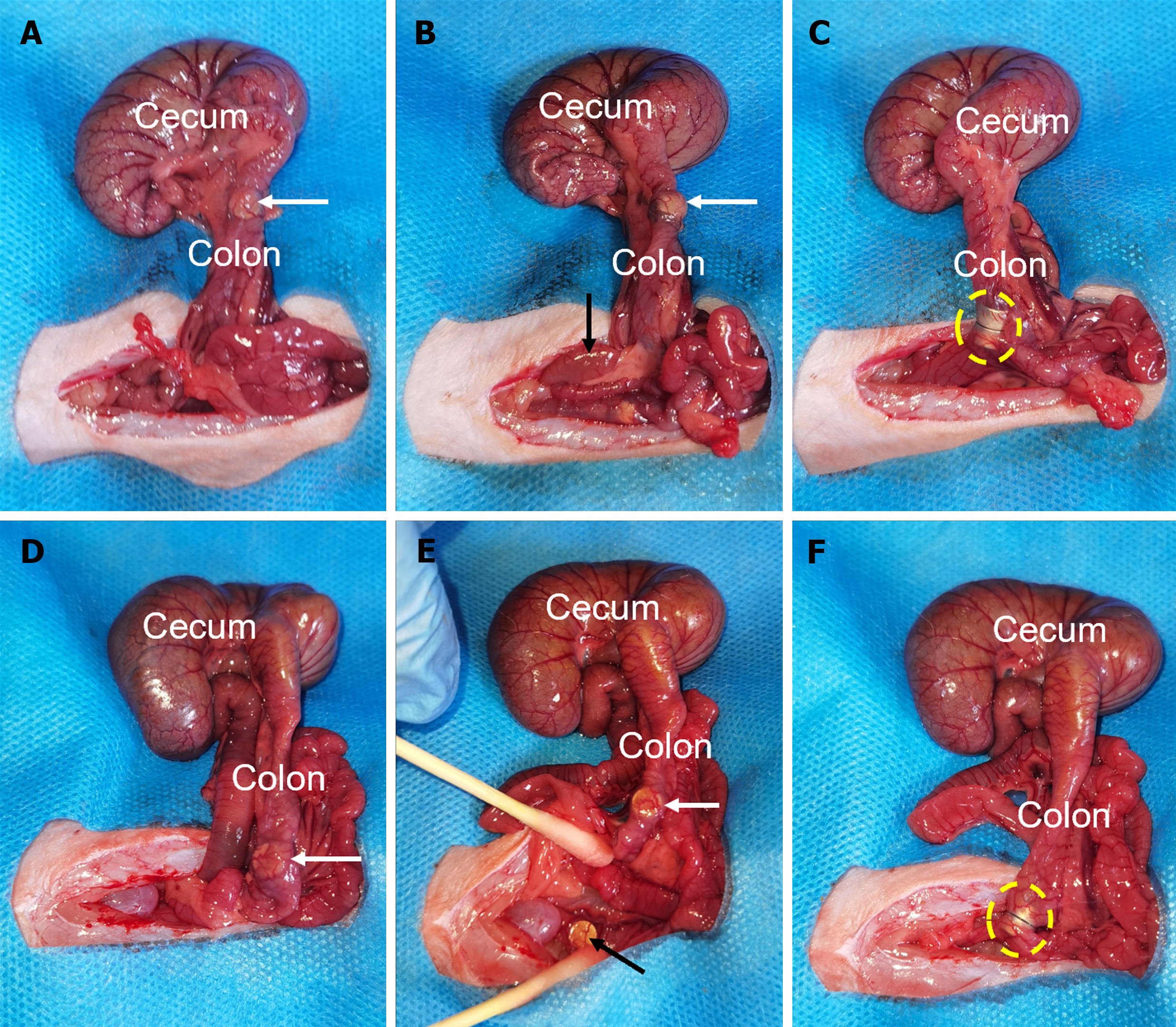
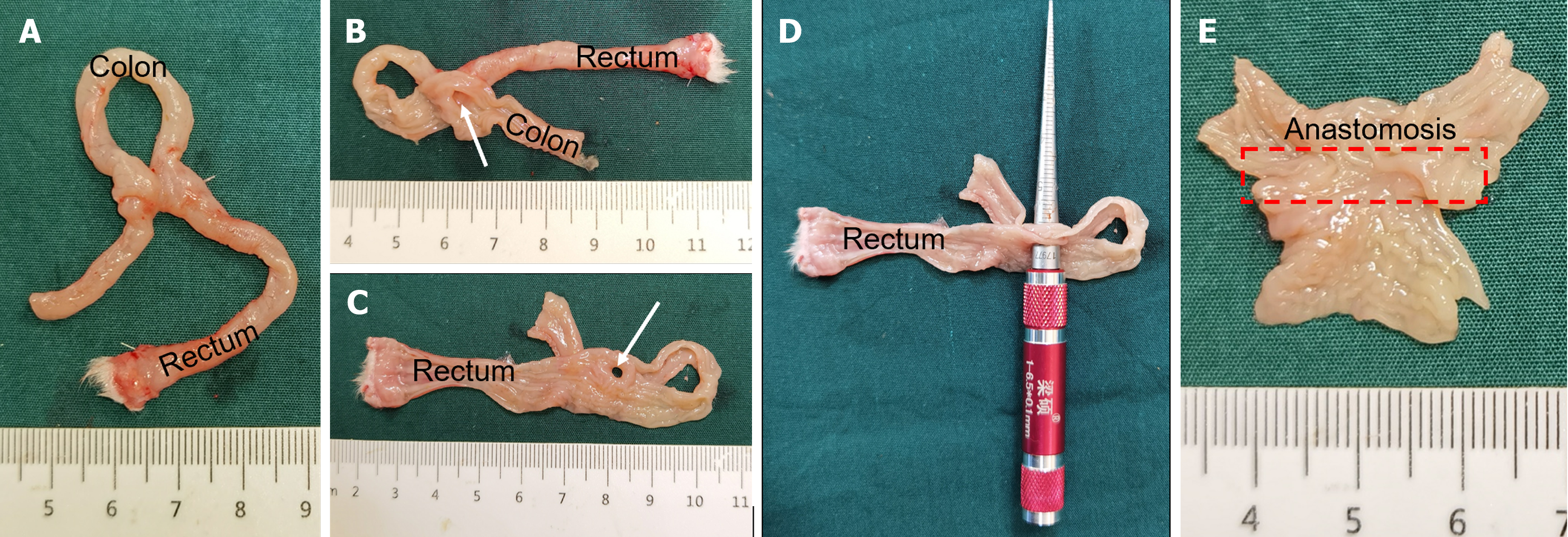
The colonic side-to-side anastomosis was performed successfully in all experimental animals with magnets inserted through the anus. During the operation, the implantation of the magnet was smooth, and it successfully completed the attraction after reaching the target position without perforation or bleeding. The operation times of the powerful and common magnet groups were 11.6 ± 2.3 min and 11.8 ± 2.4 min, respectively, with no statistical difference between the two groups (P = 0.865). The intraoperative procedures of the two groups are presented in Figure 4.
All rats survived until 4 wk after the surgery (survival rate 100%). The mental state and food intake of the animals were normal after the operation, and there were no postoperative complications, such as bleeding or intestinal obstruction.
When the anastomosis was formed, all magnets were smoothly discharged from the body. The magnet discharge time of rats in the powerful magnet group (5.3 ± 1.4 d) was slightly longer than that in the common magnet group (5.6 ± 1.1 d), but there was no statistical difference between the two groups (P = 0.513).
All experimental animals were euthanized 4 wk after the surgery, and colon samples of at least 3 cm on both ends, including the anastomosis, were obtained. The burst pressure of the anastomosis was measured using the water pumping method, and the results showed a lack of statistical difference between the two groups (261.3 ± 6.0 mmHg vs 264.3 ± 6.9 mmHg, P = 0.266). The anastomotic diameters of the two groups were 5.5 ± 0.4 mm and 5.8 ± 0.5 mm, respectively, with no statistical difference (P = 0.095). The relevant data of the results are shown in Table 2.
| Powerful magnet group | Common magnet group | P value | |
| Subjects, n | 12 | 12 | 1.00 |
| Gender, n (%) | |||
| Male | 6 (50) | 6 (50) | 1.00 |
| Female | 6 (50) | 6 (50) | |
| Weight (g) | 234.3 ± 13.5 | 233.0 ± 14.4 | 0.828 |
| Operative time (min) | 11.6 ± 2.3 | 11.8 ± 2.4 | 0.865 |
| Magnet discharge time (d) | 5.3 ± 1.4 | 5.6 ± 1.1 | 0.513 |
| Bursting pressure (mmHg) | 261.3 ± 6.0 | 264.3 ± 6.9 | 0.266 |
| Anastomotic diameter (mm) | 5.5 ± 0.4 | 5.8 ± 0.5 | 0.095 |
The colons on both sides of the anastomosis were dissected longitudinally, and the mucosa of the anastomosis was smooth without retention of any foreign body (Figures 5 and 6). H&E and Masson staining indicated good continuity of the mucosal layer of the anastomosis (Figure 7). There was no significant difference in the anastomosis between the two groups.
Several feasibility studies have been performed on MCA, a new suture-free anastomosis method; however, its clinical application is limited[16,17]. On the one hand, there are few commercial magnetic anastomosis medical devices, and on the other hand, the basic research on MCA is weak. Some scholars believe that the magnetic force plays a pertinent role in MCA, which is related to the success of the anastomosis[18]. Therefore, some researchers have examined the optimal magnetic range for MCA in different tissues. Xue et al[19] using the dog as the animal model, concluded experimentally that 0.2-0.3 MPa is the most suitable magnetic force for choledochojejunal magnetic pressure. Another study reported that the magnetic force of 6.27-13.3 N is most suitable for small intestine anastomosis in dogs[15]. However, there are presently only a few reports on the correlation between magnetic compression and the optimal magnetic force. There are differences in the schemes used, and the evaluation criteria for the optimal magnetic force are inconsistent. Hence, we believe that such studies are not sufficient.
Under a continuous magnetic force field, the intestinal wall compressed between the magnets is thought to undergo a pathological process of ischemia-necrosis-shedding. Simultaneously, the intestinal wall tissue adjacent to the magnets is believed to undergo adherence-repair-healing, which results in the formation of the anastomosis. The process of pathological change has reached a wide consensus in magnetic surgery research and has been recognized by most researchers. Based on this fact, some researchers believe that when the magnetic force is increased, the time of tissue ischemic necrosis and the time of magnetic anastomosis formation are reduced; on the contrary, when the magnetic force is reduced, the time of tissue ischemic necrosis and the time of magnetic anastomosis formation are increased. However, there is no consensus on the most suitable time for the formation of magnetic anastomosis. The so-called long or excessive anastomosis formation time may come from the subjective will of the researcher. Therefore, attempts have been made to shorten the time for establishing magnetic anastomosis by increasing the magnetic force. Nonetheless, some scholars have raised objections that excessive magnetic force can reduce the tissue ischemia-necrosis-shedding time, resulting in the incomplete healing of the tissues around the magnet. This could reduce the magnetic anastomotic burst pressure, which is an adverse consequence.
The findings from this investigation show that even when the magnetic force difference between the magnets is doubled, there is no significant difference in the magnet discharge time, anastomotic burst pressure, or colonic anastomotic healing effect. However, such a conclusion does not completely deny the potential influence of magnetic force factors on MCA of the digestive tract but merely suggests that the prime concern should be the minimum magnetic force required for MCA of the digestive tract, rather than the optimal range. In this study, the magnetic force of a similar-sized magnet was doubled, but it had no impact on the anastomosis effect. In other words, even if there is a maximum magnetic force that researchers imagine can cause a match to fail, currently available technologies cannot manufacture a magnet with such a magnetic force.
Although this study appears to have yielded a negative result, it is of great significance in the basic research on MCA. A simple animal experiment has corrected our misconceptions about the adverse effects of excessive magnetism. The findings of this investigation emphasize that developers of magnetic anastomosis devices should focus on the lower limit of magnetic force, rather than its upper limit. With the expansion of the application scenarios of MCA, the shapes of magnets are also getting diversified[20-22], and the magnetic force of these irregularly shaped magnets will also vary significantly. However, recent studies have shown that the magnetic force change has no influence on the anastomosis[23-25], which is consistent with our research results. Based on these results, a preliminary hypothesis regarding MCA was proposed, referred to as the “Yan-Zhang’s Magnetic Force Sea-Level Theory”: In gastrointestinal magnetic compression anastomosis, as it is constrained by anatomical and functional, the God limits of magnetic force cannot be reached, yet the lower limits determine whether the result is submerged in icy seawater or basking in the warm sunshine. Nevertheless, this study has certain limitations. First of all, there are only two groups in this experiment, and multiple groups with different magnetic forces should be set up to enable discoveries. Secondly, there are only a few histological indicators of colon anastomotic specimens, hence the collagen content of the anastomotic specimens should be quantitatively detected, and the inflammatory cell infiltration of the anastomotic specimens should be observed by immunofluorescence staining. Finally, the observation time of this study is short, so it is possible to obtain anastomotic specimens of more than 6 months for analysis in future studies. Therefore, designing magnets with different magnetic gradients and increasing the number of experimental groups may enhance the reliability of the experimental conclusions.
The present results establish that a magnetic force of > 4 N had no significant impact on the effect of colonic side-to-side anastomosis in rats. This observation suggests that the minimum magnetic force, rather than the maximum force, required to achieve the anastomosis warrants our attention in the MCA of the digestive tract.
Magnetic compression anastomosis, as a new type of anastomosis, mainly includes esophageal anastomosis, gas
At present, there are few reports on the relationship between MCA and optimal magnetic force, and the evaluation criteria of optimal magnetic force are inconsistent. We think that such studies are not enough.
To investigate the influence of different magnetic magnets on the anastomosis formed by MCA of digestive tract.
Colonic MCA was performed on two groups of rats using two sets of magnets of the same size but different magnetic forces. The anastomotic specimens were collected 4 wk after operation to evaluate the formation of the anastomosis in the two groups.
There was no significant difference in operation time, bursting pressure and anastomotic diameter between the two groups. The discharge time of the strong magnet group was slightly longer than that of the common magnet group, but the difference was not statistically significant. The anastomosis of the two groups of specimens healed well, the continuity of the mucosa was good, and there was no difference in healing.
The results indicate that there is no significant difference in the formation of the anastomosis between the magnets with different magnetic forces used in this experiment.
Although this study seems to have a negative result, it has important significance in the basic research of MCA.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Trébol J, Spain S-Editor: Gong ZM L-Editor: A P-Editor: Cai YX
| 1. | Hornok Z, Kubiak R, Csukas D, Ferencz A, Cserni T. Esophageal Magnetic Anastomosis Device (EMAD) to Simplify and Improve Outcome of Thoracoscopic Repair for Esophageal Atresia with Tracheoesophageal Fistula: A Proof of Concept Study. J Pediatr Surg. 2023;58:1489-1493. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Sterlin A, Evans L, Mahler S, Lindner A, Dickmann J, Heimann A, Sahlabadi M, Aribindi V, Harrison MR, Muensterer OJ. An experimental study on long term outcomes after magnetic esophageal compression anastomosis in piglets. J Pediatr Surg. 2022;57:34-40. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Mascagni P, Tringali A, Boškoski I, Bove V, Schepis T, Perri V, Costamagna G. Magnetic kissing for the endoscopic treatment of a complete iatrogenic stenosis of the hypopharynx. Endoscopy. 2023;55:E499-E500. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Gagner M, Abuladze D, Koiava L, Buchwald JN, Van Sante N, Krinke T. First-in-Human Side-to-Side Magnetic Compression Duodeno-ileostomy with the Magnet Anastomosis System. Obes Surg. 2023;33:2282-2292. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | Kawabata H, Nakase K, Okazaki Y, Yamamoto T, Yamaguchi K, Ueda Y, Miyata M, Motoi S. Endoscopic ultrasonography for pre-operative local assessment and endoscopic ultrasonography-guided marking before gastrojejunostomy for duodenal obstruction using magnetic compression anastomosis. J Clin Transl Res. 2021;7:621-624. [PubMed] [Cited in This Article: ] |
| 6. | van Hooft JE, Vleggaar FP, Le Moine O, Bizzotto A, Voermans RP, Costamagna G, Devière J, Siersema PD, Fockens P. Endoscopic magnetic gastroenteric anastomosis for palliation of malignant gastric outlet obstruction: a prospective multicenter study. Gastrointest Endosc. 2010;72:530-535. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Lebares CC, Graves CE, Lin MY, Fidelman N, Cello J, Harrison MR, Rogers S. Endoscopic Magnetic Compression Anastomosis For Small Bowel Bypass in a High Operative Risk Setting. Surg Laparosc Endosc Percutan Tech. 2019;29:e84-e87. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Schlottmann F, Ryou M, Lautz D, Thompson CC, Buxhoeveden R. Sutureless Duodeno-Ileal Anastomosis with Self-Assembling Magnets: Safety and Feasibility of a Novel Metabolic Procedure. Obes Surg. 2021;31:4195-4202. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Graves CE, Co C, Hsi RS, Kwiat D, Imamura-Ching J, Harrison MR, Stoller ML. Magnetic Compression Anastomosis (Magnamosis): First-In-Human Trial. J Am Coll Surg. 2017;225:676-681.e1. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Erdmann D, Sweis R, Heitmann C, Yasui K, Olbrich KC, Levin LS, Sharkawy AA, Klitzman B. Side-to-side sutureless vascular anastomosis with magnets. J Vasc Surg. 2004;40:505-511. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Vicol C, Eifert S, Oberhoffer M, Boekstegers P, Reichart B. Mid-term patency after magnetic coupling for distal bypass anastomosis in coronary surgery. Ann Thorac Surg. 2006;82:1452-1456. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | An Y, Zhang M, Xu S, Deng B, Shi A, Lyu Y, Yan X. An experimental study of magnetic compression technique for ureterovesical anastomosis in rabbits. Sci Rep. 2023;13:1708. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Zhang M, Lyu X, Zhao G, An Y, Lyu Y, Yan X. Establishment of Yan-Zhang's staging of digestive tract magnetic compression anastomosis in a rat model. Sci Rep. 2022;12:12445. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Lambe T, Ríordáin MG, Cahill RA, Cantillon-Murphy P. Magnetic compression in gastrointestinal and bilioenteric anastomosis: how much force? Surg Innov. 2014;21:65-73. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Zhao G, Ma J, Yan X, Li J, Ma F, Wang H, Liu Y, Lv Y. Optimized force range of magnetic compression anastomosis in dog intestinal tissue. J Pediatr Surg. 2019;54:2166-2171. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Diaz R, Davalos G, Welsh LK, Portenier D, Guerron AD. Use of magnets in gastrointestinal surgery. Surg Endosc. 2019;33:1721-1730. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Trujillo Loli Y, Trejo Huamán MD, Campos Medina S, Vega Landa JI, García Pérez R, Targarona Soler EM. Physical Bases, Indications, and Results of the Use of Magnets in Digestive Surgery: A Narrative Review. J Laparoendosc Adv Surg Tech A. 2022;32:485-494. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | Wall J, Diana M, Leroy J, Deruijter V, Gonzales KD, Lindner V, Harrison M, Marescaux J. MAGNAMOSIS IV: magnetic compression anastomosis for minimally invasive colorectal surgery. Endoscopy. 2013;45:643-648. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Xue F, Guo HC, Li JP, Lu JW, Wang HH, Ma F, Liu YX, Lv Y. Choledochojejunostomy with an innovative magnetic compressive anastomosis: How to determine optimal pressure? World J Gastroenterol. 2016;22:2326-2335. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression ostomy as new cystostomy technique in the rat: magnacystostomy. Urology. 2012;79:738-742. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Uygun I, Okur MH, Arayici Y, Keles A, Ozturk H, Otcu S. Magnetic compression ostomy for simple tube colostomy in rats--magnacolostomy. Adv Clin Exp Med. 2012;21:301-305. [PubMed] [Cited in This Article: ] |
| 22. | Uygun I, Okur MH, Cimen H, Keles A, Yalcin O, Ozturk H, Otcu S. Magnetic compression gastrostomy in the rat. Pediatr Surg Int. 2012;28:529-532. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Li GZ, Ryou M, Thompson CC, Wang J. A Preclinical Study of an Esophagojejunal Compression Anastomosis After Total Gastrectomy with Self-Forming Magnets. J Gastrointest Surg. 2023;27:1710-1712. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Ore AS, Askenasy E, Ryou M, Baldwin T, Thompson CC, Messaris E. Evaluation of sutureless anastomosis after ileostomy takedown using the self-forming magnet anastomosis system in a porcine model. Surg Endosc. 2022;36:7664-7672. [PubMed] [DOI] [Cited in This Article: ] |
| 25. | Pichakron KO, Jelin EB, Hirose S, Curran PF, Jamshidi R, Stephenson JT, Fechter R, Strange M, Harrison MR. Magnamosis II: Magnetic compression anastomosis for minimally invasive gastrojejunostomy and jejunojejunostomy. J Am Coll Surg. 2011;212:42-49. [PubMed] [DOI] [Cited in This Article: ] |