Copyright
©The Author(s) 2022.
World J Gastrointest Surg. Feb 27, 2022; 14(2): 78-106
Published online Feb 27, 2022. doi: 10.4240/wjgs.v14.i2.78
Published online Feb 27, 2022. doi: 10.4240/wjgs.v14.i2.78
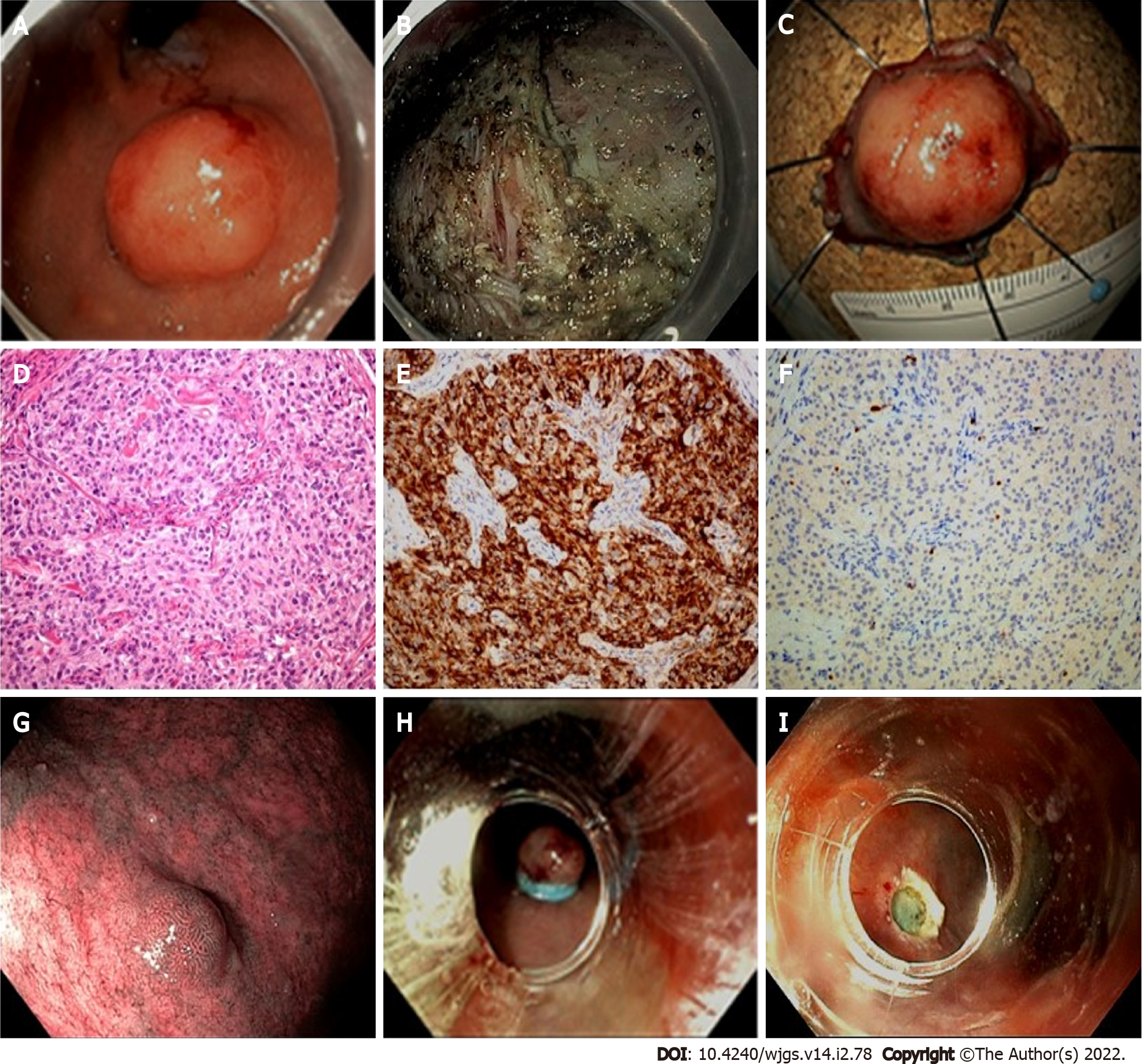
Figure 2 Endoscopic management of gastric neuroendocrine tumors presentation of a clinical case referred to our hospital.
A 78-year-old female patient was referred to our Endoscopy Unit for resection of a lesion of the gastric fundus. Staging by endoscopic ultrasound showed hypoechoic lesion of 19 mm × 12 mm, with well-defined margins, originating from the third hyperechoic layer. Fine-needle cytology diagnosed a NET G1 (Ki67 < 2%). The lesion was then resected by endoscopic submucosa dissection (ESD). Histological evaluation described a gastric NET (g-NET) G1, associated with autoimmune gastritis (Type I). During follow-up, another minor lesion (< 10 mm) suspected for NET was reported along the greater curvature, and resected by Band-ligation endoscopic mucosal resection (EMR-L). Histological report confirmed a Type I g-NET. A: Cardial area reflexed view; B: Resection base after ESD; C: Oriented and pinned specimen; D: Hematoxylin-eosin stain showing monomorphic cells in a nested architecture without necrosis; E: Corresponding Chromogranin A immunostain (20 × magnification); F: Corresponding Ki67 immunostain (20 × magnification); G: Endoscopic appearance of the lesion detected during follow-up; H: EMR-L: Rubber band release; I: Resection base after EMR-L.
- Citation: Merola E, Michielan A, Rozzanigo U, Erini M, Sferrazza S, Marcucci S, Sartori C, Trentin C, de Pretis G, Chierichetti F. Therapeutic strategies for gastroenteropancreatic neuroendocrine neoplasms: State-of-the-art and future perspectives. World J Gastrointest Surg 2022; 14(2): 78-106
- URL: https://www.wjgnet.com/1948-9366/full/v14/i2/78.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i2.78