Published online Jun 15, 2012. doi: 10.4239/wjd.v3.i6.110
Revised: June 4, 2012
Accepted: June 10, 2012
Published online: June 15, 2012
Diabetes is a major lifestyle disorder, the prevalence of which is increasing globally. Asian countries contribute to more than 60% of the world’s diabetic population as the prevalence of diabetes is increasing in these countries. Socio-economic growth and industrialization are rapidly occurring in many of these countries. The urban-rural divide in prevalence is narrowing as urbanization is spreading widely, adversely affecting the lifestyle of populations. Asians have a strong ethnic and genetic predisposition for diabetes and have lower thresholds for the environmental risk factors. As a result, they develop diabetes at a younger age and at a lower body mass index and waist circumference when compared with the Western population. The adverse effect of physical inactivity and fatty food are manifested as the increasing rate of overweightness and obesity, even among children. The health care budgets for the disease management are meager and the health care outcome is far from the optimum. As a result, complications of diabetes are common and the economic burden is very high, especially among the poor strata of the society. National endeavors are urgently needed for early diagnosis, effective management and for primary prevention of diabetes. This editorial aims to highlight the rising trend in prevalence of diabetes in Asia, its causative factors and the urgent need to implement national strategies for primary prevention of type 2 diabetes.
- Citation: Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes 2012; 3(6): 110-117
- URL: https://www.wjgnet.com/1948-9358/full/v3/i6/110.htm
- DOI: https://dx.doi.org/10.4239/wjd.v3.i6.110
The prevalence of diabetes, constituted chiefly by type 2 diabetes (T2D), is a global public health threat. The prevalence among adults aged 20-70 years is expected to rise from 285 million in 2010 to 438 million by the year 2030[1]. While T2D poses a huge economic burden to all nations, developing countries bear the highest burden since more than 80% of cases occur in these countries. Prevalence estimates of diabetes and impaired glucose tolerance (IGT) are high for all Asian countries and are expected to increase further in the next two decades[1]. The present trend indicates that more than 60% of the world’s diabetic population will be in Asia. This editorial aims to highlight the rising trend in prevalence of diabetes in Asia, its causative factors and the urgent need to implement national strategies for primary prevention of T2D.
Table 1 shows the changing trends in the prevalence of diabetes in South Asian countries[2-31]. In the past two decades, the prevalence in urban areas has increased remarkably in most countries, the increase being phenomenal in Nepal[16-18] and China[4-6]. The national prevalence has increased by two fold or more within a decade in many countries[6,8,22,29,31]. Rural prevalence has increased considerably in India[9], Nepal[18] and China[6]. India and China have large rural populations and hence the increased prevalence of diabetes in rural areas has contributed to the overall national increase in the prevalence of diabetes in these countries.
| Country | Year | Diagnosis method | Criteria | Prevalence (%) | Fold increase (%) | ||||
| National | Urban | Rural | National | Urban | Rural | ||||
| Bangladesh[2,3] | 1997 | FPG/OGTT | WHO 1985 | 4.5 | |||||
| 2005 | FPG/OGTT | WHO 1999 | 8.1 | 2.3 | 1.8 (8 yr) | ||||
| China | |||||||||
| Mainland[4-6] | 1994 | FPG/OGTT | WHO 1985 | 2.5 | |||||
| 2001 | FPG/OGTT | WHO 1985 | 6.1 | 6.9 | 5.6 | 2.4 (7 yr) | |||
| 2008 | OGTT | WHO 1999 | 9.4 | 11.4 | 8.2 | 3.8 (13 yr) | 1.7 (6 yr) | 1.5 (6 yr) | |
| Hong Kong[7,8] | 1990 | OGTT | WHO 1985 | 4.5 | |||||
| 1996 | FPG/OGTT | ADA 1997/WHO 1998 | 9.8 | 2.2 (6 yr) | |||||
| Taiwan[28,29] | 1987 | FPG/OGTT | WHO 1985 | 4.4 | 2.2 (8 yr) | ||||
| 1996 | OGTT | WHO 1985 | 9.2 | ||||||
| India[9,10] | 1989 | FPG/WHO | WHO 1985 | 8.2 | 2.4 | 2.3 (16 yr) | 3.8 (16 yr) | ||
| 2006 | OGTT | WHO 1999 | 18.6 | 9.2 | |||||
| Indonesia[11,12] | 1981 | OGTT | WHO 1980 | 1.6 | |||||
| 1995 | 5.7 | 3.5 (13 yr) | |||||||
| South Korea[13] | 1997 | OGTT | ADA 1997 | 6.9 | |||||
| 2003 | OGTT | ADA 1997 | 11.7 | 1.7 (6 yr) | |||||
| Malaysia[14,15] | 1982 | NA | 2.1 | ||||||
| 2006 | FPG | WHO 1985 | 11 | 5.2 (24 yr) | |||||
| Nepal[16-18] | 1990 | FPG | ADA 1997 | 1.41 | 0.3 | ||||
| 1999 | FPG | ADA 1997 | 14.6 | 2.5 | 6.81 (17 yr) | 8.3 (11 yr) | |||
| 2007 | NA | NA | 9.51 | ||||||
| Pakistan[19] | 2006 | OGTT | WHO 1985 | 10.6 | 7.7 | ||||
| Philippines[20] | 1982 | OGTT | ≥ 11.0 mmol/L | 3.3 | |||||
| 2002 | OGTT | WHO 1999 | 4.9 | 1.5 (19 yr) | |||||
| Singapore[21-23] | 1985 | OGTT | WHO 1985 | 4.7 | |||||
| 1998 | FPG/OGTT | WHO 1985 | 9 | ||||||
| 2004 | FPG/OGTT | WHO 1985 | 8.2 | 1.9 (19 yr) | |||||
| Sri Lanka[24,25] | 1994 | OGTT | WHO 1985 | 5 | |||||
| 2005 | FPG/OGTT | ADA 1997 | 10.3 | ||||||
| Thailand[26,27] | 2000 | FPG | ≥ 7 mmol/L | 6.7 | |||||
| 2004 | FPG | WHO 1985 | 9.6 | 1.4 (4 yr) | |||||
| Taiwan[28,29] | 1987 | FPG/OGTT | WHO 1985 | 4.4 | 2.2 (8 yr) | ||||
| 1996 | OGTT | WHO 1985 | 9.2 | ||||||
| Vietnam[30,31] | 1990 | FPG | ADA | 1.4 | |||||
| 2001 | OGTT | WHO 1985 | 3.8 | 2.7 (11 yr) | |||||
The recent improvements seen in health status of people of Singapore in the National Health Survey are commendable[23]. In the past 50 years, the country achieved rapid economic progress and underwent an epidemiological transition from a high prevalence of infectious diseases to a high prevalence of lifestyle-associated chronic non communicable diseases such as diabetes, hypertension (HTN) and cardiovascular risk factors. In 1991, Singapore’s Review Committee on National Health Policies reviewed the country’s health care services and endorsed policies focusing on health promotion and disease prevention and control of health risk factors, including overweightness and obesity. A series of health promotion measures were initiated in 1992 under the National Healthy Lifestyle Program, focusing on not smoking, being physically active, eating right and managing stress to combat major chronic disease and their risk factors. Health education and disease prevention campaigns made significant achievements in the health status of the people.
With the national initiatives taken to improve the health status of the people, a decrease was seen for the first time in the prevalence of diabetes (from 9% in 1998 to 8.2% in 2004)[23]. A remarkable reduction was seen in other cardiovascular risk factors, such as hypertension, dyslipidemia and smoking. Physical activity levels have shown improvement, although much needs to be done to tackle the problem of rising overweightness and obesity.
The escalating prevalence of diabetes seen in the last two to three decades can be attributed mostly to the change in lifestyle as a result of rapid socioeconomic growth. The rise in prevalence, therefore, is a result of environmental and behavioral changes and cannot be attributed to altered gene frequencies since the increase has occurred within a few decades. It is estimated that the substantial increase in urbanization will occur in most Asian countries, although the rates are variable among these countries[32]. The highest rates of urbanization (50%) have been in Singapore, Korea, Malaysia, Philippines and Indonesia. China, Pakistan, India and Thailand have intermediate rates (30%) and Bangladesh and Sri Lanka have slow rates of urbanization. The increase in urban population and aging are the main determinants of the global rise in prevalence of diabetes. Urbanization and internal rural to urban migration result in several adverse impacts; physical activity decreases, diet habits shift towards high-energy foods and body mass index (BMI) and upper body adiposity increase considerably.
Socio-economic progress, occurring even in the rural areas of countries such as India and China, have adversely affected the proportion of people affected with lifestyle disorders such as obesity, diabetes, HTN and cardiovascular diseases (CVD). As shown in the recent studies in India[10] and China[6,33], considerable changes have occurred in the living pattern of the rural population, leading to an increase in total prevalence of overweightness and diabetes in these countries. In 1980, less than 1% of Chinese adults had diabetes and in 2008, the prevalence had increased to nearly 10%[6].
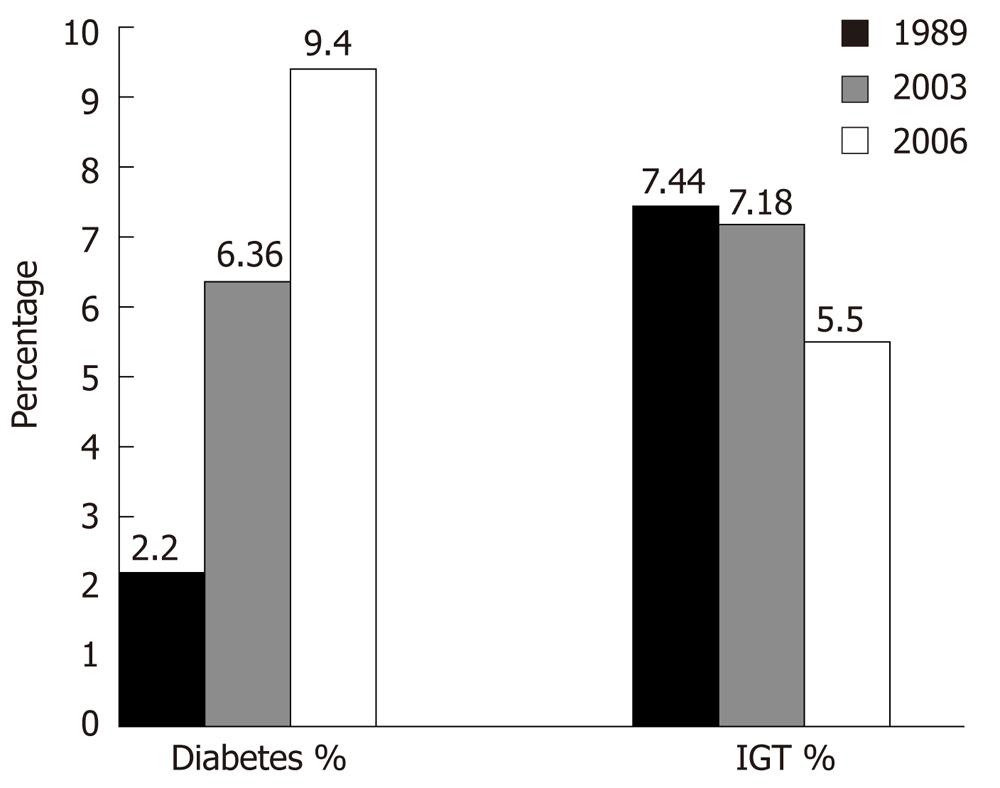
The temporal change in the prevalence of diabetes and IGT in rural India over the period of 1989-2006 is shown in Figure 1[10]. Similar trends have been described for Thailand, Malaysia, Bangladesh and Pakistan[34]. A large pool of prediabetic subjects exists even in the rural region, as shown by the high prevalence of IGT. Recent studies in India showed that the conversion rate of IGT to diabetes is high, probably on account of the influence of lifestyle transitions[10,35]. It was noted that the prevalence of IGT decreased from 7.2% in 2003 to 5.5% in 2006, with a concomitant increase in the prevalence of diabetes. In another rural region in India, the crude prevalence of diabetes was 13.2% and prevalence of IGT was 15.9% in 2006[36]. Several other reports also show the rising trend in the prevalence of diabetes in rural regions[37,38].
The natural history of prediabetes is unclear. A review of data from 79 cross sectional studies in South Asian populations showed that diabetes prevalence was rising, whereas IGT prevalence was stable[39]. Possible explanations for this apparent discrepancy are a rapid conversion of IGT to diabetes produced by lifestyle transition or a cohort effect, with improving maternal and infant nutrition in reduced IGT and with a fall in diabetes to follow. More prospective studies are needed to address these hypotheses.
Asian populations develop diabetes at a younger age than Western populations[39]. However, racial variations within Asia are evident in the age specific prevalence of diabetes. In the Asian Indian population, prevalence of diabetes peaks at 60-69 years of age, whereas in the Chinese population it peaks at 79-89 years. Indians also have a higher prevalence of IGT at a younger age than the Chinese population. The findings from Pakistan[19] and Sri Lanka[25] are similar to the results from India[10]. The ethnic differences in the prevalence of diabetes and impaired glucose regulation may not be completely explained by the living environment and geographical locations, suggesting a major role for genetic factors as well[40]. It may also be related to an interplay of higher rates of central obesity, insulin resistance, genetic predisposition and/or influence of adverse intrauterine influences present among the Asian Indian population.
As the prevalence of diabetes increases, the proportion of young people with diabetes also increases. The rapidly increasing prevalence of T2D in the youth is highlighted by studies in the Asian populations in native lands and in migrant countries. China showed an 88% increase in prevalence in 35-44 years age group within a period of 6 years[41]. In southern India, the prevalence of diabetes in persons under 44 years has increased from 25% of the total prevalence in 2000 to 36% in 2006[10]. Asian people with young onset of diabetes have substantial phenotypic heterogeneity, many with a positive family history, impaired beta cell function, no islet cell autoantibodies and with clustering of cardio metabolic disorders[42,43]. The major cause for the increasing prevalence of T2D in Asian children is the increasing rate of obesity and decreasing rate of physical activity, leading to insulin resistance[44]. Most of the Asian countries are largely rural; hence a sudden change in the lifestyle of the rural people would increase the number of people affected by metabolic disorders.
The rising trend seen in the prevalence of gestational diabetes among Asian women and the increased risk for future diabetes in them may also contribute to the escalating prevalence of diabetes in young people[45].
Although the prevalence of obesity and being overweight are relatively lower in Asia compared with Western populations, the recent socioeconomic transition in Asia is resulting in a parallel increase in its prevalence. Among Asians, diabetes occurs at lower BMI levels than in Western populations and small increments in weight triggers glucose intolerance in susceptible subjects[40,46,47]. Analysis of the National Health Interview survey in the United States from 1997 to 2008 showed that Asian Americans had a significantly higher rate for diabetes than the whites throughout the study period[48]. There was a significant upward trend in both groups for diabetes and BMI. However, Asian Americans, especially Asian Indians, had higher odds of developing diabetes, despite having a significantly lower BMI than the white population.
Several studies in Asian populations, particularly in Asian Indians, have highlighted the “metabolically obese” phenotype among normal weight individuals[46-53]. This phenotype, characterized by greater abdominal obesity despite a normal BMI, less muscle mass, higher percentage of body fat and increased propensity for insulin resistance compared with the Western population, renders higher susceptibility for diabetes in Asian populations[49-52].
The association of BMI and diabetes is modified by ethnicity[40]. Ethnicity is associated with several factors, such as genetic constitution, lifestyle, living environment and anthropometric characteristics. Body composition related to fat distribution is a stronger determinant of the metabolic milieu than BMI. The diabetes epidemiology, collaborative analysis of diabetes criteria in Europe/in Asia study group noted that the overall effect of age on the prevalence of diabetes differed considerably between the ethnic groups, even in the subjects with the same BMI[40]. Asian populations are prone to have more intra abdominal fat accumulation and low muscle mass. Asian Indians, in particular, have the above abnormalities which account for the high prevalence of insulin resistance and diabetes at low levels of BMI. A study by our group showed that the risk of diabetes increases progressively from a BMI of ≥ 23 kg/m2 among Indians[54]. BMI in ≥ of 23 kg/m2 is also considered overweight for most Asian populations[55].
The risk of diabetes is shown to be higher by 45% in smokers than among non smokers[56]. Smoking increases the risk of central obesity and insulin resistance[57] and nicotine exposure has several other deleterious effects. Asian countries such as China and India continue to produce and consume tobacco products and hence face a huge public health problem.
The increasing use of alcohol in Asian countries, especially among the middle class and rural population, also increases the risk for diabetes and other metabolic diseases.
Prevalence of T2D is high among Asian populations, particularly so in Asian Indians, by virtue of a high genetic susceptibility and enhanced interaction with environmental triggers. Exposure to a high fat diet and lower levels of physical activity are the common factors which trigger the gene-environmental interaction.
Both the thrifty genotype and thrifty phenotype hypotheses appear to have etiological roles in development of diabetes in Asian populations. While the thrifty genotype hypothesis points to a mismatch between the ancestral genes and modern environment, the thrifty phenotype hypothesis postulates a mismatch between intrauterine and adult life environments[58]. The selective presence of “thrifty genotypes”has been considered to be advantageous in certain populations during evolutionary selection by repeated famine and feast cycles. However, these genes have rendered them highly predisposed to obesity and diabetes during the modern of era of continuous feasting[59]. The “thrift phenotype” hypothesis postulates that intrauterine malnutrition leads to metabolic and structural changes in the beta cells that are beneficial for early survival, but increases the risk of T2D and other chronic disorders in adulthood[60]. Rapid weight gain occurring in childhood due to a nutritionally rich environment enhances the risk of these adult diseases. A recent collaborative study of prospective data from large numbers of individuals in 5 low and middle income countries, including India, showed that lower birth weight is a risk factor for glucose intolerance[61]. Higher than expected weight gain between 48 mo and adolescent/adult is also a risk factor for glucose intolerance.
The combination of gestational diabetes, in utero nutritional imbalance, childhood obesity and over nutrition in adulthood will continue to fuel the epidemic in Asian countries undergoing rapid nutritional transitions[58].
Asian diabetic patients have a high risk of developing long term diabetic complications because they develop the disease earlier. The association between vascular complications and poor glycemic control is well known[62,63]. The health care outcome among diabetic patients in many Asian countries is far from optimum.
Diabetes is associated with debilitating micro and macro vascular complications. As Asian populations develop diabetes at a young age, they live long enough to develop the complications too, resulting in high rates of morbidity and early mortality[1]. The risk of CVD increases by 3-4 fold in a diabetic person. More than 75% of all mortality among diabetic persons occurs from cardiovascular disease[64]. The UK Prospective Diabetes Study (UKPDS) showed that every 1% increase in HbA1c was associated with 12% increase in heart failure[64]. In diabetic subjects, several stronger risk factors other than the classic risk factors exist, such as elevated small, dense low-density lipoprotein (LDL) cholesterol or oxidized LDL, which confer a higher risk in diabetic than in non-diabetic individuals with elevated LDL. The process of atherogenesis in diabetes is complex and consists of interrelated multiple factors. The chronic hyperglycemia activates the mechanisms related to atherogenesis. The cardiovascular pathology is related to a combination of both micro and macrovascular dysfunction[64]. The epidemiology of diabetes intervention and complications study[65] in type 1 diabetes and the extended UKPDS study[66] have shown definite cardiovascular benefit with lowering of blood glucose levels.
Few population based data on prevalence of diabetic complications are available from developing countries. However, it is been estimated that nearly 30% of type 2 diabetic patients in Asian countries have retinopathy. The prevalence of diabetic end stage renal disease is also higher than among the white populations. The prevalence of neuropathy and foot complications are also high among the Asian patients[46,47].
The young age at onset not only increases the health care burden of treating large numbers of people with diabetes, but also increases the morbidity and premature mortality due to diabetic complications. The rate of complications increases proportionally with the duration of diabetes.
The cost of diabetes care is high and increasing worldwide. The economic burden is very high, especially in developing countries, and more so in the lower economic groups, who spend 25%-34% of their income on diabetes care[67,68]. The cost of care increases substantially when complications occur or when admission to hospital, surgery or insulin treatment is needed.
Studies from developed western countries and developing countries in Asia have shown similar results with respect to the quality of diabetes care and the glycemic outcome among the diabetic population[67,69]. Less than 30% of the patients achieve the desired glycemic goals[69].
In most Asian countries, the medical challenge posed by the burden of diabetes is huge. It is unmatched by the budget allocations for health care. Primary prevention is important to reduce the burden of diabetes faced by patients, families and society at large. Several prospective randomized clinical trials have shown that primary prevention of T2D is possible by lifestyle intervention or by the use of pharmacological agents such as metformin[70]. The Chinese Da-Qing study[71] and the Indian Diabetes Prevention Programs[72] have shown the benefits of lifestyle modification focused on improved physical activity and healthy diet habits to prevent or at least delay the onset of diabetes in high risk subjects. Lifestyle intervention can have a sustained 43% reduction in the incidence of diabetes over a 20 year period[73].
Prevention of obesity and diabetes will be cost effective as it will prevent not only the development of diabetes but can also prevent the occurrence of complications.
The serious epidemic nature of diabetes has been recognized by the United Nations and it recommends member countries to develop national policies to combat the disease. In several Asian countries, governments have initiated national programs for the prevention and control of non-communicable diseases[74]. The health care programs implemented by Singapore have been effective and fruitful[23].
The health care and societal burden of diabetes is alarming in many Asian countries, particularly in China and India. In addition to the rising number of people with the disease and its complications, the younger age at which the disease develops and the escalating occurrence of T2D in children and adolescents are of significant concern. Rapid rates of urbanization, modernization, readily available fast foods and sedentary habits have altered the lifestyle of the population, more so among the youth. The health consequences are devastating in Asian populations due to a strong genetic predisposition to metabolic diseases like diabetes and CVD. Current lifestyle parameters perhaps accelerate the clinical expression of the disease at a very young age itself.
Primary prevention of diabetes is possible by modifying risk factors such as obesity and insulin resistance[70-74]. National programs promoting healthy lifestyle among the population, starting from a young age, should be given priority in the health care agenda.
Peer reviewers: Dr. Kristine Færch, Steno Diabetes Center, Niels Steensens Vej 2, DK-2820 Gentofte, Denmark; Sokratis Pastromas, MD, First Cardiology Department, Evagelismos Hospital, Ipsilantou 45-47, 106 76 Athens, Greece
S- Editor Wu X L- Editor Roemmele A E- Editor Zhang DN
| 1. | Unwin N, Whiting D, Gan D, Jacqmain O, Ghyoot G, editors . IDF Diabetes Atlas. 4th ed. Brussels: International Diabetes Federation 2009; . [Cited in This Article: ] |
| 2. | Sayeed MA, Hussain MZ, Banu A, Rumi MA, Azad Khan AK. Prevalence of diabetes in a suburban population of Bangladesh. Diabetes Res Clin Pract. 1997;34:149-155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Hussain A, Rahim MA, Azad Khan AK, Ali SM, Vaaler S. Type 2 diabetes in rural and urban population: diverse prevalence and associated risk factors in Bangladesh. Diabet Med. 2005;22:931-936. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 77] [Cited by in F6Publishing: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Pan XR, Yang WY, Li GW, Liu J. Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care. 1997;20:1664-1669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 371] [Cited by in F6Publishing: 373] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 5. | Dong Y, Gao W, Nan H, Yu H, Li F, Duan W, Wang Y, Sun B, Qian R, Tuomilehto J. Prevalence of Type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabet Med. 2005;22:1427-1433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 76] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090-1101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2186] [Cited by in F6Publishing: 2265] [Article Influence: 161.8] [Reference Citation Analysis (2)] |
| 7. | Cockram CS, Woo J, Lau E, Chan JC, Chan AY, Lau J, Swaminathan R, Donnan SP. The prevalence of diabetes mellitus and impaired glucose tolerance among Hong Kong Chinese adults of working age. Diabetes Res Clin Pract. 1993;21:67-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 76] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Janus ED, Watt NM, Lam KS, Cockram CS, Siu ST, Liu LJ, Lam TH. The prevalence of diabetes, association with cardiovascular risk factors and implications of diagnostic criteria (ADA 1997 and WHO 1998) in a 1996 community-based population study in Hong Kong Chinese. Hong Kong Cardiovascular Risk Factor Steering Committee. American Diabetes Association. Diabet Med. 2000;17:741-745. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 97] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Ramachandran A, Snehalatha C, Dharmaraj D, Viswanathan M. Prevalence of glucose intolerance in Asian Indians. Urban-rural difference and significance of upper body adiposity. Diabetes Care. 1992;15:1348-1355. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 210] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 10. | Ramachandran A, Mary S, Yamuna A, Murugesan N, Snehalatha C. High prevalence of diabetes and cardiovascular risk factors associated with urbanization in India. Diabetes Care. 2008;31:893-898. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 195] [Cited by in F6Publishing: 219] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 11. | Waspadji S, Ranakusuma AB, Suyono S, Supartondo S, Sukaton U. Diabetes mellitus in an urban population in Jakarta, Indonesia. Tohoku J Exp Med. 1983;141 Suppl:219-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Sutanegara D, Budhiarta AA. The epidemiology and management of diabetes mellitus in Indonesia. Diabetes Res Clin Pract. 2000;50 Suppl 2:S9-S16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Song KH, Nam-Goomg IS, Han SM, Kim MS, Lee EJ, Lee YS, Lee MS, Yoon S, Lee KU, Park JY. Change in prevalence and 6-year incidence of diabetes and impaired fasting glucose in Korean subjects living in a rural area. Diabetes Res Clin Pract. 2007;78:378-384. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Zaini A. Where is Malaysia in the midst of the Asian epidemic of diabetes mellitus? Diabetes Res Clin Pract. 2000;50 Suppl 2:S23-S28. [PubMed] [Cited in This Article: ] |
| 15. | World Health Organization, Disease Control Division, Ministry of Health Malaysia. NCD risk factors in Malaysia. Available from: http: //www.who.int/chp/steps/MalaysiaSTEPSReport.pdf. Accessibility verified April 23, 2009. [Cited in This Article: ] |
| 16. | Sasaki H, Kawasaki T, Ogaki T, Kobayashi S, Itoh K, Yoshimizu Y, Sharma S, Acharya GP. The prevalence of diabetes mellitus and impaired fasting glucose/glycaemia (IFG) in suburban and rural Nepal-the communities--based cross-sectional study during the democratic movements in 1990. Diabetes Res Clin Pract. 2005;67:167-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Singh DL, Bhattarai MD. High prevalence of diabetes and impaired fasting glycaemia in urban Nepal. Diabet Med. 2003;20:170-171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Ono K, Limbu YR, Rai SK, Kurokawa M, Yanagida J, Rai G, Gurung N, Sharma M, Rai CK. The prevalence of type 2 diabetes mellitus and impaired fasting glucose in semi-urban population of Nepal. Nepal Med Coll J. 2007;9:154-156. [PubMed] [Cited in This Article: ] |
| 19. | Shera AS, Jawad F, Maqsood A. Prevalence of diabetes in Pakistan. Diabetes Res Clin Pract. 2007;76:219-222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 20. | Baltazar JC, Ancheta CA, Aban IB, Fernando RE, Baquilod MM. Prevalence and correlates of diabetes mellitus and impaired glucose tolerance among adults in Luzon, Philippines. Diabetes Res Clin Pract. 2004;64:107-115. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Thai AC, Yeo PP, Lun KC, Hughes K, Ng WY, Lui KF, Cheah JS. Diabetes mellitus and its chronic complications in Singapore: an increasing healthcare problem. Ann Acad Med Singapore. 1990;19:517-523. [PubMed] [Cited in This Article: ] |
| 22. | Tan CE, Emmanuel SC, Tan BY, Jacob E. Prevalence of diabetes and ethnic differences in cardiovascular risk factors. The 1992 Singapore National Health Survey. Diabetes Care. 1999;22:241-247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 150] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 23. | Ministry of Health. WHO Global Infobase: National Health Survey 2004, Singapore. Available from: http: //www.who.int/infobase/. Accessed March 31, 2009. [Cited in This Article: ] |
| 24. | Fernando DJ, Siribaddana S, de Silva D. Impaired glucose tolerance and diabetes mellitus in a suburban Sri Lankan community. Postgrad Med J. 1994;70:347-349. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Katulanda P, Constantine GR, Mahesh JG, Sheriff R, Seneviratne RD, Wijeratne S, Wijesuriya M, McCarthy MI, Adler AI, Matthews DR. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka--Sri Lanka Diabetes, Cardiovascular Study (SLDCS). Diabet Med. 2008;25:1062-1069. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 156] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 26. | Aekplakorn W, Stolk RP, Neal B, Suriyawongpaisal P, Chongsuvivatwong V, Cheepudomwit S, Woodward M. The prevalence and management of diabetes in Thai adults: the international collaborative study of cardiovascular disease in Asia. Diabetes Care. 2003;26:2758-2763. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 88] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | Aekplakorn W, Abbott-Klafter J, Premgamone A, Dhanamun B, Chaikittiporn C, Chongsuvivatwong V, Suwanprapisa T, Chaipornsupaisan W, Tiptaradol S, Lim SS. Prevalence and management of diabetes and associated risk factors by regions of Thailand: Third National Health Examination Survey 2004. Diabetes Care. 2007;30:2007-2012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Chou P, Chen HH, Hsiao KJ. Community-based epidemiological study on diabetes in Pu-Li, Taiwan. Diabetes Care. 1992;15:81-89. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 47] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Lu FH, Yang YC, Wu JS, Wu CH, Chang CJ. A population-based study of the prevalence and associated factors of diabetes mellitus in southern Taiwan. Diabet Med. 1998;15:564-572. [PubMed] [Cited in This Article: ] |
| 30. | Quoc PS, Charles MA, Cuong NH, Lieu LH, Tuan NA, Thomas M, Balkau B, Simon D. Blood glucose distribution and prevalence of diabetes in Hanoi (Vietnam). Am J Epidemiol. 1994;139:713-722. [PubMed] [Cited in This Article: ] |
| 31. | Duc Son LN, Kusama K, Hung NT, Loan TT, Chuyen NV, Kunii D, Sakai T, Yamamoto S. Prevalence and risk factors for diabetes in Ho Chi Minh City, Vietnam. Diabet Med. 2004;21:371-376. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Duc Son LN; UN. World population prospects: the 2007 revision population database. Available from: http: //esa.un.org/unup (accessed April 10, 2009). [Cited in This Article: ] |
| 33. | Gao WG, Dong YH, Pang ZC, Nan HR, Zhang L, Wang SJ, Ren J, Ning F, Qiao Q. Increasing trend in the prevalence of Type 2 diabetes and pre-diabetes in the Chinese rural and urban population in Qingdao, China. Diabet Med. 2009;26:1220-1227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 34. | Sicree R, Shaw J, Zimmet P. Prevalence and projections. Diabetes Atlas International Diabetes Federation. 3rd ed. Brussels: International Diabetes Federation 2006; 16-104. [Cited in This Article: ] |
| 35. | Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, Bhansali A, Joshi SR, Joshi PP, Yajnik CS. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022-3027. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 433] [Cited by in F6Publishing: 462] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 36. | Chow CK, Raju PK, Raju R, Reddy KS, Cardona M, Celermajer DS, Neal BC. The prevalence and management of diabetes in rural India. Diabetes Care. 2006;29:1717-1718. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 37. | Mohan V, Mathur P, Deepa R, Deepa M, Shukla DK, Menon GR, Anand K, Desai NG, Joshi PP, Mahanta J. Urban rural differences in prevalence of self-reported diabetes in India--the WHO-ICMR Indian NCD risk factor surveillance. Diabetes Res Clin Pract. 2008;80:159-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 156] [Cited by in F6Publishing: 174] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 38. | Gupta R, Misra A. Type 2 diabetes in India: Regional disporaties. Br J Diabetes Vasc Dis. 2007;7:12-16. [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 39. | Katikireddi SV, Morling JR, Bhopal R. Is there a divergence in time trends in the prevalence of impaired glucose tolerance and diabetes? A systematic review in South Asian populations. Int J Epidemiol. 2011;40:1542-1553. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Nakagami T, Qiao Q, Carstensen B, Nhr-Hansen C, Hu G, Tuomilehto J, Balkau B, Borch-Johnsen K. Age, body mass index and Type 2 diabetes-associations modified by ethnicity. Diabetologia. 2003;46:1063-1070. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 137] [Cited by in F6Publishing: 142] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 41. | Gu D, Reynolds K, Duan X, Xin X, Chen J, Wu X, Mo J, Whelton PK, He J. Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia (InterASIA). Diabetologia. 2003;46:1190-1198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 307] [Cited by in F6Publishing: 315] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 42. | Ng MC, Lee SC, Ko GT, Li JK, So WY, Hashim Y, Barnett AH, Mackay IR, Critchley JA, Cockram CS. Familial early-onset type 2 diabetes in Chinese patients: obesity and genetics have more significant roles than autoimmunity. Diabetes Care. 2001;24:663-671. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 60] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 43. | Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Type 2 diabetes in Asian-Indian urban children. Diabetes Care. 2003;26:1022-1025. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 86] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 44. | Gill T. Young people with diabetes and obesity in Asia: a growing epidemic. Diabetes Voice. 2007;52:20-22. [Cited in This Article: ] |
| 45. | Ma RC, Chan JC. Pregnancy and diabetes scenario around the world: China. Int J Gynaecol Obstet. 2009;104 Suppl 1:S42-S45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 46. | Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375:408-418. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 519] [Cited by in F6Publishing: 537] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 47. | Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009;301:2129-2140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1411] [Cited by in F6Publishing: 1433] [Article Influence: 95.5] [Reference Citation Analysis (0)] |
| 48. | Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997-2008. Diabetes Care. 2011;34:353-357. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 206] [Cited by in F6Publishing: 226] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 49. | Shelgikar KM, Hockaday TD, Yajnik CS. Central rather than generalized obesity is related to hyperglycaemia in Asian Indian subjects. Diabet Med. 1991;8:712-717. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 66] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 50. | Lear SA, Humphries KH, Kohli S, Chockalingam A, Frohlich JJ, Birmingham CL. Visceral adipose tissue accumulation differs according to ethnic background: results of the Multicultural Community Health Assessment Trial (M-CHAT). Am J Clin Nutr. 2007;86:353-359. [PubMed] [Cited in This Article: ] |
| 51. | Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86:5366-5371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 95] [Cited by in F6Publishing: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 52. | Chandalia M, Abate N, Garg A, Stray-Gundersen J, Grundy SM. Relationship between generalized and upper body obesity to insulin resistance in Asian Indian men. J Clin Endocrinol Metab. 1999;84:2329-2335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 102] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 53. | Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681-1688. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1114] [Cited by in F6Publishing: 1094] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 54. | Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in asian Indian adults. Diabetes Care. 2003;26:1380-1384. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 273] [Cited by in F6Publishing: 282] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 55. | WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7065] [Cited by in F6Publishing: 7846] [Article Influence: 392.3] [Reference Citation Analysis (0)] |
| 56. | Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298:2654-2664. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 849] [Cited by in F6Publishing: 845] [Article Influence: 49.7] [Reference Citation Analysis (2)] |
| 57. | Barrett-Connor E, Khaw KT. Cigarette smoking and increased central adiposity. Ann Intern Med. 1989;111:783-787. [PubMed] [Cited in This Article: ] |
| 58. | Yajnik CS. Nutrient-mediated teratogenesis and fuel-mediated teratogenesis: two pathways of intrauterine programming of diabetes. Int J Gynaecol Obstet. 2009;104 Suppl 1:S27-S31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 58] [Cited by in F6Publishing: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 59. | Neel JV. Diabetes mellitus: a "thrifty" genotype rendered detrimental by "progress"? 1962. Bull World Health Organ. 1999;77:694-703; discussion 692-693. [PubMed] [Cited in This Article: ] |
| 60. | Gluckman PD, Hanson MA, Bateson P, Beedle AS, Law CM, Bhutta ZA, Anokhin KV, Bougnères P, Chandak GR, Dasgupta P. Towards a new developmental synthesis: adaptive developmental plasticity and human disease. Lancet. 2009;373:1654-1657. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 301] [Cited by in F6Publishing: 259] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 61. | Norris SA, Osmond C, Gigante D, Kuzawa CW, Ramakrishnan L, Lee NR, Ramirez-Zea M, Richter LM, Stein AD, Tandon N. Size at birth, weight gain in infancy and childhood, and adult diabetes risk in five low- or middle-income country birth cohorts. Diabetes Care. 2012;35:72-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 62. | Gerstein HC, Islam S, Anand S, Almahmeed W, Damasceno A, Dans A, Lang CC, Luna MA, McQueen M, Rangarajan S. Dysglycaemia and the risk of acute myocardial infarction in multiple ethnic groups: an analysis of 15,780 patients from the INTERHEART study. Diabetologia. 2010;53:2509-2517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 63. | UK Prospective Diabetes Study (UKPDS) group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications with subjects with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837-853. [DOI] [Cited in This Article: ] [Cited by in Crossref: 14327] [Cited by in F6Publishing: 12489] [Article Influence: 480.3] [Reference Citation Analysis (0)] |
| 64. | Geiss LS, Herman WH, Smith PJ. Mortality in non-insulin dependent diabetes. Diabetes in America. 2nd ed. Bethesda: National Institutes of Health 1995; 233-255. [Cited in This Article: ] |
| 65. | Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353:2643-2653. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3538] [Cited by in F6Publishing: 3369] [Article Influence: 177.3] [Reference Citation Analysis (0)] |
| 66. | Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577-1589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5314] [Cited by in F6Publishing: 5134] [Article Influence: 320.9] [Reference Citation Analysis (0)] |
| 67. | Kapur A. Economic analysis of diabetes care. Indian J Med Res. 2007;125:473-482. [PubMed] [Cited in This Article: ] |
| 68. | Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, Kapur A, Williams R. Increasing expenditure on health care incurred by diabetic subjects in a developing country: a study from India. Diabetes Care. 2007;30:252-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 135] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 69. | Chan JC, Gagliardino JJ, Baik SH, Chantelot JM, Ferreira SR, Hancu N, Ilkova H, Ramachandran A, Aschner P. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care. 2009;32:227-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 214] [Cited by in F6Publishing: 220] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 70. | Pratley RE, Matfin G. Pre-diabetes: Clinical Relevance and Therapeutic Approach. Br J Diab and Vasc Dis. 2007;7:120-129. [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 71. | Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537-544. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2773] [Cited by in F6Publishing: 2550] [Article Influence: 94.4] [Reference Citation Analysis (1)] |
| 72. | Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49:289-297. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1219] [Cited by in F6Publishing: 1161] [Article Influence: 64.5] [Reference Citation Analysis (0)] |
| 73. | Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008;371:1783-1789. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1074] [Cited by in F6Publishing: 1008] [Article Influence: 63.0] [Reference Citation Analysis (0)] |
| 74. | Ramachandran A, Snehalatha C. Diabetes prevention and control programs in developing countries. Diabetes Public Health. Oxford: Oxford University Press 2011; 603-621. [Cited in This Article: ] |