Copyright
©The Author(s) 2022.
World J Gastrointest Oncol. Sep 15, 2022; 14(9): 1758-1770
Published online Sep 15, 2022. doi: 10.4251/wjgo.v14.i9.1758
Published online Sep 15, 2022. doi: 10.4251/wjgo.v14.i9.1758
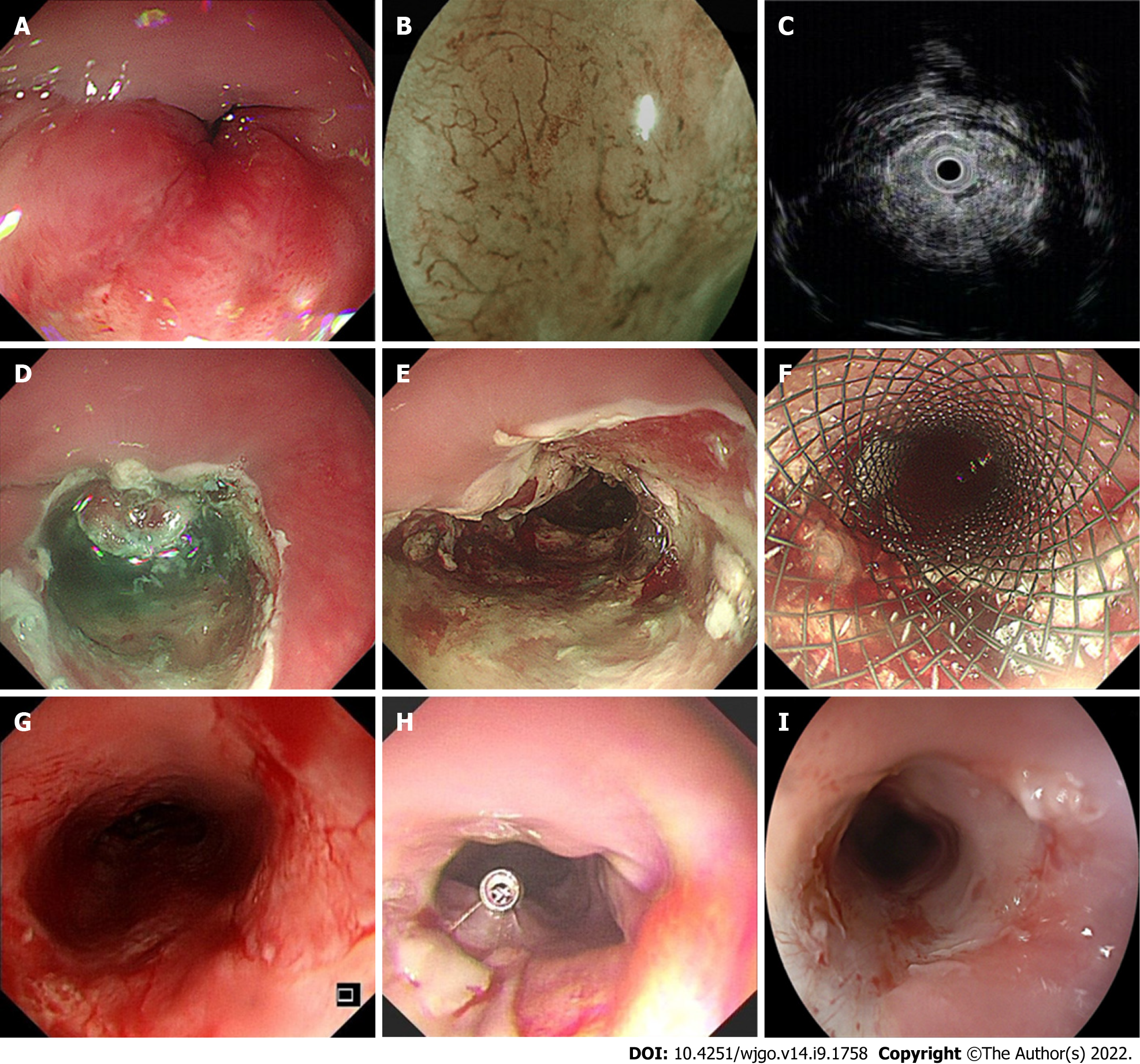
Figure 1 Technical notes of endoscopic debulking resection.
This is a typical case from our study, A: An irregular, protruding neoplasm was seen in the esophagus 21 cm away from the incisor, occupying approximately 2/3 of the circumference of the lumen, and the endoscope could not pass through; B: Blue laser imaging magnification showed the type B2 intrapapillary capillary loop vessel in the lesion, with small aortic valve area observed; C: Endoscopic ultrasonography showed hypoechogenicity, an obvious thick mucosal layer and a submucosal layer. The submucosal layer of the lesion was discontinuous and involved the muscularis propria; D: A mixture of saline solution diluted with methylthionine chloride and epinephrine was injected into the lesion, and then incision of the lesion was made using the Dual-Knife; E: The final wound was hemostatically treated; F: A fully covered esophageal stent was finally implanted; G: One month later, the stent was removed endoscopically; H: After another week, the lumen of the endoscopic resection was slightly narrowed, but the ordinary gastroscope was still passable. A titanium clip was used to mark the lesion for later radiotherapy positioning; I: Six months of follow-up after chemoradiotherapy showed slight narrowing of the lumen of the esophagus.
- Citation: Ren LH, Zhu Y, Chen R, Shrestha Sachin M, Lu Q, Xie WH, Lu T, Wei XY, Shi RH. Endoscopic debulking resection with additive chemoradiotherapy: Optimal management of advanced inoperable esophageal squamous cell carcinoma. World J Gastrointest Oncol 2022; 14(9): 1758-1770
- URL: https://www.wjgnet.com/1948-5204/full/v14/i9/1758.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i9.1758