Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.274
Peer-review started: August 29, 2014
First decision: October 28, 2014
Revised: December 16, 2014
Accepted: January 9, 2015
Article in press: January 12, 2015
Published online: March 16, 2015
Processing time: 204 Days and 20.6 Hours
Large bile duct stone (> 10 mm) or multiple stones (≥ 3) are challenging for endoscopists. Endoscopic sphincterotomy (EST) is a routine therapeutic endoscopic retrograde cholangiopancreatography (ERCP) procedure usually used. It is safe and effective, but severe perforation or massive bleeding are the main causes of mortality. Because of the permanent destroy of Oddi sphincter, the use of EST is still controversial. Endoscopic papillary balloon dilation (EPBD) gives another way to open the sphincter. Less incidence of bleeding, perforation and partly preserving the Oddi sphincter’s function are the main advantages. But high incidence of post-ERCP pancreatitis becomes a predominant problem. According to the anatomical feature of Oddi sphincter, limited EST + EPBD seems a more reasonable procedure. Compared to the former two procedures, it makes the stone extraction process much easier with lower incidences of short-term and long-term complications.
Core tip: This review describes endoscopic sphincterotomy (EST), endoscopic papillary balloon dilation (EPBD) and limited EST + EPBD in the treatment of difficult bile duct stones. We analyze the advantages and disadvantages of these procedures from a unique anatomic view. Limited EST + EPBD may be the most reasonable procedure with the highest successful rate and the lowest incidence of complications.
- Citation: Ding J, Li F, Zhu HY, Zhang XW. Endoscopic treatment of difficult extrahepatic bile duct stones, EPBD or EST: An anatomic view. World J Gastrointest Endosc 2015; 7(3): 274-277
- URL: https://www.wjgnet.com/1948-5190/full/v7/i3/274.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i3.274
Endoscopic sphincterotomy (EST) which was developed from the 70’s of last century has been widely used in therapeutic endoscopic retrograde cholangiopancreatography (ERCP) for a few decades. It is a safe and effective method for the treatment of extrahepatic bile duct stones. Although the short-term complications are decreased with the development of technique and equipment, massive bleeding and perforation are still the main causes for patients’ death. As an operation which destroys the Oddi sphincter permanently, the use of EST is controversial. The long -term complications, such as intestinal content reflux, biliary tract inflammation and stone recurrence, are the grounds of argument for those who object the use of EST. In 1982, Staritz treated common bile duct stones by endoscopic papillary balloon dilation (EPBD) successfully. Since then, many authors published reports on the benefits of EPBD and their outcome were almost comparable to EST. Compared with EST, EPBD was easier to operate and of less incidence of bleeding and perforation. Most of all, it might preserve the function of the Oddi sphincter. But soon the high incidence of post ERCP pancreatitis (PEP) reported by DiSario et al[1] and his colleagues after a series of multicenter studies questioned the value of this technique. Their results showed that 15%-20% patients developed PEP after EPBD and 2 patients died of severe pancreatitis and EPBD was the only reason for PEP. Incomplete dilation of the papilla, intra-mucosal bleeding and local edema were thought to be the main causes. Due to the high risk of PEP, most of the endoscopists in North America abandoned this method. But EPBD was still used in Europe and East Asia. Recently some authors report that with large balloon (≥ 10 mm) and long term (3 to 5 min) could prominently decreased the incidence of PEP after EPBD compared to the traditional small balloon and short term (< 1 min) procedure. More recent reports recommend the combination of limited EST + EPBD and it seems to be a more reasonable technique.
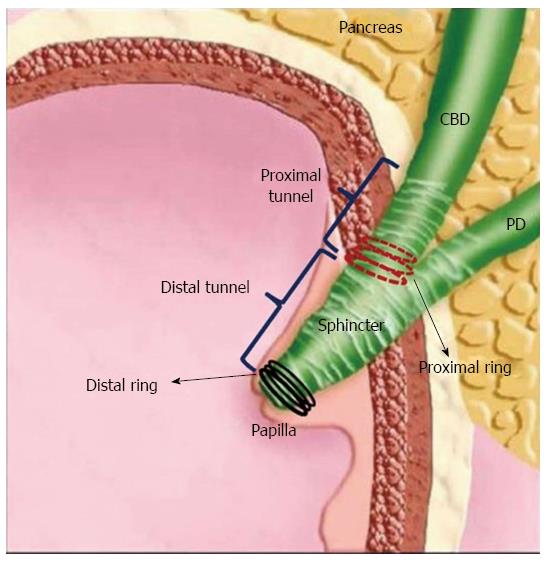
The treatment of a large bile duct stone (> 10 mm) or multiple stones sometimes appears to be a difficult experience for endoscopists. How to get the opening as wide as possible is the key factor for a successful treatment. To understand the difference between these 3 techniques, some further understanding should be made on the anatomy of the Oddi sphincter. It is a very complicated muscle structure which is composed of sphincter choledochus, sphincter pancreaticus, sphincter ampullae and some longitudinal bundles. In most human beings, the muscle fibers around the orifice of the papilla and the one passing through the duodenum wall are dense and thick. They are the main barrier for stone extraction like two dense rings in the papilla (Figure 1).
It is usually defined that the tunnel starts from the distal portion of the bile duct to the orifice of the papilla as the stone extraction tunnel (SET). Based upon the anatomy described above, we divide the tunnel into two segments: the distal bile duct and the intra-mural portion of the Oddi sphincter constitute the proximal segment, which contains the proximal ring, and the intra-duodenal portion of the papilla forms the distal segment which contains the distal ring around the orifice (Figure 1). EST, EPBD and limited EST + EPBD have different effects on that tunnel. Traditional EST cuts almost the entire distal segment from the orifice up close to the duodenal wall. EPBD dilates the total SET. Limited EST opens the distal portion of the intraluminal papilla and at the same time EPBD dilates the rest portion. Analyzing based on our “2-ring” theory, EST opens the distal ring, shortens SET while does nothing on the proximal ring. EPBD dilates the entire SET including 2 rings but keep the whole structure intact. Limited EST + EPBD cut the distal ring to shorten SET and dilate the proximal ring as well. So the combination procedure may be better to access a wide opening of SET from the anatomical view.
Poincloux et al[2] studied 64 cases of limited EST + EPBD for difficult bile duct stones retrospectively. The successful rate in the first attempt was 95.3% without the use of mechanical lithotripsy (ML). Stefanidis et al[3] did a prospective study on EST + EPBD and EST + ML for the treatment of large stones (> 12 mm). There was no difference between the two groups of the successful rate in the first attempt (97.7% vs 91.1%, P > 0.05). It was concluded that EST + EPBD decreased the frequency of ML usage. Another RCT study[4] shows that there’s no difference on the successful rate between limited EST+EPBD and EST group. However, the frequency of ML usage is much lower in the former group (28.8% vs 46.2%, P = 0.028) and the difference becomes more prominent when the diameter of the stones are beyond 15 mm (58.1% vs 90.9%, P = 0.002).
Reviewing the recent 5-year reports on simple EPBD in treating difficult bile duct stones, the successful rate in the first attempt was 65.8%-92.7% and ML was frequently used[5-8], which indicates the effects are not as good as EST and EST + EPBD.
Although most of post-ERCP pancreatitis (PEP) cases are mild, it is a common early complication after ERCP intervention. Studies on early EPBD treatment showed a higher incidence of PEP when compared with EST, especially for the severe PEP. Obstruction of the outflow of pancreas aroused by intra-mucosa bleeding and/or local edema after EPBD is assumed to be the main cause. But some authors think that the procedures before EPBD, such as difficult cannulation, guidewire runing into the pancreatic duct repeatedly, opacification of the pancreatic duct or even ML are the key factors for PEP. To prove this hypothesis, Seo et al[9] designed an interesting study. Fifty-six antegrade balloon dilation of the papilla through the PTCD method were done for the treatment of common bile duct stones. Two hundred and eight cases of EPBD of the same period were put into the control group. Except for 4 cases of hyperamylasemia, there was no pancreatitis in the experimental group, but the PEP and hyperamylasemia rate was 6.7% (including 1 severe type) and 29.8% respectively in control group. But this hypothesis can’t explain why there is a lower incidence of PEP in the EST group when the similar pre-EPBD procedures exists. Reviewing some early reports on EPBD, we can find that the incidence of PEP was as high as 15%-20%. Most of these studies utilized short-term (< 1 min) dilation of the Oddi sphincter with small diameter balloons. Incomplete dilations brought difficulties in stone extraction and resulted in high incidence of ML usage. The subsequent intra-mucosa bleeding and/or local edema around the pancreatic orifice became the main cause of pancreatic outflow obstruction and thus PEP. Comparing to the incomplete short-term dilation with small balloons, EST shortens SET and makes a wider opening which facilitates stone extraction. Therefore, it leads to less edema and eventually a lower incidence of PEP.
Recently, there has been a great development in the EPBD therapy. Long term (3-5 min) dilation with large balloon (12-20 mm) is replacing the old method. Complete dilation results in a total paralysis of the sphincter. It not only makes the extraction easier, but also guarantees a patent bilio-pancreatic outflow for a period of time. Limited EST with long-term large balloon dilation is more widely accepted now, especially in East Asia. This operation is recommended for that it not only opens the distal ring to shorten SET, but also dilates the proximal ring. The bilio-pancreatic outflow is more patent than that made by EST because EST has done nothing to the proximal ring. Although it is called “limited”, the cutting edge can usually reach or even exceed the pancreatic orifice. So the subsequent balloon stress maybe only focused on the proximal ring, which may alleviate the extent of edema around the pancreatic orifice.
The recent reports on large balloon and long-term EPBD with or without EST indicate that the incidence of PEP is 5% and there’s no significant difference when compares to EST. Park et al[10] published a multicenter retrospective studying which EPBD with or without limited EST were used to treat 964 cases of large (> 10 mm) common bile duct stones. Their result confirms that the incidence of PEP has an inverse correlation to the diameter of the balloon. We don’t agree that “the bigger, the better” can be the principle for choosing a balloon caliber. The common consensus is that the adequate diameter of a balloon should at least be equal to that of the biggest stone. Furthermore, EPBD is not recommended for the patients without bile duct dilation and those with distal bile duct stricture[10].
The incidence of bleeding after EST is about 0.8%-2%. Radiologic intervention or surgery may be necessary when massive bleeding occurs. Cirrhosis, coagulopathy and anti-coagulant taking are the contraindications for EST. The early purpose of replacing EST with EPBD is to avoid bleeding and perforation. In Japan, Takahara et al[11] reported a 37-case group of bile duct stone patients who were undertaking hemodialysis. Only 2 (5.4%) patients developed bleeding after EPBD. When reviewing the recent Meta-analysis comparing EST and EPBD, it is showed that EST has a higher incidence of bleeding.
According to the anatomy of vessel distribution around Oddi sphincter, the small vessels are usually located at the roof of the papilla just close to the duodenal wall. The territory from 11 o’clock to 1 o’clock direction is recommended for a safe EST. In order to get a large outlet for stone extraction, total EST is recommended to extend the incision up close to the duodenal wall, as a result bleeding cannot be totally avoided. Limited EST only cut the distal ring and leave the proximal portion intact to keep a distance from these vessels, so bleeding is rare. Park’s et al[10] study demonstrated this hypothesis. They found that complete EST or limited EST is the independent factor that influences the incidence of post-operative bleeding (OR 6.22, P < 0.001).
Although the incidence of bleeding after EPBD or limited EST + EPBD is low, the result is unacceptable. Excessive cutting, distal bile duct stricture or inadequate use of a large balloon are the main factors for tearing the mucosa of the lower bile duct apart. Because the location of the bleeding vessels is very high as described, the uncut structure after EPBD or limited EST + EPBD prevent the endoscopists from visualizing the bleeding point directly under the scope. And finally, there may be multiple bleeding exists when the mucosa is torn apart. These factors make the diagnosis and treatment much challenging. Recurrent hemorrhage is common after radiologic intervention or even surgery. Fully covered metal stent maybe useful in this situation.
Besides the advantages for less bleeding and less perforation, preserving the function of Oddi sphincter is another goal of EPBD. According to Kojima’s[12] excellent manometry study on patients’ sphincter before and after EPBD, he concluded that 70% of the sphincter function was preserved after EPBD.
Changes of bile composition and bacterial infection are well-known causes for bile duct stone formation. But little is known in present about the role of biliary dynamics. We believe that it takes great part in the pathogenesis of choledocholithiasis or even cholecystolithiasis.
The normal functions of Oddi sphincter are: (1) to provide a patent pathway for bile excretion; and (2) to prevent bowel reflux. Either disorder in these 2 aspects may result in stone formation. If the etiology is due to an inadequate patency, EST maybe the correct choice; while if bowel reflux is the main problem, such as the para-papilla diverticulum, it may be more reasonable to do EPBD. Some further evidence-based studies was needed on these interesting topics. But above all, development in atraumatic and repeatable diagnostic methods to evaluate the status of Oddi sphincter was looking forward.
In summary, EST + EPBD is a reasonable procedure for difficult bile duct stones. It makes a wide opening of the Oddi sphincter to ensure a high success rate of stone extraction with lower incidence of PEP, bleeding and perforation. The long-term results need further researches on the dynamics study of the biliary tract, especially the Oddi sphincter.
P- Reviewer: Gornals JB, Rustagi T S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291-1299. [Cited in This Article: ] |
| 2. | Poincloux L, Rouquette O, Privat J, Gorce D, Abergel A, Dapoigny M, Bommelaer G. Large-balloon dilation of the sphincter of Oddi after sphincterotomy or infundibulotomy to extract large calculi or multiple common bile duct stones without using mechanical lithotripsy. Scand J Gastroenterol. 2013;48:246-251. [Cited in This Article: ] |
| 3. | Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278-285. [Cited in This Article: ] |
| 4. | Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, Chiu PW, Wong SK, Chan FK, Lau JY. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology. 2013;144:341-345.e1. [Cited in This Article: ] |
| 5. | Kuo CM, Chiu YC, Changchien CS, Tai WC, Chuah SK, Hu TH, Kuo YH, Kuo CH. Endoscopic papillary balloon dilation for removal of bile duct stones: evaluation of outcomes and complications in 298 patients. J Clin Gastroenterol. 2012;46:860-864. [Cited in This Article: ] |
| 6. | Youn YH, Lim HC, Jahng JH, Jang SI, You JH, Park JS, Lee SJ, Lee DK. The increase in balloon size to over 15 mm does not affect the development of pancreatitis after endoscopic papillary large balloon dilatation for bile duct stone removal. Dig Dis Sci. 2011;56:1572-1577. [Cited in This Article: ] |
| 7. | Chan HH, Lai KH, Lin CK, Tsai WL, Wang EM, Hsu PI, Chen WC, Yu HC, Wang HM, Tsay FW. Endoscopic papillary large balloon dilation alone without sphincterotomy for the treatment of large common bile duct stones. BMC Gastroenterol. 2011;11:69. [Cited in This Article: ] |
| 8. | Jeong S, Ki SH, Lee DH, Lee JI, Lee JW, Kwon KS, Kim HG, Shin YW, Kim YS. Endoscopic large-balloon sphincteroplasty without preceding sphincterotomy for the removal of large bile duct stones: a preliminary study. Gastrointest Endosc. 2009;70:915-922. [Cited in This Article: ] |
| 9. | Seo YR, Moon JH, Choi HJ, Kim DC, Lee TH, Cha SW, Cho YD, Park SH, Kim SJ. Papillary balloon dilation is not itself a cause of post-endoscopic retrograde cholangiopancreatography pancreatitis; results of anterograde and retrograde papillary balloon dilation. J Gastroenterol Hepatol. 2013;28:1416-1421. [Cited in This Article: ] |
| 10. | Park SJ, Kim JH, Hwang JC, Kim HG, Lee DH, Jeong S, Cha SW, Cho YD, Kim HJ, Kim JH. Factors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter series. Dig Dis Sci. 2013;58:1100-1109. [Cited in This Article: ] |
| 11. | Takahara N, Isayama H, Sasaki T, Tsujino T, Toda N, Sasahira N, Mizuno S, Kawakubo K, Kogure H, Yamamoto N. Endoscopic papillary balloon dilation for bile duct stones in patients on hemodialysis. J Gastroenterol. 2012;47:918-923. [Cited in This Article: ] |
| 12. | Kojima Y, Nakagawa H, Miyata A, Hirai T, Ohyama I, Okada A, Hiramatsu T, Ohhara Y, Kuwahara T. Long-term prognosis of bile duct stones: endoscopic papillary balloon dilatation versus endoscopic sphincterotomy. Dig Endosc. 2010;22:21-24. [Cited in This Article: ] |