Published online Apr 16, 2023. doi: 10.4253/wjge.v15.i4.297
Peer-review started: December 17, 2022
First decision: January 12, 2023
Revised: January 23, 2023
Accepted: March 17, 2023
Article in press: March 17, 2023
Published online: April 16, 2023
Gastrointestinal bleeding (GIB) is a serious health problem worldwide, particularly during childhood. This can be an alarming sign of an underlying disease. Gastrointestinal endoscopy (GIE) is a safe method for the diagnosis and treatment of GIB in most cases.
To determine the incidence, clinical presentation, and outcomes of GIB in children in Bahrain over the last two decades.
This was a retrospective cohort review of the medical records of children with GIB who underwent endoscopic procedures in the Pediatric Department at Salmaniya Medical Complex, Bahrain, between 1995 and 2022. Demographic data, clinical presentation, endoscopic findings, and clinical outcomes were recorded. GIB was classified into upper (UGIB) and lower (LGIB) GIB according to the site of bleeding. These were compared with respect to patients’ sex, age, and nationality using the Fisher’s exact, Pearson’s χ2, or the Mann-Whitney U tests.
A total of 250 patients were included in this study. The median incidence was 2.6/100000 per year (interquartile range, 1.4-3.7) with a significantly increasing trend over the last two decades (P < 0.0001). Most patients were males (n = 144, 57.6%). The median age at diagnosis was 9 years (5–11). Ninety-eight (39.2%) patients required upper GIE alone, 41 (16.4%) required colonoscopy alone, and 111 (44.4%) required both. LGIB was more frequent (n = 151, 60.4%) than UGIB (n = 119, 47.6%). There were no significant differences in sex (P = 0.710), age (P = 0.185), or nationality (P = 0.525) between the two groups. Abnormal endoscopic findings were detected in 226 (90.4%) patients. The common cause of LGIB was inflammatory bowel disease (IBD) (n = 77, 30.8%). The common cause of UGIB was gastritis (n = 70, 28%). IBD and undetermined cause for bleeding were higher in the 10–18 years group (P = 0.026 and P = 0.017, respectively). Intestinal nodular lymphoid hyperplasia, foreign body ingestion, and esophageal varices were more common in the 0–4 years group (P = 0.034, P < 0.0001, and P = 0.029, respectively). Ten (4%) patients underwent one or more therapeutic interventions. The median follow-up period was two years (0.5-3). No mortality was reported in this study.
GIB in children is an alarming condition, whose significance is increasing. LGIB, commonly due to IBD, was more common than UGIB, commonly due to gastritis.
Core Tip: The incidence, clinical presentation, cause, and outcomes of gastrointestinal bleeding (GIB) in children in Bahrain are unknown. We observed a significant increase in the annual incidence of GIB. Lower GIB (LGIB) was more common than upper GIB (UGIB). The most common cause of LGIB was inflammatory bowel disease. The most common cause of UGIB was gastritis. Causes of GIB varied with patient’s age and differed from that reported in other countries. No mortality was observed in any patient. These findings are essential to tailor management based on the most common causes and patient age.
- Citation: Isa HM, Alkharsi FA, Ebrahim HA, Walwil KJ, Diab JA, Alkowari NM. Causes of gastrointestinal bleeding in children based on endoscopic evaluation at a tertiary care center in Bahrain. World J Gastrointest Endosc 2023; 15(4): 297-308
- URL: https://www.wjgnet.com/1948-5190/full/v15/i4/297.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i4.297
Gastrointestinal (GI) bleeding (GIB) is a serious health problem worldwide, particularly during childhood. It is defined as any kind of hemorrhage or blood loss in the digestive tract, from the mouth to the anus[1], which can range from nearly undetectable to acute, massive, or life-threatening[1]. It is divided into three main clinical forms: Upper GIB (UGIB), lower GIB (LGIB), and bleeding of obscure origin[2]. UGIB and LGIB are defined based on their relationship with the ligament of Treitz[3]. The source of bleeding in UGIB is proximal to the ligament of Treitz (from the upper part of the esophagus to the duodenojejunal flexure), whereas that of LGIB is distal to the ligament (small bowel and colon)[3]. GIB can also be occult, that is, not visible to the patient or physician, leading to either a positive fecal occult blood test or iron-deficiency anemia[3].
GIB can cause anxiety in children, caregivers, and healthcare providers[4] and can be an alarming sign of an underlying disease[5]. GIB has a variety of causes; a good elicitation of patients’ medical history and physical examination can adequately differentiate between macroscopic and microscopic forms of bleeding[5].
GI endoscopy (GIE) is a safe method for the diagnosis and treatment of GIB[4]. GIE can reveal the underlying etiology of GIB in most cases[3]. However, it requires the experience and coordination of the medical team to provide specialized patient care[6].
According to the Italian Society of Pediatric Gastroenterology, the incidence rate of GIB in children is 6.4%[3]. However, there is a paucity of studies regarding the incidence and causes of GIB in the pediatric population in the Middle East. Thus, we aimed to determine the incidence, clinical presentation, causes, and outcomes of GIB in children at the main tertiary hospital in Bahrain over the last two decades. Additionally, we aimed to stratify the causes of GIB based on patient age.
We conducted a retrospective cohort review of all medical records of children diagnosed with GIB in the Pediatric Department at Salmaniya Medical Complex (SMC), Manama, Bahrain, between January 1995 and October 2022. SMC is the only tertiary hospital in Bahrain to where children with GIB are referred for diagnosis and management. Endoscopic procedures were performed in either the endoscopy unit or the main operating theatre. The endoscopy unit in SMC consists of three rooms, in which three pediatric gastroenterology consultants and one chief resident can perform endoscopic procedures. Two types of endoscopic equipment were used: Olympus (PCF-230 and XQ230, Olympus Cooperation, Shinjuku, Tokyo, Japan) and Pentax (EG-2901 and EC-380IF, Pentax Ricoh Imaging Company Ltd, Tokyo, Japan).
All children who were admitted to the pediatric department for GIB and underwent GIE were included in the study. Patients who were discharged from the emergency department and those who did not undergo endoscopic procedures were excluded. Patients were classified as having upper, lower, or both GIB according to their presenting symptoms.
From 1995 to 2010, the data were retrieved from archived paper-based medical records, while from 2010 to 2022, the data were retrieved from the I-Seha electronic medical records. The following demographic data were collected: Year of presentation, sex, nationality, age at diagnosis, and history of associated chronic diseases.
Presenting symptoms, such as hematemesis, melena, and rectal bleeding (hematochezia), were noted. Additional symptoms, including recurrent vomiting or abdominal pain, chest pain, diarrhea, constipation, weight loss, and history of foreign body or caustic ingestion, were noted. Physical findings such as oral ulcers, pallor, jaundice, perianal fistula or fissure, hemorrhoids, and failure to thrive were recorded. A perianal fistula was defined as a small passage that connects an infected gland inside the anus to an opening on the skin around the anus. A perianal fissure is a tear in the anal mucosa. Failure to thrive (thinness) was defined as a weight for age z-score of < 2 standard deviations according to the World Health Organization growth references[7].
Endoscopy data on the type, upper (UGIE) or lower (LGIE) GIE, and the total number of procedures performed were collected. The causes of GIB were based on endoscopic findings, such as Mallory–Weiss syndrome, esophagitis, esophageal ulcer or varices, foreign body ingestion, gastritis, peptic or duodenal ulcer, gastroenteritis, inflammatory bowel disease (IBD), nodular lymphoid hyperplasia, Meckel’s diverticulum, rectal ulcers or polyps, and anal fissures. Data on therapeutic interventions, as well as number of patients who required repeat endoscopic interventions, follow-up duration, and patient outcomes were collected.
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) (version 21; IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp, United States). The annual incidence of GIB was calculated. The 28-year study period was divided into four periods (1995–2001, 2002–2008, 2009–2015 and 2016–2022), which were compared in terms of the mean annual incidence of GIB using a one-way analysis of variance test. Bonferroni post-hoc analysis was used for pairwise multiple comparisons between the four periods. Patient ages were classified into three groups: 0–4, 5–9, and 10–18 years. Categorical variables are presented as frequency and percentage. Continuous variables are presented as median and interquartile range (IQR). UGIB and LGIB were compared with respect to sex, age, and nationality. The causes of GIB were compared according to age group. Fisher’s exact test or Pearson’s χ2 test was used to compare categorical variables, while the Mann–Whitney U test was used to compare continuous variables with a skewed distribution. P values < 0.05 were considered statistically significant.
This study was conducted in accordance with the principles of Helsinki Declaration, and it was ethically approved by the Research and Research Ethics Committee, Salmaniya Medical Complex, Government hospitals, Kingdom of Bahrain (IRB number: 6170122, January 17, 2022).
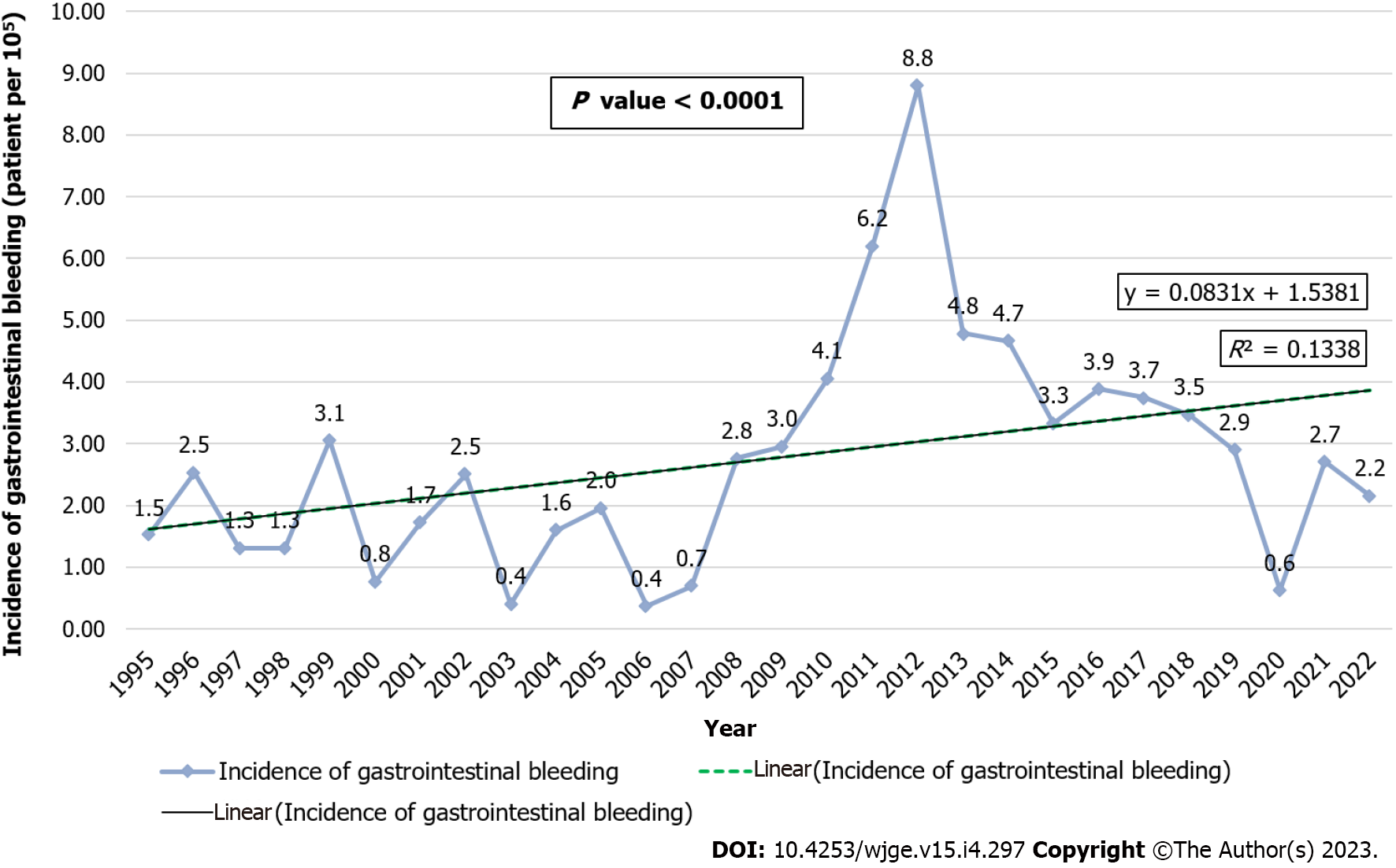
During the study period, 250 children were admitted to the hospital for GIB and underwent a GIE procedure. All the patients were included in this study. According to the 2020 Bahrain Health Statistics, the total population in Bahrain was 1472204, with 481819 people within the pediatric age group (up to 18 years). The median incidence was 2.6/100000 per year (IQR, 1.4–3.7) with an increasing trend (Figure 1). A significant difference in the mean GIB incidence was found between the four periods, [F (3, 24) =10.280, P < 0.0001]. The mean incidence in 2009–2015 was significantly higher (4.9 ± 1.9) than that in 1995–2001 (1.7 ± 0.8), 2002-2008 (1.5 ± 0.9) and 2016-2022 (2.7 ± 1.9) (P = 0.001, P < 0.0001, P = 0.028, respectively). The demographic data of the included patients are shown in Table 1. Most of the patients were males (n = 144, 57.6%). The majority were Bahraini (n = 224, 89.6%), while the rest were non-Bahraini (n = 24, 9.6%) [eight (3.2%) were from India, three (1.2%) from Pakistan, two (0.8%) from Iraq, two (0.8%) from Egypt, one (0.4%) from Oman, one (0.4%) from Qatar, one (0.4%) from Yemen, one (0.4%) from Sudan, one (0.4%) from Syria, one (0.4%) from Sweden, one (0.4%) from Bangladesh, one (0.4%) from China, and one (0.4%) from Philippines]. Two patients (0.8%) were of unspecified nationality. The median age at the time of endoscopic diagnosis was 9 years (IQR, 5–11). The most commonly affected age group was the 10–18 years group (n = 107, 42.8%). Thirty-nine (15.6%) patients had one or more associated diseases that were not considered as a direct cause of GIB. The common associated diseases were gastroesophageal reflux disease (GERD) (n = 7, 2.8%) and celiac disease (n = 7, 2.8%), followed by sickle cell disease (n = 5, 2%), and autoimmune hepatitis (n = 4, 1.6%). Other associated diseases were cerebral palsy (n = 3, 1.2%), mental retardation (n = 3, 1.2%), biliary atresia (n = 2, 0.8%), Wilson’s disease (n = 2, 0.8%), sclerosing cholangitis (n = 2, 0.8%), chronic liver disease with portal hypertension (n = 2, 0.8%), trisomy 21 (n = 2, 0.8%), Ehlers Danlos syndrome (n = 1, 0.4%), familial Mediterranean fever (n = 1, 0.4%), cholecystitis (n = 1, 0.4%), intestinal worms (n = 1, 0.4%), tracheoesophageal fistula (n = 1, 0.4%), liver cirrhosis (n = 1, 0.4%), Turner’s syndrome (n = 1, 0.4%), insulin-dependent diabetes mellitus (n = 1, 0.4%), hydrocephalus (n = 1, 0.4%), glucose-6-phosphate dehydrogenase deficiency (n = 1, 0.4%), congenital heart disease (n = 1, 0.4%), hiatal hernia (n = 1, 0.4%), autoimmune hemolytic anemia (n = 1, 0.4%), food allergy (n = 1, 0.4%) and anorexia nervosa (n = 1, 0.4%).
| Variables | n (%) |
| Sex | |
| Male | 144 (57.6) |
| Female | 106 (42.4) |
| Nationality | |
| Bahraini | 224 (89.6) |
| Non-Bahraini | 24 (9.6) |
| Unspecified | 2 (0.8) |
| Age group (yr) (n = 247) | |
| 0-4 | 58 (23.2) |
| 5–9 | 82 (32.8) |
| 10–18 | 107 (42.8) |
| Type of endoscopy performed | |
| Upper gastrointestinal endoscopy | 98 (39.2) |
| Lower gastrointestinal endoscopy | 41 (16.4) |
| Both types of gastrointestinal endoscopies | 111 (44.4) |
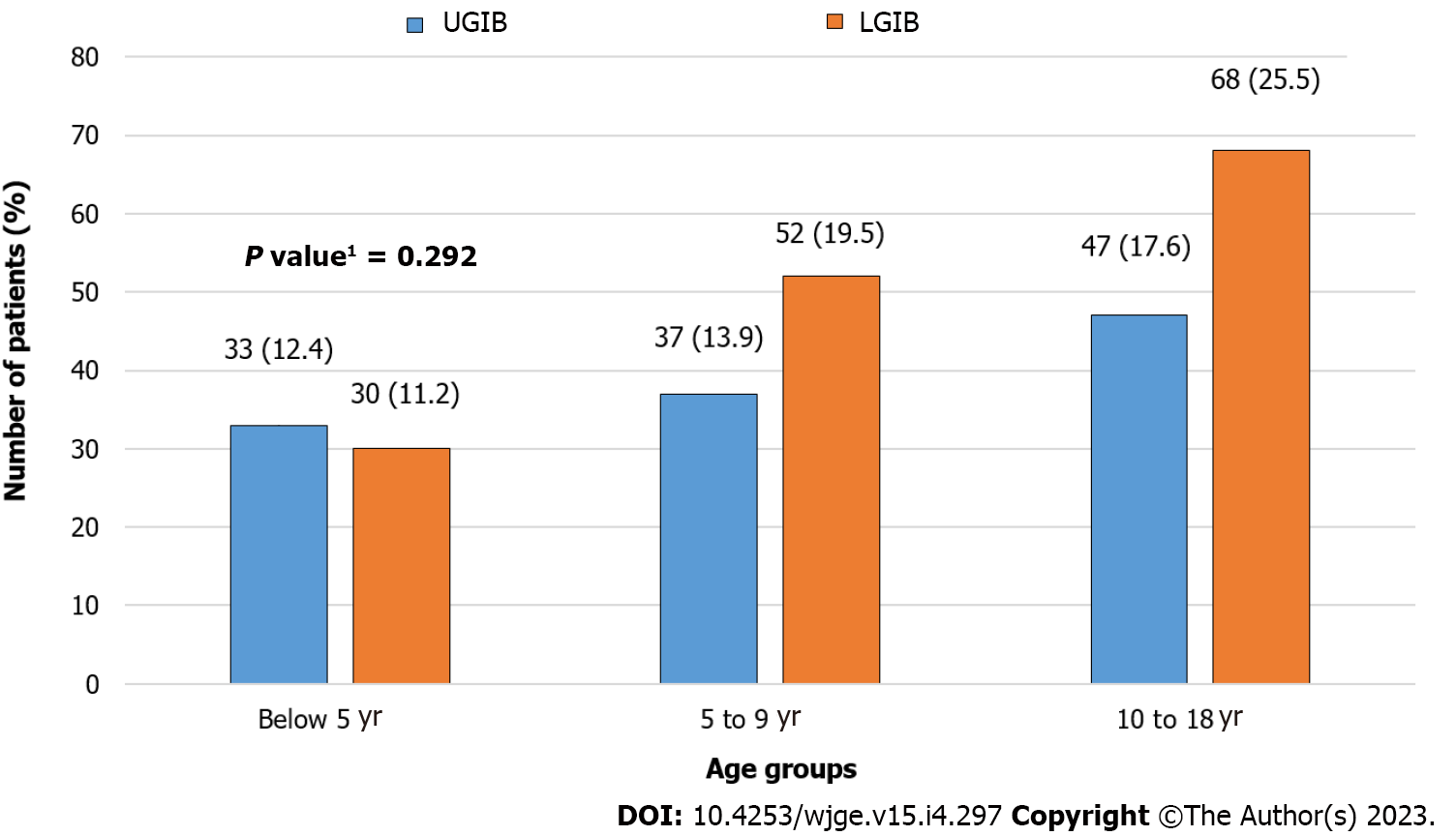
LGIB was more frequent (n = 151, 60.4%) than UGIB was (n = 119, 47.6%). Out of the 250 patients, 20 (8%) patients underwent both UGIB and LGIB. Children with LGIB were older [median age of 9 years (IQR, 5–12)] than those with UGIB [median age of 8 years (IQR, 4–11)]. This difference was not statistically significant (P = 0.185). There was also no significant difference in sex (P = 0.710) and nationality (P = 0.525) between the two groups (Figure 2).
The clinical presentations are shown in Table 2. The most common presenting symptom was per rectal bleeding (n = 151, 60.4%), followed by hematemesis (n = 117, 46.8%). Some patients presented with more than one symptom. Physical examination was unremarkable in most of the patients (n = 218, 87.2%). However, 32 (12.8%) patients had positive findings on physical examination (Table 2).
| Clinical presentation | Patients’ n (%) |
| Presenting symptoma | |
| Per rectal bleeding | 151 (60.4) |
| Hematemesis | 117 (46.8) |
| Melena | 25 (10) |
| Associated symptom | |
| Recurrent abdominal pain | 59 (23.6) |
| Diarrhea | 23 (9.2) |
| Constipation | 19 (7.6) |
| Recurrent vomiting | 17 (6.8) |
| Weight loss | 10 (4) |
| Chest pain | 8 (3.2) |
| History of foreign body ingestion | 7 (2.8) |
| Caustic ingestion | 1 (0.4) |
| Nausea | 1 (0.4) |
| Physical finding | |
| Normal | 218 (87.2) |
| Pallor | 11 (4.4) |
| Perianal fissure | 11 (4.4) |
| Perianal fistula | 4 (1.6) |
| Jaundice | 3 (1.2) |
| Failure to thrive | 2 (0.8) |
| Oral ulcers | 1 (0.4) |
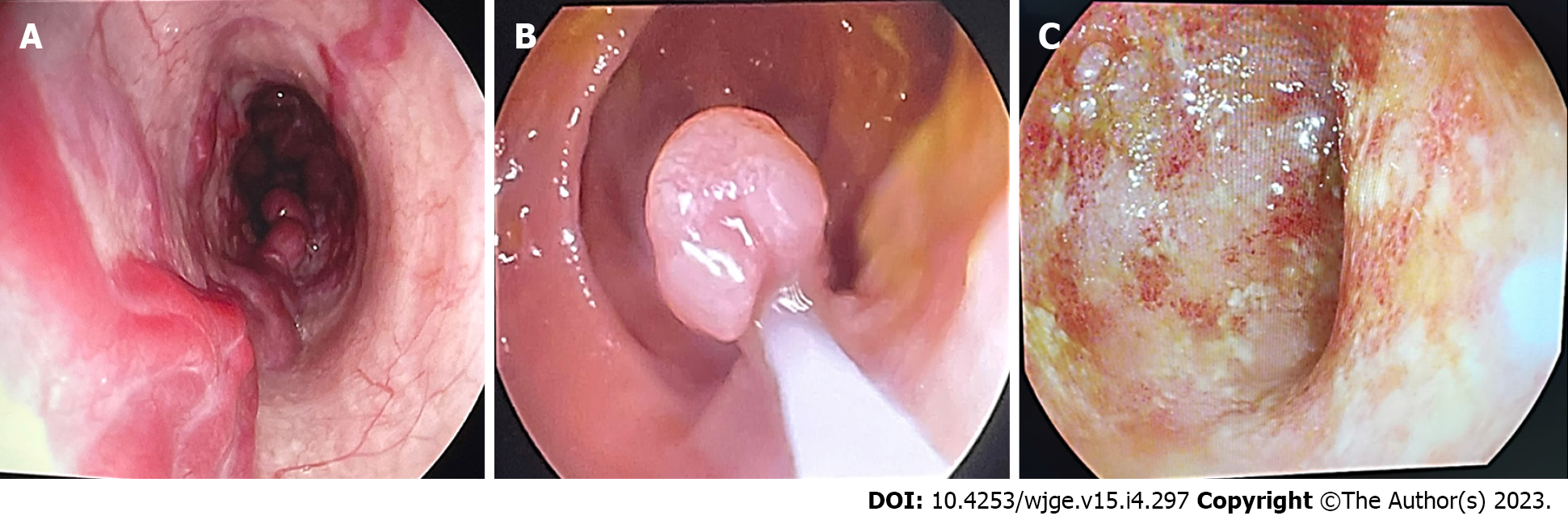
Most patients (n = 206, 82.4%) required one GIE; the remaining 44 (17.6%) required more than one GIE. The median number of endoscopies was one, ranging from one to seven. Abnormal endoscopic findings were detected in 226 (90.4%) patients; twenty-four (9.6%) patients had a normal GIE. Examples of patients with positive findings are shown in Figure 3.
The different causes of GIB according to age group are shown in Table 3. The most common cause of LGIB was IBD (n = 77, 30.8%); thirty-four (44.1%) had ulcerative colitis, 33 (42.9%) had Crohn’s disease, and 10 (13%) had unspecified IBD. The most common cause of UGIB was gastritis (n = 70, 28%); nonspecific gastritis (n = 55, 78.6%), Helicobacter pylori infection (n = 14, 20%), and eosinophilic gastritis (n = 1, 1.4%). In patients with both UGIB and LGIB, the causes of bleeding were gastritis (n = 6, 3.5%), gastroenteritis (n = 4, 2%), ulcerative colitis (n = 3, 1.5%), Crohn’s disease (n = 2, 1%), unspecified IBD type (n = 1, 0.5%), esophageal ulcer (n = 1, 0.5%), gastric ulcer (n = 1, 0.5%), duodenal ulcer (n = 1, 0.5%), and esophagitis with gastritis (n = 1, 0.5%).
| Causesa | Age group (yr) | Total, n (%) | P valueb | ||
| 0-4, n = 58 (23.2) | 5-9, n = 82 (32.8) | 10-18, n = 107 (42.8) | |||
| Inflammatory bowel disease | 10 (17.2) | 27 (32.9) | 40 (37.4) | 77 (30.8) | 0.026 |
| Gastritis | 16 (27.6) | 23 (28) | 31 (29) | 70 (28) | 0.980 |
| Unclear cause (normal) | 3 (5.2) | 4 (4.9) | 17 (15.9) | 24 (9.6) | 0.017 |
| Gastroenteritis | 7 (12.1) | 9 (11) | 6 (5.6) | 22 (8.8) | 0.275 |
| Duodenal ulcer | 5 (8.6) | 4 (4.9) | 11 (10.3) | 20 (8) | 0.397 |
| Esophagitis | 4 (6.9) | 5 (6.1) | 6 (5.6) | 15 (6) | 0.947 |
| Rectal polyp | 6 (10.3) | 5 (6.1) | 4 (3.7) | 15 (6) | 0.237 |
| Anal fissure | 1 (1.7) | 5 (6.1) | 5 (4.7) | 11 (4.4) | 0.461 |
| Peptic ulcer | 4 (6.9) | 4 (4.9) | 1 (0.9) | 9 (3.6) | 0.114 |
| Colonic ulcers | 2 (3.4) | 5 (6.1) | 2 (1.9) | 9 (3.6) | 0.305 |
| Rectal ulcer | 0 (0) | 2 (2.4) | 7 (6.5) | 9 (3.6) | 0.078 |
| Intestinal nodular lymphoid hyperplasia | 4 (6.9) | 4 (4.9) | 0 (0) | 8 (3.2) | 0.034 |
| Foreign body ingestion | 6 (10.3) | 1 (1.2) | 0 (0) | 7 (2.8) | < 0.0001 |
| Esophageal varices | 4 (6.9) | 0 (0) | 2 (1.9) | 6 (2.4) | 0.029 |
| Esophageal ulcer | 2 (3.4) | 1 (1.2) | 2 (1.9) | 5 (2) | 0.646 |
| Meckel’s diverticulum | 1 (1.7) | 2 (2.4) | 1 (0.9) | 4 (1.6) | 0.717 |
| Mallory Weiss syndrome | 1 (1.7) | 2 (2.4) | 0 (0) | 3 (1.2) | 0.291 |
| Hemorrhoids | 1 (1.7) | 0 (0) | 1 (0.9) | 2 (0.8) | 0.524 |
| Duodenal varices | 1 (1.7) | 0 (0) | 0 (0) | 1 (0.4) | 0.195 |
| Colonic angiodysplasia | 0 (0) | 0 (0) | 1 (0.9) | 1 (0.4) | 0.518 |
| CMPA | 1 (1.7) | 0 (0) | 0 (0) | 1 (0.4) | 0.195 |
IBD and unclear cause for bleeding were significantly higher in the 10–18 years group (P = 0.026 and P = 0.017, respectively), while intestinal nodular lymphoid hyperplasia, ingestion of foreign bodies, and esophageal varices were more frequent in the 0–4 years age group (P = 0.034, P < 0.0001, and P = 0.029, respectively). There were no significant differences between other causes according to age groups.
Ten (4%) patients underwent one or more therapeutic interventions [polypectomy (n = 4, 1.6%), injection sclerotherapy (n = 3, 1.2%) where one required two sessions, clipping (n = 2, 0.8%), and banding of esophageal varices and dilatation of esophageal stricture (n = 1, 0.4% each)]. Forty-five (18%) patients underwent follow-up endoscopy for disease reassessment. The median follow up period was two years (IQR, 0.5–3). No mortality was reported in this study.
This study revealed that the median incidence of GIB in children was 2.6/100000 per year, which has significantly increased over the last two decades. This increase could be attributed to the overall increase in some of the underlying etiologies, such as IBD. The burden of IBD is rising worldwide[8]. In the Middle East, the incidence of GIB in children is not well established[9,10]. However, in the United States, it accounts for 1% of all pediatric hospitalizations[11]. Romano et al[3] reported a higher incidence reaching 6.4% in Italy.
In the current study, most patients who presented with GIB were males (n = 144, 57.6%). This is comparable to several other studies, with a male predominance ranging between 54% and 59.2%[2,6,9,12,13]. However, Kalyoncu et al[14], Banisalamah et al[15], and Almadi et al[16] reported a higher percentage, ranging from 66.8% to 74.2%. The cause of this male predominance in children with GIB remains unclear.
In this study, the median age at the time of endoscopic diagnosis was 9 years (IQR, 5–11), with no significant difference according to the type of bleeding. Similarly, Cleveland et al[4] reported a median age of 10.1 years with a mean age of 9.3 ± 5.7 years. However, Gimiga et al[6], Rafeey et al[10], and Kalyoncu et al[14] reported GIB in younger children (1.3, 6.1 ± 3.9, and 7.6 ± 2.4 years, respectively). Nonetheless, the most commonly affected age group in our study was 10–18 years. However, Jafari et al[2] and Hassoon et al[9] reported that children aged 6–12 years were more frequently affected, with percentages of 31.8% and 24%, respectively. Gimiga et al[6] and Zahmatkeshan et al[12] reported that the 2–10 and 3–10 years age groups were the most commonly affected, representing 63.7% and 55.1% of their patient samples, respectively. This variation in age at diagnosis could be attributed to the differences in the study settings, inclusion criteria, and site and causes of bleeding in each study.
In the current study, the most common associated diseases were GERD and celiac disease (n = 7, 2.8%). Attard et al[13] reported a higher percentage of GERD in children with GIB (12.2%). Almadi et al[16] also reported a high percentage of GERD (38.13%) in adult patients with GIB. Celiac disease can cause occult GIB; it rarely presents as frank GIB[1].
In the present study, LGIB was more frequent than UGIB was, accounting for 60.4% (n = 151) and 47.6% (n = 119) of cases, respectively. However, Jafari et al[2] determined that UGIB was more common than LGIB. Apart from the Jafari et al[2] study, all the other published studies tackled either UGIB or LGIB alone. Thus, our findings cannot be compared with those of other studies.
In this study, per rectal bleeding was the most frequent presenting symptom (n = 151, 60.4%). Gimiga et al[6] and Zahmatkeshan et al[12] reported similar findings, with hematochezia as the most common symptom in 54.2% and 80.2% of their patients, respectively.
In our study, 117 (46.8%) patients presented with hematemesis. This percentage is higher than those reported by Jafari et al[2] (40.7%) and Rafeey et al[10] (26.9%). However, Cleveland et al[4] and Hassoon et al[9]. reported higher percentages of 58.5% and 73.4%, respectively. This might be related to the fact that hematemesis is bright red and usually alarms the child and family to seek early medical advice[9].
In the present study, melena was the third most common symptom. However, Jafari et al[2] (17.73%), Cleveland et al[4] (20.8%), and Rafeey et al[10] (13.42%) reported higher percentages of melena. In contrast, Hassoon et al[9] reported a lower percentage of 5.2%. This variation might be explained by the fact that melena is usually unnoticeable by the patients and their families, especially in older children; it typically appears after hematemesis, which leads to delayed presentation and diagnosis[9].
Recurrent abdominal pain was the most frequent associated symptom with GIB (n = 59, 23.6%). This result is comparable to that reported by Gimiga et al[6] (26.3%) and Zahmatkeshan et al[12] (24.5%), where abdominal pain was the most common accompanying symptom. However, Rafeey et al[10] reported a lower percentage (7.4%) of abdominal pain in children over the age of one. Several mechanisms can explain the association between abdominal pain and GIB, depending on the underlying etiology. Peptic or duodenal ulcers can develop due to the loss of the protective mucosal layer, which normally protects against gastric acid[17]. Deep or perforated ulcers irritate the gastric nerves or cause peritonitis, which causes severe abdominal pain[18].
In the current study, physical examination was unremarkable in most of the patients (n = 218, 87.2%). However, pallor was documented in 11 (4.4%) patients. Pallor might be related to the severity of bleeding and amount of blood loss. Cleveland et al[4] found that esophageal varices and duodenal ulcers are the most common conditions leading to anemia. Persistent or recurrent iron-deficiency anemia is a sign of obscure GIB[3]. Zahmatkeshan et al[12] reported iron deficiency anemia in 1.4% of the patients. However, Gimiga et al[6] reported a much higher incidence of hypochromic microcytic anemia (61.9%).
The causes of GIB in children vary based on the diagnostic approach used (radiological or endoscopic). Specific causes of GIB can be diagnosed based on imaging findings even before endoscopic intervention, such as foreign body ingestion, esophageal varices, intussusception, Meckel’s diverticulum, and IBD[19,20]. The role of radiology in the management of children with GIB differs according to patient age and clinical presentation[19]. Radiological imaging is frequently requested after a negative endoscopic evaluation or for undetermined causes or bleeding sites[19]. Abdominal ultrasonography, barium studies, computed tomography, magnetic resonance imaging, nuclear scintigraphy, and selective angiography may play a role in identifying the underlying pathology and exact source of bleeding[19]. In our study, IBD was the main cause of GIB in adolescents, whereas foreign body ingestion and esophageal varices were the main causes if GIB in preschool children. Çolak recently reported a small bowel intussusception caused by Meckel’s diverticulitis in a 10-year-old girl in whom it was diagnosed using radiological images even before endoscopic evaluation[20].
With advancements in the field of medical interventions, endoscopy has become the modality of choice for diagnosing GIB in children[21]. All the patients in this study were diagnosed via endoscopic examination. The causes of GIB among the published studies were diverse, which might account for the variation in disease distribution among different countries (Table 4). The most common cause of GIB in this study was IBD. Gimiga et al[6] reported ulcerative colitis (22%) as the second-most common cause of GIB. However, Jafari et al[2] and Zahmatkeshan et al[12] reported IBD to be a rare cause of GIB, accounting for only 4% and 5.8% of the study population, respectively. In patients with IBD, deep ulcers secondary to colitis might be sufficient to disrupt the underlying blood vessels of the inflamed and friable mucosa, causing GIB[11].
| Ref. | Country | n | Age (yr) | Sex | Bleeding site | Two most common symptoms (%) | Two most common causes (%) |
| Isa et al, 2023 | Bahraina | 250 | ≤ 18 | M > F | Both | Per rectal bleeding (60.4); Hematemesis (46.8) | Inflammatory bowel disease (30.8); Gastritis (28) |
| Jafari et al[2], 2018 | Iran | 113 | < 18 | M > F | Both | Hematemesis (40.7); Coffee ground vomitus (38) | Prolapse gastropathy (18.6) for UGIB; Polyps (32.5) for LGIB |
| Rafeey et al[10], 2013 | Iran | 447 | < 18 | M > F | UGIB | Hematemesis (26.85); Melena (13.42) | Erosive esophagitis (40); Gastric erosion (17) |
| Zahmatkeshan et al[12], 2012 | Iran | 363 | < 18 | M > F | LGIB | Hematochezia (80.2); Bloody diarrhea (18.1) | Juvenile polyp (23.1); Lymphoid nodular hyperplasia (18.2) |
| Hassoon et al[9], 2012 | Iraq | 58 | 4 d-18 | M > F | UGIB | Hematemesis (58.5); Melena or hematochezia (5.2) | Esophageal varices (39); Gastric erosions (19.6) |
| Gimiga et al[6], 2015 | Romania | 118 | < 18 | M > F | LGIB | Hematochezia (54.2); Rectorrhagia (40.7) | Solitary colorectal polyps (33); Ulcerative colitis (22) |
| Cleveland et al[4], 2012 | USA | 158 | < 17 | M > F | UGIB | Hematemesis (73.4); Melena (20.8) | Prolapse gastropathy syndrome (12.7); gastric erosions/ulcers (10.8) |
The second-most cause of GIB in this study was gastritis, with Helicobacter pylori infection accounting for 20% of the cases. However, Jafari et al[2] (7.1%), Rafeey et al[10] (14.5%), and Hassoon et al[9] (19.6%) reported lower percentages of gastritis in their study population. This difference might be due to the high prevalence of Helicobacter pylori gastritis in our community (57%)[22]. Duodenal ulcers were noted in 20 (8%) of our patients, which is comparable to that reported by Hassoon et al[9] (7.4%), Rafeey et al[10] (7.6%), and Cleveland et al[4] (8.2%). Duodenal ulcers can be caused by mucosal irritation from infections, such as Helicobacter pylori infection, or certain medications, such as nonsteroidal anti-inflammatory drugs[23].
Esophagitis occurs due to irritation of the esophageal mucosal lining by gastric acids[11]. In this study, esophagitis was observed in 15 (6%) patients, which is similar to that seen in Khan et al[24] (4%) and Hassoon et al[9] (4.9%). However, other studies report a higher percentage, ranging between 9.5% and 40%[2,4,10].
Intestinal polyposis is another cause of GIB. In this study, polyps were detected in only 15 (6%) patients. However, Zahmatkeshan et al[12], Jafari et al[2] and Gimiga et al[6], reported polyps as the most common cause of LGIB, representing 23.1%, 32.5%, and 33% of their study population, respectively.
In the present study, 4% of our patients underwent one or more therapeutic interventions. Polypectomy was the commonest (1.6%), followed by injection sclerotherapy (1.2%). Comparably, Lee et al[25] reported that 2.3% of their patients underwent polypectomy; however, they reported a higher percentage of injection sclerotherapy (21%).
Like most retrospective studies, this study was limited by missing medical data such as vital signs and hemoglobin levels at GIB presentation. In addition, this was a single-center study that included only patients who were admitted to the hospital and underwent an endoscopic procedure. Subsequently, children with GIB who presented to the pediatric emergency department and were discharged home, such as those with Mallory–Weiss syndrome, and those who were admitted but did not undergo endoscopy, were excluded. Therefore, this study might not reflect the true incidence of GIB in children. Another limitation is that, in 2020, most endoscopic procedures were cancelled due to the coronavirus pandemic. This resulted in a marked reduction in the total number of patients with GIB who underwent endoscopy that year.
Despite these limitations, this study is important because it is the first study from Bahrain to focus on children presenting with GIB. Moreover, this study covers most aspects of GIB, including the incidence, clinical presentation, diagnosis, therapeutic interventions, and outcomes in children. Furthermore, this study covered both types of GIB (upper and lower), which is considered a strength of this study; most previous studies reported only one type of bleeding. The findings of this study are essential for pediatricians or gastroenterologists to tailor their management strategies based on the most frequent causes of GIB according to the patient’s age group. Additionally, it forms a strong foundation for future research.
Gastrointestinal bleeding in children is an alarming condition that has increased significantly over the last two decades. LGIB was more common in our study population than UGIB was. Additionally, most of the patients presented with bleeding per rectum. Endoscopic procedures are the best modality for diagnosing this condition. IBD was the most frequent cause of LGIB, whereas gastritis was the most frequent cause of UGIB. The causes of GIB varied according to the patients’ age group and were different from those reported in neighboring countries and the rest of the world. The children in our study had particularly good outcomes. Further studies that include GIB identified in an emergency setting and those that assess the effect of GIB on patients’ hemodynamic stability, the need for blood transfusion, and the long-term impact of this condition are needed.
Gastrointestinal bleeding (GIB) is a serious health problem worldwide, particularly in childhood. The incidence, clinical presentation, and causes of pediatric GIB vary among countries.
Due to limited data on GIB in the pediatric population in the Middle East, we were motivated to study this health problem in Bahrain.
To assess the incidence, clinical presentation, causes, and outcomes of GIB in children at the main tertiary hospital in Bahrain over the last two decades and to stratify the causes of GIB according to the patients’ age group.
We retrospectively reviewed and collected the demographic data, clinical presentation, endoscopic findings, and outcomes of children with GIB admitted to the Pediatric Department at Salmaniya Medical Complex, Kingdom of Bahrain, from medical records between 1995 and 2022. The causes of GIB were compared according to patient’s age at presentation.
A total of 250 patients with GIB were included in this study. The median incidence was 2.6/100000 per year (interquartile range, 1.4–3.7) with a significantly increasing trend over the last two decades (P < 0.0001). Most patients were males (n = 144, 57.6%). The median age at diagnosis was 9 years (IQR, 5–11). Ninety-eight (39.2%) patients required upper gastrointestinal endoscopy alone, 41 (16.4%) required colonoscopy alone, and 111 (44.4%) required both. Lower GIB (LGIB) was more frequent (n = 151, 60.4%) than upper GIB (UGIB) (n = 119, 47.6%). There were no significant differences in sex (P = 0.710), age (P = 0.185), or nationality (P = 0.525) between the two groups. Abnormal endoscopic findings were detected in 226 (90.4%) patients. Inflammatory bowel disease (IBD) was the most common cause of LGIB (n = 77, 30.8%), whereas gastritis was the most common cause of UGIB (n = 70, 28%). IBD and undetermined cause for bleeding were higher in the 10–18 years group (P = 0.026 and P = 0.017, respectively), while intestinal nodular lymphoid hyperplasia, foreign body ingestion, and esophageal varices were more common in the 0–4 years group (P = 0.034, P < 0.0001, and P = 0.029, respectively). Ten (4%) patients underwent one or more therapeutic intervention. The median follow-up period by endoscopy was two years (IQR, 0.5-3). No mortality was reported in this study.
GIB in children is an alarming condition that is increasing significantly. LGIB were more frequent than UGIB. IBD was the most common cause of LGIB, whereas gastritis was the most common cause of UGIB in our children. The cause for GIB varied based on patient age and differed from those reported in neighboring countries and the rest of the world.
Further studies are needed that include children with GIB from an emergency setting and studies that assess the effect of this bleeding on patients’ hemodynamic stability, the need for blood transfusion, and the long-term impact of this condition.
We gratefully acknowledge all health care providers who provided the needed care for children with gastrointestinal bleeding in the Pediatric Departments at Salmaniya Medical Complex, Kingdom of Bahrain.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Bahrain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Çolak E, Turkey; Hu B, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Bresci G. Occult and obscure gastrointestinal bleeding: Causes and diagnostic approach in 2009. World J Gastrointest Endosc. 2009;1:3-6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 14] [Cited by in F6Publishing: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Jafari SA, Kiani MA, Kianifar HR, Mansooripour M, Heidari E, Khalesi M. Etiology of gastrointestinal bleeding in children referred to pediatric wards of Mashhad hospitals, Iran. Electron Physician. 2018;10:6341-6345. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Romano C, Oliva S, Martellossi S, Miele E, Arrigo S, Graziani MG, Cardile S, Gaiani F, de'Angelis GL, Torroni F. Pediatric gastrointestinal bleeding: Perspectives from the Italian Society of Pediatric Gastroenterology. World J Gastroenterol. 2017;23:1328-1337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 43] [Cited by in F6Publishing: 31] [Article Influence: 4.4] [Reference Citation Analysis (3)] |
| 4. | Cleveland K, Ahmad N, Bishop P, Nowicki M. Upper gastrointestinal bleeding in children: an 11-year retrospective endoscopic investigation. World J Pediatr. 2012;8:123-128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Saljoughian M. Gastrointestinal bleeding: An alarming sign. US Pharm 2009; 34: HS12-HS16. Available from: https://www.researchgate.net/publication/289783639_Gastrointestinal_bleeding_An_alarming_sign. [Cited in This Article: ] |
| 6. | Gimiga N, Burlea M, Diaconescu S, Olaru C. An assessment of the causes of lower gastrointestinal bleeding in a children’s hospital in northeastern Romania. Arch Biol Sci. 2015;67:715-720. [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 7. | WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: Methods and development. Geneva: World Health Organization, 2006. [Cited in This Article: ] |
| 8. | GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:17-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 604] [Cited by in F6Publishing: 1074] [Article Influence: 214.8] [Reference Citation Analysis (0)] |
| 9. | Hassoon AJ, AlMaeeni AA, Matloub HY. Upper gastrointestinal bleeding in children. J Fac Med Baghdad 2012; 54: 223-227. Available from: https://iqjmc.uobaghdad.edu.iq/index.php/19JFacMedBaghdad36/article/download/722/526. [Cited in This Article: ] |
| 10. | Rafeey M, Shoaran M, Majidy H. Diagnostic endoscopy and clinical characteristics of gastrointestinal bleeding in children: a 10-year retrospective study. Iran Red Crescent Med J. 2013;15:794-797. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Nationwide children’s. GI Bleeding. 2022. Available from: https://www.nationwidechildrens.org/conditions/gi-bleeding. [Cited in This Article: ] |
| 12. | Zahmatkeshan M, Fallahzadeh E, Najib K, Geramizadeh B, Haghighat M, Imanieh MH. Etiology of lower gastrointestinal bleeding in children:a single center experience from southern iran. Middle East J Dig Dis. 2012;4:216-223. [PubMed] [Cited in This Article: ] |
| 13. | Attard TM, Miller M, Pant C, Kumar A, Thomson M. Mortality associated with gastrointestinal bleeding in children: A retrospective cohort study. World J Gastroenterol. 2017;23:1608-1617. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 11] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Kalyoncu D, Urganci N, Cetinkaya F. Etiology of upper gastrointestinal bleeding in young children. Indian J Pediatr. 2009;76:899-901. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Banisalamah AA, Mraiat ZM. Upper gastrointestinal bleeding in Irbid, Jordan. Rawal Med J 2007; 32: 105-108. Available from: https://www.semanticscholar.org/paper/Upper-Gastrointestinal-Bleeding-in-Irbid%2C-Jordan-Banisalamah-Mraiat/738542c47059fe624e617ca753d5c378ddc8d8fa. [Cited in This Article: ] |
| 16. | Almadi MA, Almutairdi A, Alruzug IM, Aldarsouny TA, Semaan T, Aldaher MK, AlMustafa A, Azzam N, Batwa F, Albawardy B, Aljebreen A. Upper gastrointestinal bleeding: Causes and patient outcomes. Saudi J Gastroenterol. 2021;27:20-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 2] [Reference Citation Analysis (0)] |
| 17. | Malik TF, Gnanapandithan K, Singh K. Peptic ulcer disease. 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534792/. [Cited in This Article: ] |
| 18. | Di Saverio S, Bassi M, Smerieri N, Masetti M, Ferrara F, Fabbri C, Ansaloni L, Ghersi S, Serenari M, Coccolini F, Naidoo N, Sartelli M, Tugnoli G, Catena F, Cennamo V, Jovine E. Diagnosis and treatment of perforated or bleeding peptic ulcers: 2013 WSES position paper. World J Emerg Surg. 2014;9:45. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Racadio JM, Agha AK, Johnson ND, Warner BW. Imaging and radiological interventional techniques for gastrointestinal bleeding in children. Semin Pediatr Surg. 1999;8:181-192. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Çolak E. Meckel’ diverticulitis causing small bowel intussusception: A case report. Pediatr Pract Res. 2021;9:97-99. [DOI] [Cited in This Article: ] |
| 21. | ASGE Standards of Practice Committee; Fisher L, Lee Krinsky M, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Cash BD, Decker GA, Fanelli RD, Friis C, Fukami N, Harrison ME, Ikenberry SO, Jain R, Jue T, Khan K, Maple JT, Strohmeyer L, Sharaf R, Dominitz JA. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010;72:471-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 184] [Cited by in F6Publishing: 202] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 22. | Zainaldeen HA, Isa HM. Helicobacter pylori associated gastritis among Bahraini children presenting with abdominal pain. J Bahrain Med Soc 2010; 22: 52-54. Available from: https://www.researchgate.net/publication/286378046_Helicobacter_pylori_associated_gastritis_among_Bahraini_children_presenting_with_abdominal_pain. [Cited in This Article: ] |
| 23. | Barth B. 7 common causes of pediatric GI bleeding, plus treatment information. 2019. Available from: https://utswmed.org/medblog/gi-bleeding-children/. [Cited in This Article: ] |
| 24. | Khan MR, Ahmed S, Ali SR, Maheshwari PK, Jamal MS. Spectrum of upper GI endoscopy in pediatric population at a tertiary care centre in Pakistan. Open J Pediatr. 2014;4:180-184. [DOI] [Cited in This Article: ] |
| 25. | Lee WS, Zainuddin H, Boey CC, Chai PF. Appropriateness, endoscopic findings and contributive yield of pediatric gastrointestinal endoscopy. World J Gastroenterol. 2013;19:9077-9083. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.3] [Reference Citation Analysis (1)] |