Published online Apr 16, 2023. doi: 10.4253/wjge.v15.i4.285
Peer-review started: December 16, 2022
First decision: February 20, 2023
Revised: February 22, 2023
Accepted: March 15, 2023
Article in press: March 15, 2023
Published online: April 16, 2023
The optimal timing of esophagogastroduodenoscopy (EGD) and the impact of clinico-demographic factors on hospitalization outcomes in non-variceal upper gastrointestinal bleeding (NVUGIB) remains an area of active research.
To identify independent predictors of outcomes in patients with NVUGIB, with a particular focus on EGD timing, anticoagulation (AC) status, and demographic features.
A retrospective analysis of adult patients with NVUGIB from 2009 to 2014 was performed using validated ICD-9 codes from the National Inpatient Sample database. Patients were stratified by EGD timing relative to hospital admission (≤ 24 h, 24-48 h, 48-72 h, and > 72 h) and then by AC status (yes/no). The primary outcome was all-cause inpatient mortality. Secondary outcomes included healthcare usage.
Of the 1082516 patients admitted for NVUGIB, 553186 (51.1%) underwent EGD. The mean time to EGD was 52.8 h. Early (< 24 h from admission) EGD was associated with significantly decreased mortality, less frequent intensive care unit admission, shorter length of hospital stays, lower hospital costs, and an increased likelihood of discharge to home (all with P < 0.001). AC status was not associated with mortality among patients who underwent early EGD (aOR 0.88, P = 0.193). Male sex (OR 1.30) and Hispanic (OR 1.10) or Asian (aOR 1.38) race were also independent predictors of adverse hospitalization outcomes in NVUGIB.
Based on this large, nationwide study, early EGD in NVUGIB is associated with lower mortality and decreased healthcare usage, irrespective of AC status. These findings may help guide clinical management and would benefit from prospective validation.
Core Tip: Patients are often admitted for nonvariceal upper gastrointestinal bleeding (NVUGIB). There is not enough data on the importance and timing of esophagogastroduodenoscopy (EGD) in those scenarios. We investigated a nationally representative database to identify independent predictors of outcomes in patients with NVUGIB, with a particular focus on EGD timing, anticoagulation (AC) status, and demographic features. We found that early EGD in NVUGIB is associated with lower mortality and decreased healthcare usage, irrespective of AC status.
- Citation: Weissman S, Aziz M, Bangolo AI, Ehrlich D, Forlemu A, Willie A, Gangwani MK, Waqar D, Terefe H, Singh A, Gonzalez DMC, Sajja J, Emiroglu FL, Dinko N, Mohamed A, Fallorina MA, Kosoy D, Shenoy A, Nanavati A, Feuerstein JD, Tabibian JH. Relationships of hospitalization outcomes and timing to endoscopy in non-variceal upper gastrointestinal bleeding: A nationwide analysis. World J Gastrointest Endosc 2023; 15(4): 285-296
- URL: https://www.wjgnet.com/1948-5190/full/v15/i4/285.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i4.285
Non-variceal upper gastrointestinal bleeding (NVUGIB) is responsible for approximately 300000 hospital admissions in the United States (US) annually[1,2]. NVUGIB can range from mild to life-threatening, with a mortality rate of 3%-14% despite the best available care[3-5], and places a substantial burden on the healthcare system, with annual costs surpassing $1 billion[2]. The timing of endoscopy in acute NVUGIB has long been an area of discussion and research[4-12]. While multiple guidelines recommend early esophagogastroduodenoscopy (EGD) (within 24 h of admission) for NVUGIB, existing evidence regarding the benefit of early endoscopy remains unclear[1,4,6-10,13,14]. Several studies have revealed mortality benefits with early endoscopy; however, they included variceal hemorrhage in their cohort, were limited by small sample size, single-center experiences, and/or did not examine healthcare usage amongst the study outcomes[5,7,11].
While numerous scoring systems—such as the Rockall score, Blatchford score, and AIMS65—have been proposed to help risk stratify patients presenting with UGIBs, none of them have been adopted widely. Moreover, few large-scale studies have assessed variables such as anticoagulation (AC) use and/or demographic features for adverse hospitalization outcomes in NVUGIB.
The purpose of this study was to analyze a large, nationwide database to identify risk factors that predict differences in outcomes in patients hospitalized for NVUGIB—with a particular focus on timing to EGD, anticoagulation status, and demographic features.
The National Inpatient Sample (NIS) is the largest publicly available all-payer inpatient database in the United States with more than seven million hospital stays each year, as a part of the Healthcare Cost and Utilization Project. As such, this database contains de-identified data on nationwide hospital admissions including demographic information, clinical data, comorbidities, discharge diagnoses, procedures, outcomes, and hospitalization costs. It lists patients based upon a primary discharge diagnosis, up to 29 sary diagnoses, and is associated with 15 different procedural codes.
In this retrospective cohort study, using the NIS data from 2009 to 2014, adult (> 18 years old) patients with a primary diagnosis of NVUGIB were identified via validated International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes[15].
Exclusion criteria: Patients admitted electively, below the age of 18, with a history of liver cirrhosis, and/or admitted for anything other than NVUGIB were excluded from this study.
Inclusion criteria: Adult patients (> 18 years old), no past medical history of liver cirrhosis with or without varices, primary admission diagnosis of upper gastrointestinal (GI) bleed were included in our study.
Patients who had an esophagogastroduodenoscopy (EGD) during the hospitalization were identified and linked with the time and/or day the procedure was performed. Subsequently, those that underwent an EGD were stratified into 2 groups: (1) Early, defined as EGD performed within 24 h of admission; and (2) late, defined as EGD performed after 24 h from admission[12,13]. A subgroup analysis was performed by further stratifying these patients based on timing of EGD: (1) EGD performed within 24 h after admission; (2) EGD performed 24-48 h after admission; (3) EGD performed 48-72 h after admission; and (4) EGD performed more than 72 h after admission. Additionally, to determine the association between EGD timing and mortality, another subgroup analysis was performed to identify the AC status (warfarin, dabigatran, rivaroxaban, or apixaban) for all patients who underwent an EGD (due to the limited granularity of the NRD dataset, anti-platelet therapy use was unable to be determined). Thereafter, a sensitivity analysis was performed, for the most common etiology of bleeding, to determine the independent association between EGD timing and mortality. The validated ICD-9-CM diagnostic and procedural codes used in this study are presented in Supplementary Table 1[15]. Institutional Review Board approval was not required for this study as it was performed using de-identified and nationally available data.
Patient demographics were age, sex, race, primary expected payer, hospital bed size (small, medium, and large), teaching status, and hospital location (urban vs rural). Burden of comorbidities was assessed using the chronic condition indicator originating from the Elixhauser comorbidity index and Hwang’s method[16,17]. These are medical conditions that last 12 mo or longer, resulting in ongoing need for the use of medical services or products, and place undue limitations on self-care, independent living, and social interactions.
Hospital bed size was reported as small for hospitals in the northern region that had 1-49 beds (rural), 1-124 beds (Urban, nonteaching) and 1-249 beds (Urban, teaching); in the Midwest region that had 1-29 (rural), 1-74 (Urban, nonteaching) and 1-249 (Urban, teaching); southern region 1-39 (rural), 1-99 (Urban, nonteaching) and 1-249 (Urban, teaching); and western region 1-24 (rural), 1-99 (Urban, nonteaching) and 1-199 (Urban, teaching). Hospital bed size was reported as medium hospitals in the northern region that had 50-99 beds (rural), 125-199 (Urban, nonteaching) and 250-424 (Urban, teaching); Midwest region 30-49 (rural), 75-174 (Urban, nonteaching) and 250-374 (Urban, teaching); southern region 40-74 (rural), 100-199 (Urban, nonteaching) and 250-499 (Urban, teaching); and western region 25-44 (rural), 100-174 (Urban, nonteaching) and 200-324 (Urban, teaching). Hospital bed size was reported large for hospitals in the northern region that had 100+ beds (rural), 200+ (Urban, nonteaching) and 425+ (Urban, teaching); Midwest region 50+ (rural), 175+ (Urban, nonteaching) and 375+ (Urban, teaching); southern region 75+ (rural), 200+ (Urban, nonteaching) and 450+ (Urban, teaching); and western region 45+ (rural), 175+ (Urban, nonteaching) and 325+ (Urban, teaching).
Thirty comorbidities were taken into account among which: Congestive heart failure, Cardiac arrythmias, Valvular disease, Pulmonary circulation disorders, peripheral vascular disorders, Hypertension, paralysis, neurodegenerative disorders, uncomplicated diabetes, complicated diabetes, hypothyroidism, renal failure, liver disease, peptic ulcer disease excluding bleeding, acquired immunodeficiency syndrome/human immunodeficiency virus, lymphoma, metastatic cancer, solid tumor without metastasis, rheumatoid arthritis/collagen vascular diseases, coagulopathy, obesity, weight loss, fluid and electrolyte disorders, blood loss anemia, deficiency anemia, alcohol abuse, drug abuse, Psychoses, and depression.
Our primary outcome was in-hospital all-cause mortality: (1) Based upon ethno-racial/socioeconomic disposition; (2) per EGD timing; and (3) based upon long-term anticoagulation status. Our secondary outcomes included: (1) Intensive care unit (ICU) admission; (2) mean length of stay (LOS); (3) mean hospitalization charges and costs; and (4) patient disposition; discharge to home vs short- or long-term rehabilitation facilities. All these outcomes were defined using validated ICD-9 diagnostic and procedural codes, as shown in Supplementary Table 1[15].
Statistical analyses were performed using IBM SPSS statistics for windows software, version 24.0 (IBM Corp., Armonk, NY, United States). This software facilitates analysis to produce nationally representative unbiased results, variance estimates and P values. A weight for patient-level observations was implemented. Proportions were compared using the Chi square test and continuous variables were compared using the student t-test (for outcomes with two levels) and ANOVA (for outcomes with more than two levels). Univariate analysis was initially performed to calculate unadjusted odds ratio and determine confounders significantly associated with the outcomes. The multivariate regression analysis was performed to adjust for gender, race category, age category, insurance payer, hospital details (region, size, location, ownership), comorbidities and EGD within 1 d of admission. A significant association was determined with a cutoff P value of 0.2. Regression models were then built by including all confounders that were found to be significant by univariate analysis, to calculate adjusted odds ratio. Logistic regression was used to model in-hospital mortality with and without regard to anticoagulant use, ICU admission status, and patient disposition upon discharge. Linear regression was used to model hospital LOS and total charges. All P values were two sided, with 0.01 as threshold for statistical significance.
1082516 adult patients with a diagnosis of NVUGIB were included in the study. The mean age was 66.1 years, the majority of patients were female (50.3%), white (69.6%), and had 4 or more comorbidities (81.1%). Medicare was the primary payer insurance of the patients (62.2%) and patients were predominantly admitted to non-teaching hospitals (80.1%). The complete patient and hospital characteristics are presented in Table 1.
| Variable | Number (%) or mean ± SD |
| Mean age | 66.10 yr ± 16.45 yr |
| Age group | |
| 18 to 49 yr | 199875 (18.5) |
| 50 years or more | 882641 (81.5) |
| Sex | |
| Female | 544506 (50.3) |
| Male | 538010 (49.7) |
| Race | |
| White | 692345 (69.6) |
| Black | 145949 (14.7) |
| Hispanic | 95736 (9.6) |
| Asian/pacific islander | 26569 (2.7) |
| Native American | 7082 (0.7) |
| Other | 26982 (2.7) |
| Payment method/insurance type | |
| Medicare | 653964 (62.2) |
| Medicaid | 118107 (11.2) |
| Private insurance | 213404 (20.3) |
| Self-pay | 59962 (5.7) |
| Other insurance | 5932 (0.6) |
| Hospital location | |
| Urban | 288087 (81.8) |
| Rural | 63972 (18.2) |
| Hospital teaching status | |
| Non-teaching hospital | 334 (80.1) |
| Teaching hospital | 83 (19.9) |
| Hospital bed size | |
| Small | 188 (45.1) |
| Medium | 105 (25.2) |
| Large | 124 (29.7) |
| Comorbidities | |
| None | 12361 (1.1) |
| One | 45456 (4.2) |
| Two | 61930 (5.7) |
| Three | 84763 (7.8) |
| Four or more | 878006 (81.1) |
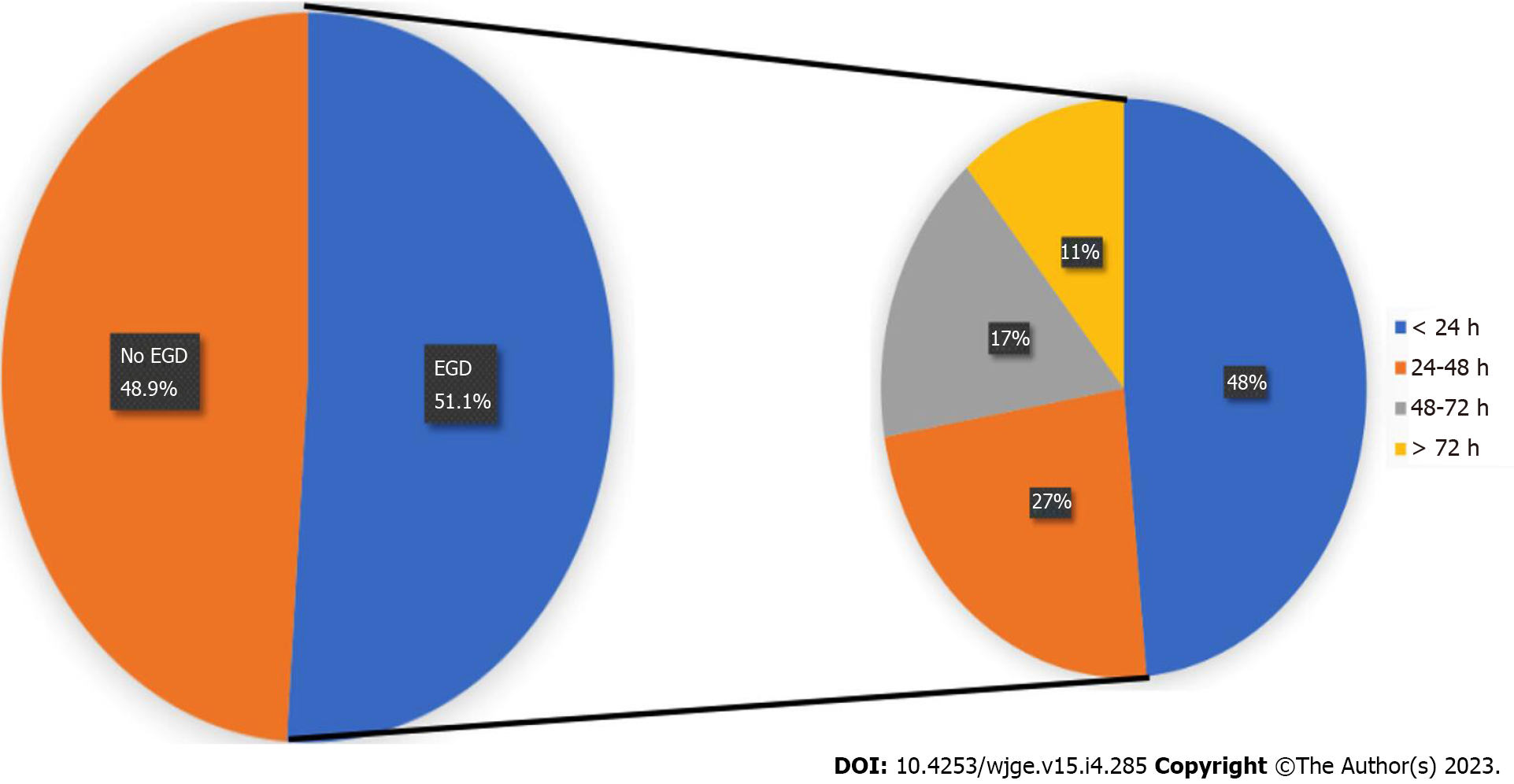
Of the 1082516 patients admitted for NVUGIB, 553,186 patients (51.1%) underwent EGD during hospital admission. Early (< 24 h) EGD was performed in 265529 patients (48%). The mean time to EGD was 52.8 h. Peptic ulcers represented the most common etiology of NVUGIB (62%). Figure 1 summarizes the pattern of EGD timing by gastroenterologists. Figure 2 summarizes the etiology of NVUGIB. Table 2 offers data on demographic/ethno-racial predictors of hospitalization outcomes.
| Factor | Mortality | LOS | Discharge home | ICU admission |
| Gender | ||||
| Male (vs female) | aOR: 1.32, 95%CI: 1.26-1.38a | aOR: -0.25, 95%CI: -0.30-0.1a | aOR: 1.22, 95%CI: 1.19-1.24a | aOR: 1.36, 95%CI: 1.32-1.40a |
| Ethnicity | ||||
| Black (vs White) | aOR: 0.95, 95%CI: 0.89-1.01 | aOR: 1.13, 95%CI: 1.05-1.21a | aOR: 0.96, 95%CI: 0.93-0.98a | aOR: 1.04, 95%CI: 0.99-1.09 |
| Hispanic (vs White) | aOR: 1.15, 95%CI: 1.07-1.24a | aOR: 0.62, 95%CI: 0.53-0.72a | aOR: 1.29, 95%CI: 1.24-1.35a | aOR: 1.10, 95%CI: 1.05-1.16a |
| Asian (vs White) | aOR: 1.30, 95%CI: 1.15-1.46a | aOR: 0.84, 95%CI: 0.67-1.01 | aOR: 1.21, 95%CI: 1.13-1.30a | aOR: 1.28, 95%CI: 1.18-1.40a |
| CCI | ||||
| 4 vs 0 | aOR: 4.71, 95%CI: 3.02 -7.35a | aOR: 2.82, 95%CI: 2.57–3.07a | aOR: 0.32, 95%CI: 0.26-0.38a | aOR: 5.35, 95%CI: 4.00-7.14a |
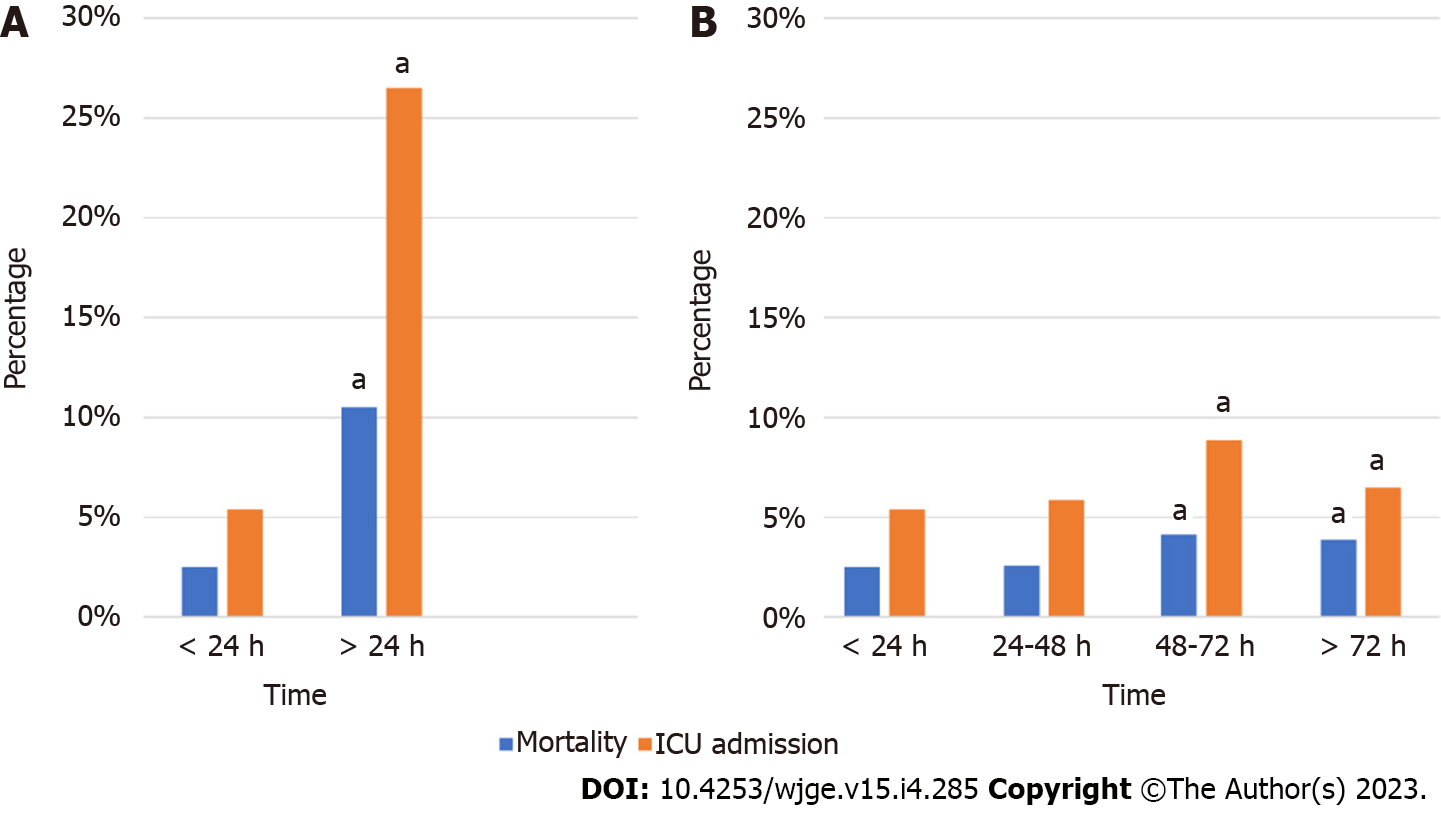
Our primary outcome, total all cause in-hospital mortality for patients admitted with NVUGIB, was 5.9%. There was a significantly increased likelihood of mortality in patients who underwent EGD after 24 h compared to those whom had it done within 24 h of admission (aOR 2.94, P < 0.001). Additionally, compared to those who underwent EGD within the first 24 h, there was a significantly increased likelihood of mortality if EGD was done 48-72 h (aOR 1.54, P < 0.001) or > 72 h of admission (aOR 1.63, P < 0.001); however, there was no mortality difference if EGD was performed 24-48 h of admission (aOR 1.01, P = 0.805) (Figure 3). Upon subgroup analysis, examining the most common etiology of bleeds, for both peptic ulcer bleeds and bleeding gastritis/duodenitis there was a significantly increased likelihood of in-hospital mortality in patients who underwent EGD after 24 h compared to those who had it done within 24 h of admission [(aOR 1.20, P < 0.001), and (aOR 1.15, P = 0.001) respectively].
Total all-cause in-hospital mortality for patients on long-term AC (either warfarin, dabigatran, rivaroxaban, or apixaban) (of note, anti-platelet therapy use was unable to be determined) admitted with NVUGIB was 7.0% as compared to 5.1% [aOR 2.02, P = 0.001] in patients that were not on AC. Total all-cause in-hospital mortality for patients on long-term AC who underwent EGD was 1.5% as compared to 2.5% [aOR 1.83, P = 0.001] in patients on long-term AC who did not undergo EGD. There was no significant difference in mortality between patients on long-term anticoagulation who underwent EGD within 24 h compared to those whom had it done after 24 h from admission (aOR 0.88, P = 0.193). Additionally, there was no significant difference in mortality for those on long-term anticoagulation if EGD was done 24-48 h (aOR 0.78, P = 0.015), 48-72 h (aOR 1.01, P = 0.907), or > 72 h from admission (aOR 1.35, P = 0.036), compared to those who underwent EGD within the first 24 h.
Of patients admitted for NVUGIB, 7.9% were admitted to the ICU at some point during the hospital stay. Patients who underwent EGD after 24 h had a significantly increased likelihood of ICU admission compared to those who underwent EGD within 24 h from admission (aOR 1.51, P = 0.001). Additionally, compared to those who underwent EGD within the first 24 h of admission there was a significant increased likelihood of ICU admission if EGD was performed 48-72 h (aOR 1.59, P = 0.001) or > 72 h (aOR 1.21, P = 0.001) from admission; however, there was no significant difference in ICU admission if EGD was performed within 24-48 of admission (aOR 1.03, P = 0.045) (Figure 3).
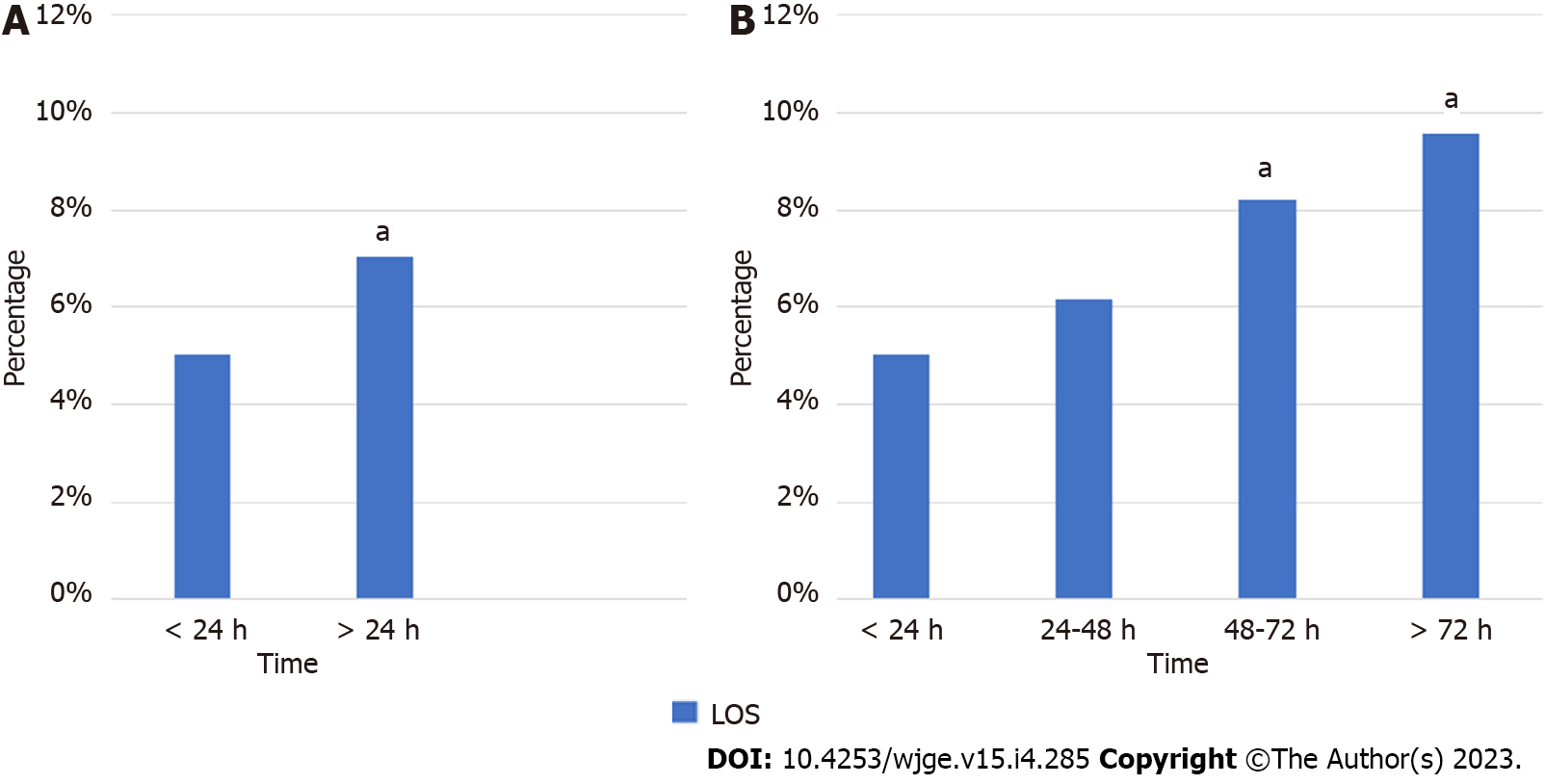
The mean LOS for patients admitted with NVUGIB was 6.55 d. Patients who underwent EGD within 24 h had a significantly lower LOS (adjusted coefficient: -2.19 d, P < 0.001) compared to those who underwent EGD after 24 h from admission. Additionally, compared to patients who underwent EGD within the first 24 h, there was a significantly increased LOS if EGD was performed 48-72 (adjusted coefficient: 2.90, P < 0.001) or > 72 h (adjusted coefficient: 4.43, P < 0.001) from admission; however no significant difference was found in LOS for EGD performed between 24-48 h (adjusted coefficient: 0.96, P = 0.08) (Figure 4).
Mean hospitalization charges for all patients admitted with NVUGIB was $56195. Patients who went through EGD in the first 24 h of admission had significantly lesser mean hospitalization charges compared to those who had it done post 24 h (adjusted coefficient: $-9021, P < 0.001). Additionally, compared to patients who underwent EGD within the first 24 h of admission, there were significantly higher hospitalization charges if EGD was performed 24-48 h (adjusted coefficient: $8441), 48-72 h (adjusted coefficient: $27341), or after 72 h (adjusted coefficient: $26216) from admission (all with P < 0.001) (Figure 5).
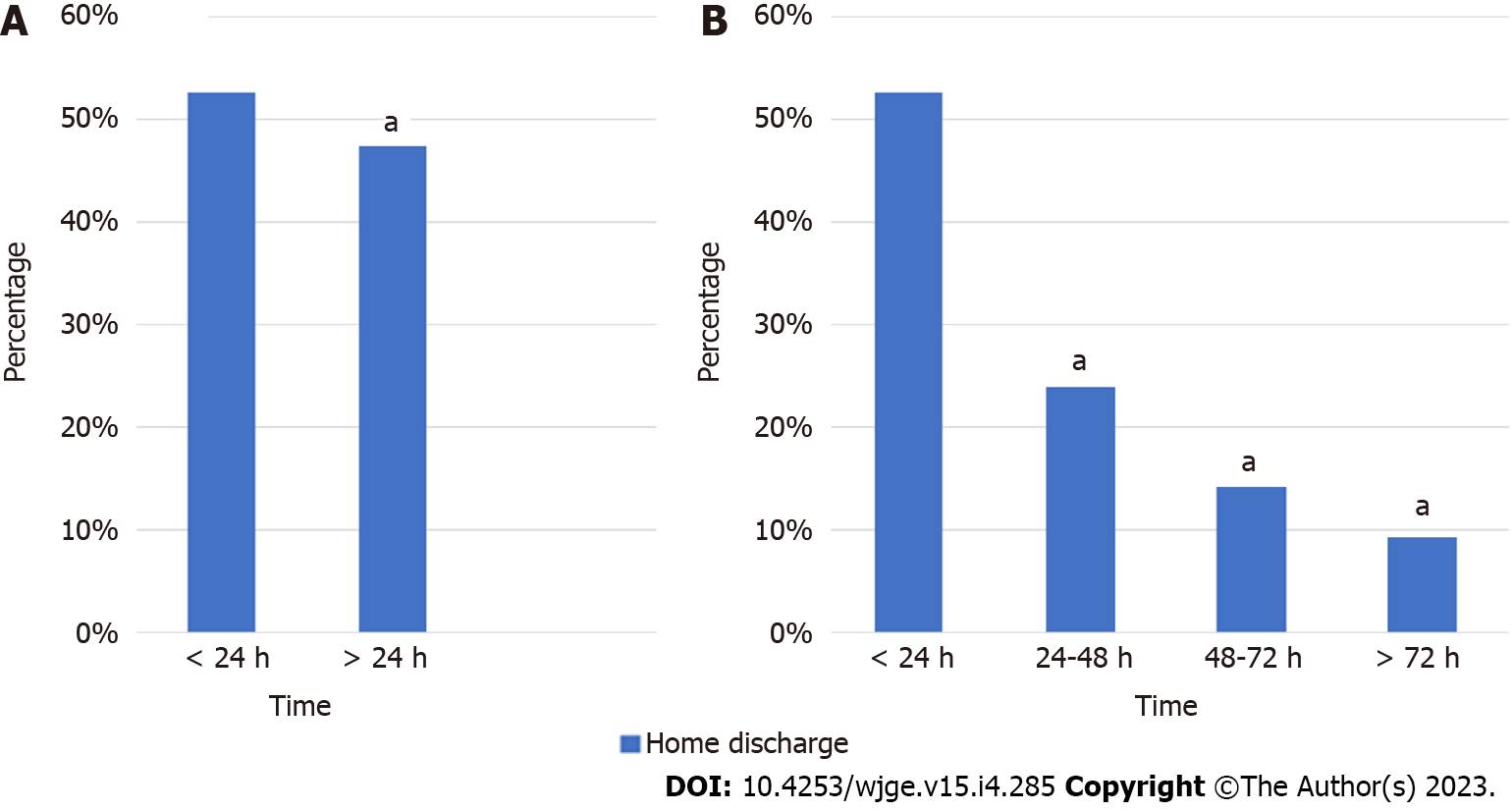
Overall, 56.9% of patients were discharged to home as opposed to a rehabilitation facility. Patients who had EGD after 24 h were significantly less likely to be discharged home than those who underwent EGD within 24 h from admission (aOR 0.69, P < 0.001). Additionally, there was a significantly decreased likelihood of discharge to home if EGD was performed 24-48 h (aOR 0.44), 48-72 h (aOR 0.60), or > 72 h (aOR 0.86) from admission, compared to patients who underwent EGD within the first 24 h of admission (all with P < 0.001) (Figure 6).
Using a large, nationally representative database, we found that mortality was significantly affected by the timing of endoscopic intervention in patients admitted with NVUGIB. Patients who underwent an EGD within the first 24 h had lower mortality than those who had it performed after 24 h of admission. Interestingly, there was no mortality difference if EGD was performed 24-48 h of admission as compared to within the first 24 h, despite current guidelines that suggest EGD within the first 24 h of hospital admission. In addition, we found that patients on long-term AC who did not undergo EGD had higher mortality than those who did, which appears to be unaffected timing. Moreover, we were able to identify numerous other factors such as-Male sex, Hispanic or Asian race, and those with more numerous comorbidities, to help predict patients at high risk for adverse hospital outcomes in NVUGIB.
Although prior studies have aimed to determine the appropriate timing of EGD in patients hospitalized for UGIB, the current study demonstrates some unique and important differences[4-14]. Including variceal hemorrhage amongst the etiology of bleeding, as done in prior studies, limits the value of extrapolating the data to NVUGIB in particular[11]. As variceal bleeding is thought to spontaneously cease (without endoscopic intervention) in up to 50% of cases and most other causes of upper GI bleeding in up to 80% of cases, variceal bleeding is of higher acuity[18,19]. While specifically examining NVUGIB (as opposed to all UGIB), as well as subgrouping by etiology of NVUGIB, we were able to identify the benefits/advantages of early endoscopy in this setting.
During the years of data collection (2009-2014), we noted that the mean time to EGD was 52.8 h, less than half of patients underwent EGD within 24 h of admission, and 11% of patients underwent EGD greater than 72 h after admission, even though current guidelines suggest EGD within the first 24 h of hospital admission.
Notably, the timing of EGD did not affect mortality in patients on long-term anticoagulation. Endoscopic hemostasis was notably safe and effective in a study where patients were anticoagulated with warfarin and international normalized ratio (INR) was observed to be 1.5-2.5. A limitation of this analysis was the low number of study sample (n = 23 patients)[20]. More studies are needed to assess the impact of elevated INR and/or use of direct oral anticoagulants and the risk of increased adverse outcomes (worsening bleeding, failure of hemostasis, need for transfusion, and/or mortality) in patients undergoing early endoscopy i.e., within 24 h of presentation. This will help formulate guidelines and assist the endoscopist in taking informed decisions for their patients that are on anticoagulants and presenting with NVUGIB.
Healthcare utilization was significantly affected by EGD timing. ICU admission rates were significantly higher in patients who had a delayed EGD (> 24 h from time of admission). Overall healthcare costs and LOS were also significantly affected by EGD timing. Additionally, discharge disposition was directly related to the timing of EGD, with those patients having an EGD within 24 h from admission being more likely to be discharged to home. Retrospective studies have shown the benefit of decreasing the length of stay in patients undergoing early EGD. Chak et al[21] demonstrated significantly decreased length of hospital stay in patients undergoing early EGD within 24 h of admission vs after 24 h (median 5 vs 7 d, P < 0.005). Similarly, Jairath et al[22] demonstrated that patients that underwent delayed endoscopy i.e. after 24 h remained 1.7 d longer in the hospital compared to those that underwent endoscopy within 12 h. Our study demonstrated a significant decrease in healthcare utilization, including ICU admission, data which has not been previously found on a national level[5]. Nevertheless, we acknowledge that perhaps patients whom went to the ICU were too hemodynamically unstable for an early EGD, thus it cannot be determined, based on this observation, what the causality was.
Our results are consistent with previous studies in terms of increasing age and comorbidities causing increased mortality rates in patients presenting with an upper GI bleed[23,24]. We further found that male sex, Hispanic or Asian race and persons on Medicaid insurance were also at increased risk of mortality. These findings may partially be explained by hormonal differences in (male) sex, and/or limited access to healthcare for patients of Hispanic/Asian race or those with Medicaid insurance.
Some limitations should be taken into account when interpreting the data of the current study. First, we used a database that relies on billing codes to generate diagnoses limited to the inpatient setting. Second, akin to many other national databases, a few important pieces of information might not be available in the NIS database. This missing data prevents the determination of the clinical severity or contraindications to EGD (e.g., severe coagulopathy). Third, the specific reason for EGD timing (24 h vs 48 h vs 72 h) remains unknown. While early EGD could be associated with hospital teaching status, patient comorbidity, age, and/or socioeconomic status, other factors not possible to quantify—such as endoscopist or patient preference-may have contributed. Lastly, incorrect ICD coding (and consequently erroneous inclusion of patients with variceal bleeding, for example) could have skewed data in favor of early EGD; however, with such a large dataset, we believe that such patients would be unlikely to significantly affect the overall results, especially since we have used validated codes[15].
Despite such limitations, our study has several strengths. The primary strength is the large sample size and breadth of the population studied. This is significantly more expansive than other studies on this topic, which tend to be smaller. Within the limits of making associations from a coding database, the large sample size and variety of patients lessen the risk of making unwarranted conclusions based on outliers. In addition, we were able to provide meaningful information on both well-studied endpoints such as all-cause inpatient mortality, as well as other less-studied outcomes such as ICU admission, health care utilization, and home discharge. Further, we were able to stratify based on several time strata to predict the appropriate time frame for EGD in NVUGIB.
To conclude, early EGD (within 24 h) is associated with several benefits including less mortality, irrespective of anticoagulation status. Insofar as high-quality RCTs examining the timing of EGD in NVUGIB are unlikely to be conducted, the findings of this large, nationwide study may serve as a useful clinical resource to effectively help guide patient care. Additionally, we identified numerous other factors such as-Male sex, Hispanic or Asian race, and those with more numerous comorbidities, all of which may help predict patients at high risk for adverse hospital outcomes in NVUGIB.
Patients are often admitted for nonvariceal upper Gastrointestinal bleeding (NVUGIB). However, there is not enough data on the importance and timing of esophagogastroduodenoscopy (EGD) in those scenarios.
The main motivation of this study was to identify independent predictors of outcomes in patients with NVUGIB, with a particular focus on EGD timing, anticoagulation (AC) status, and demographic features.
The purpose of this study was to analyze a large, nationwide database to identify risk factors that predict differences in outcomes in patients hospitalized for NVUGIB—with a particular focus on timing to EGD, anticoagulation status, and demographic features.
This was a retrospective analysis of patients with NVUGIB from 2009 to 2014, using validated ICD-9 codes from the National Inpatient Sample database. Patients were stratified by EGD timing relative to hospital admission (≤ 24 h, 24-48 h, 48-72 h, and > 72 h) and then by AC status (yes/no). The primary outcome was all-cause inpatient mortality. Secondary outcomes included healthcare usage.
553186 (51.1%) patients underwent EGD between 2009-2014. The mean time to EGD was 52.8 h. Early (< 24 h from admission) EGD was associated with significantly decreased mortality, less frequent ICU admission, shorter length of hospital stays, lower hospital costs, and an increased likelihood of discharge to home (all with P < 0.001). AC status was not associated with mortality among patients who underwent early EGD (aOR 0.88, P = 0.193). Male sex (OR 1.30) and Hispanic (OR 1.10) or Asian (aOR 1.38) race were also independent predictors of adverse hospitalization outcomes in NVUGIB.
Early EGD (within 24 h) is associated with lower mortality, less hospital cost and less healthcare utilization; regardless of the consumption of anticoagulants.
Randomized clinical trials examining the timing of EGD in NVUGIB will be difficult to conduct. Thus, the data of our study can shed some light on this clinically important subject. Additionally, we identified numerous other factors such as-Male sex, Hispanic or Asian race, Medicaid insurance, age > 50, and those with more numerous comorbidities, all of which may help predict patients at high risk for adverse hospital outcomes in NVUGIB.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elsayed MO, United Kingdom; Ko J, South Korea; Li J, China; Otani K, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Adler DG, Leighton JA, Davila RE, Hirota WK, Jacobson BC, Qureshi WA, Rajan E, Zuckerman MJ, Fanelli RD, Hambrick RD, Baron T, Faigel DO; ASGE. ASGE guideline: The role of endoscopy in acute non-variceal upper-GI hemorrhage. Gastrointest Endosc. 2004;60:497-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Esrailian E, Gralnek IM. Nonvariceal upper gastrointestinal bleeding: epidemiology and diagnosis. Gastroenterol Clin North Am. 2005;34:589-605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Colle I, Wilmer A, Le Moine O, Debruyne R, Delwaide J, Dhondt E, Macken E, Penaloza A, Piessevaux H, Stéphenne X, Van Biervliet S, Laterre PF. Upper gastrointestinal tract bleeding management: Belgian guidelines for adults and children. Acta Gastroenterol Belg. 2011;74:45-66. [PubMed] [Cited in This Article: ] |
| 4. | Hwang JH, Fisher DA, Ben-Menachem T, Chandrasekhara V, Chathadi K, Decker GA, Early DS, Evans JA, Fanelli RD, Foley K, Fukami N, Jain R, Jue TL, Khan KM, Lightdale J, Malpas PM, Maple JT, Pasha S, Saltzman J, Sharaf R, Shergill AK, Dominitz JA, Cash BD; Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. The role of endoscopy in the management of acute non-variceal upper GI bleeding. Gastrointest Endosc. 2012;75:1132-1138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 232] [Cited by in F6Publishing: 197] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 5. | Wysocki JD, Srivastav S, Winstead NS. A nationwide analysis of risk factors for mortality and time to endoscopy in upper gastrointestinal haemorrhage. Aliment Pharmacol Ther. 2012;36:30-36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Sung JJ, Chan FK, Chen M, Ching JY, Ho KY, Kachintorn U, Kim N, Lau JY, Menon J, Rani AA, Reddy N, Sollano J, Sugano K, Tsoi KK, Wu CY, Yeomans N, Vakil N, Goh KL; Asia-Pacific Working Group. Asia-Pacific Working Group consensus on non-variceal upper gastrointestinal bleeding. Gut. 2011;60:1170-1177. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 142] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 7. | Kumar NL, Cohen AJ, Nayor J, Claggett BL, Saltzman JR. Timing of upper endoscopy influences outcomes in patients with acute nonvariceal upper GI bleeding. Gastrointest Endosc. 2017;85:945-952.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Bjorkman DJ, Zaman A, Fennerty MB, Lieberman D, Disario JA, Guest-Warnick G. Urgent vs. elective endoscopy for acute non-variceal upper-GI bleeding: an effectiveness study. Gastrointest Endosc. 2004;60:1-8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 112] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Dworzynski K, Pollit V, Kelsey A, Higgins B, Palmer K; Guideline Development Group. Management of acute upper gastrointestinal bleeding: summary of NICE guidance. BMJ. 2012;344:e3412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. |
Iqbal U, Anwar H, Patel H, et al (February 28, 2018) Does Early Endoscopy Improve Mortality in Patients with Acute Non-variceal Gastrointestinal Bleeding? A Retrospective review.
|
| 11. | Garg SK, Anugwom C, Campbell J, Wadhwa V, Gupta N, Lopez R, Shergill S, Sanaka MR. Early esophagogastroduodenoscopy is associated with better Outcomes in upper gastrointestinal bleeding: a nationwide study. Endosc Int Open. 2017;5:E376-E386. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Lau JYW, Yu Y, Tang RSY, Chan HCH, Yip HC, Chan SM, Luk SWY, Wong SH, Lau LHS, Lui RN, Chan TT, Mak JWY, Chan FKL, Sung JJY. Timing of Endoscopy for Acute Upper Gastrointestinal Bleeding. N Engl J Med. 2020;382:1299-1308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 148] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 13. | Barkun AN, Almadi M, Kuipers EJ, Laine L, Sung J, Tse F, Leontiadis GI, Abraham NS, Calvet X, Chan FKL, Douketis J, Enns R, Gralnek IM, Jairath V, Jensen D, Lau J, Lip GYH, Loffroy R, Maluf-Filho F, Meltzer AC, Reddy N, Saltzman JR, Marshall JK, Bardou M. Management of Nonvariceal Upper Gastrointestinal Bleeding: Guideline Recommendations From the International Consensus Group. Ann Intern Med. 2019;171:805-822. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 209] [Cited by in F6Publishing: 259] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 14. | Mullady DK, Wang AY, Waschke KA. AGA Clinical Practice Update on Endoscopic Therapies for Non-Variceal Upper Gastrointestinal Bleeding: Expert Review. Gastroenterology. 2020;159:1120-1128. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 58] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 15. | Cooper GS, Chak A, Lloyd LE, Yurchick PJ, Harper DL, Rosenthal GE. The accuracy of diagnosis and procedural codes for patients with upper GI hemorrhage. Gastrointest Endosc. 2000;51:423-426. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 78] [Cited by in F6Publishing: 83] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6456] [Cited by in F6Publishing: 7226] [Article Influence: 277.9] [Reference Citation Analysis (0)] |
| 17. | Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood). 2001;20:267-278. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 292] [Cited by in F6Publishing: 303] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 18. | Prandi D, Rueff B, Roche-Sicot J, Sicot C, Maillard JN, Benhamou JP, Fauvert R. Life-threatening hemorrhage of the digestive tract in cirrhotic patients. An assessment of the postoperative mortality after emergency portacaval shunt. Am J Surg. 1976;131:204-209. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 35] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Hsu, Edmund, and Singwu D Law. “Refractory Nonvariceal Upper Gastrointestinal Bleeding Requiring Surgical Intervention. Cureus. 2019;11: e4135. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Choudari CP, Rajgopal C, Palmer KR. Acute gastrointestinal haemorrhage in anticoagulated patients: diagnoses and response to endoscopic treatment. Gut. 1994;35:464-466. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 106] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Chak A, Cooper GS, Lloyd LE, Kolz CS, Barnhart BA, Wong RC. Effectiveness of endoscopy in patients admitted to the intensive care unit with upper GI hemorrhage. Gastrointest Endosc. 2001;53:6-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Jairath V, Kahan BC, Logan RF, Hearnshaw SA, Doré CJ, Travis SP, Murphy MF, Palmer KR. Outcomes following acute nonvariceal upper gastrointestinal bleeding in relation to time to endoscopy: results from a nationwide study. Endoscopy. 2012;44:723-730. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Elsebaey MA, Elashry H, Elbedewy TA, Elhadidy AA, Esheba NE, Ezat S, Negm MS, Abo-Amer YE, Abgeegy ME, Elsergany HF, Mansour L, Abd-Elsalam S. Predictors of in-hospital mortality in a cohort of elderly Egyptian patients with acute upper gastrointestinal bleeding. Medicine (Baltimore). 2018;97:e0403. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Baradaran F, Norouzi A, Tavassoli S, Baradaran A, Roshandel G. Factors Associated with Outcome in Patients with Acute Upper Gastrointestinal Bleeding in a Tertiary Referral Center in Northern Iran. Middle East J Dig Dis. 2016;8:201-205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |