Copyright
©The Author(s) 2024.
World J Hepatol. Nov 27, 2024; 16(11): 1225-1242
Published online Nov 27, 2024. doi: 10.4254/wjh.v16.i11.1225
Published online Nov 27, 2024. doi: 10.4254/wjh.v16.i11.1225
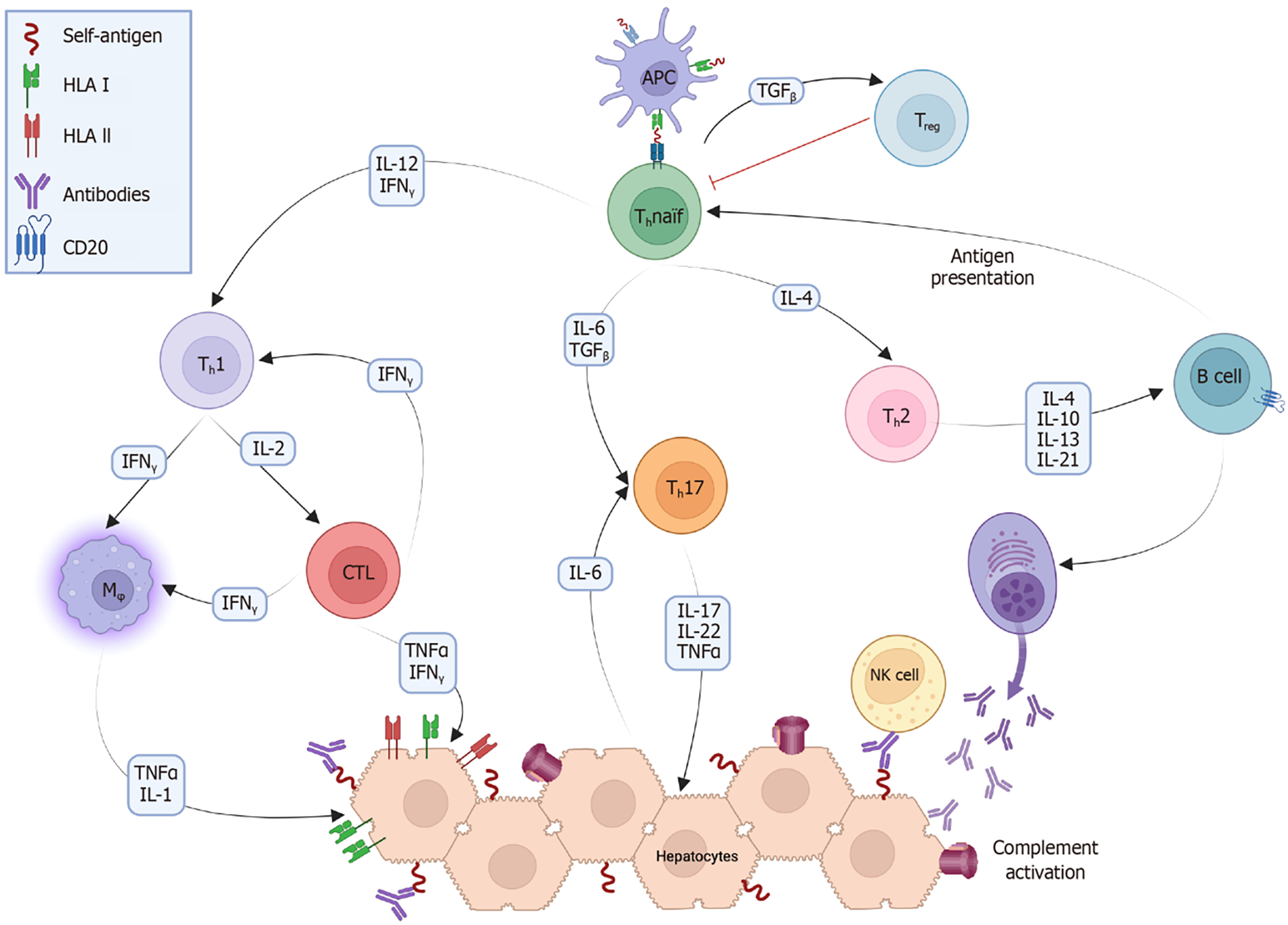
Figure 1 After a triggering event, peptides originating from healthy hepatocytes become self-antigens via a mechanism known as molecular mimicry.
These antigens are processed by antigen-presenting cells (APCs), consisting primarily of dendritic cells, and presented through human leukocyte antigen (HLA) type II to naïve T cells. APCs produce certain cytokines that, along with those already present in the environment, stimulate the differentiation of T helper (Th) cells into their different phenotypes (Th1, Th2, and Th17). This triggers a cascade of immune reactions, where Th1 cells produce interleukin (IL)-2 and interferon (IFN) gamma, which in turn stimulate cytotoxic T cells and macrophages (Mφ), as well as enhance the expression of HLA type I and II in hepatocytes. Th2 cells produce IL-4, IL-10, IL-13, and IL-21, which stimulate B cells to become plasmacytes and to produce antibodies. Active B cells also act as APCs to further stimulate naïve Th0 cells. Th17 cells secrete the proinflammatory cytokines IL-17, IL-22, and tumor necrosis factor (TNF). Natural killer (NK) cells recognize the components of antibodies fixed to the surface of hepatocytes and begin to lyse them. The complement system becomes active mainly through the classical pathway, forming membrane attack complexes on the surface of hepatocytes. Finally, through the stimulation of transforming growth factor (TGF) beta, Th0 cells become regulatory T cells, which secrete anti-inflammatory cytokines. CD: Cluster of differentiation; CTL: Cytotoxic T lymphocyte; Thnaïf: T helper naïf.
- Citation: Costaguta A, Costaguta G, Álvarez F. Autoimmune hepatitis: Towards a personalized treatment. World J Hepatol 2024; 16(11): 1225-1242
- URL: https://www.wjgnet.com/1948-5182/full/v16/i11/1225.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i11.1225