Copyright
©2009 Baishideng.
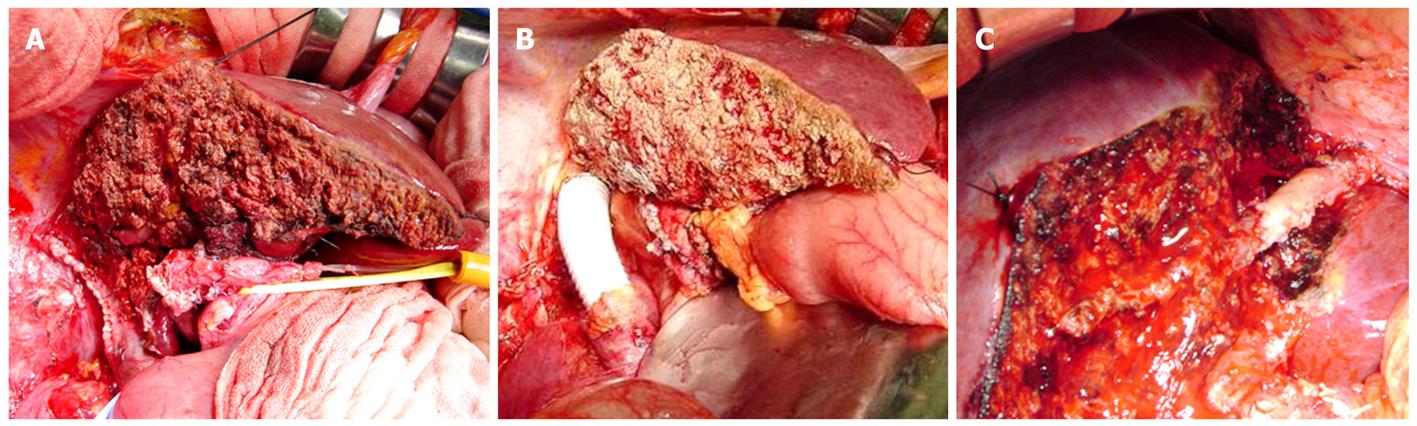
Figure 1 Combined resection of liver and major vessels.
A: Extended right hemihepatectomy with resection of the hepatic vena cava repaired primarily; B: Extended right hemihepatectomy with reconstruction of the hepatic vena cava with a Gore-Tex graft; C: Left hemihepatectomy with resection of the middle hepatic venous confluence with the IVC reconstructed using a portal vein graft from the resected liver specimen.
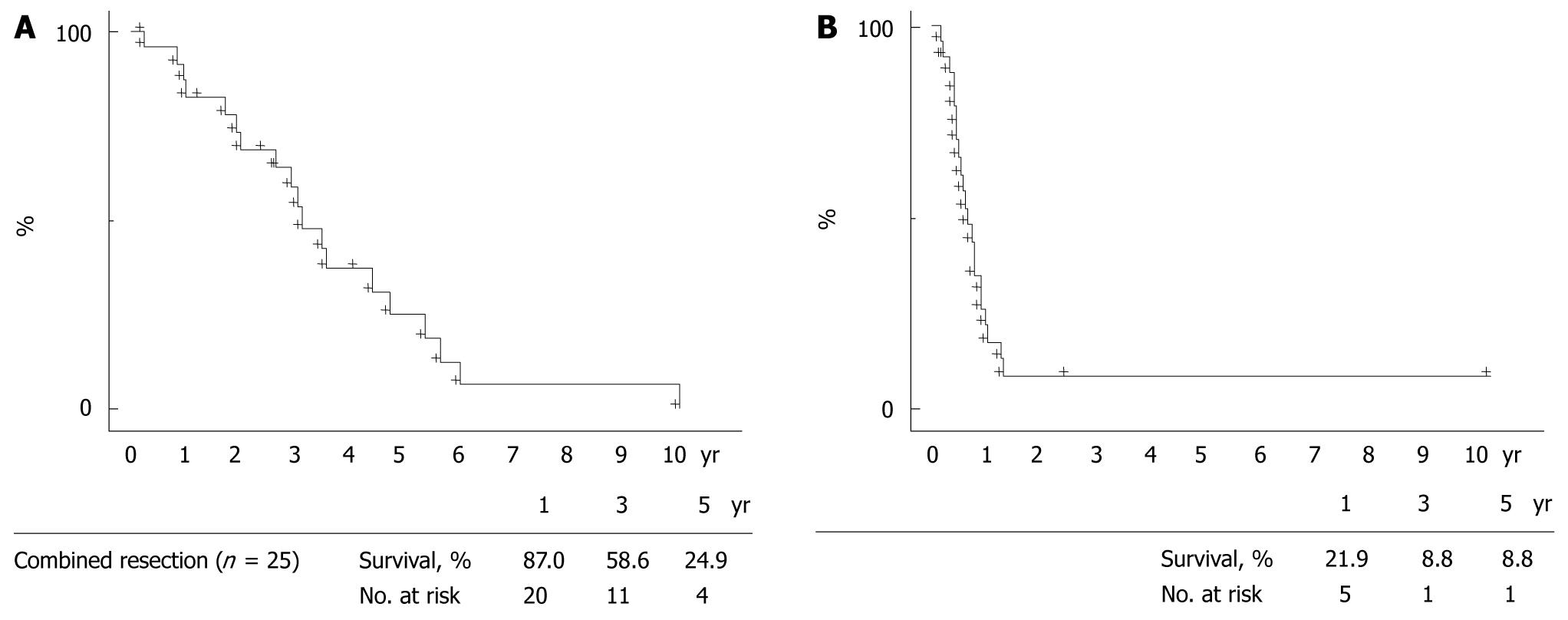
Figure 2 Overall survival (A) and disease-free rate (B) in years following surgery for 25 patients with resection/reconstruction of major vessels during hepatectomy for colorectal liver metastases.
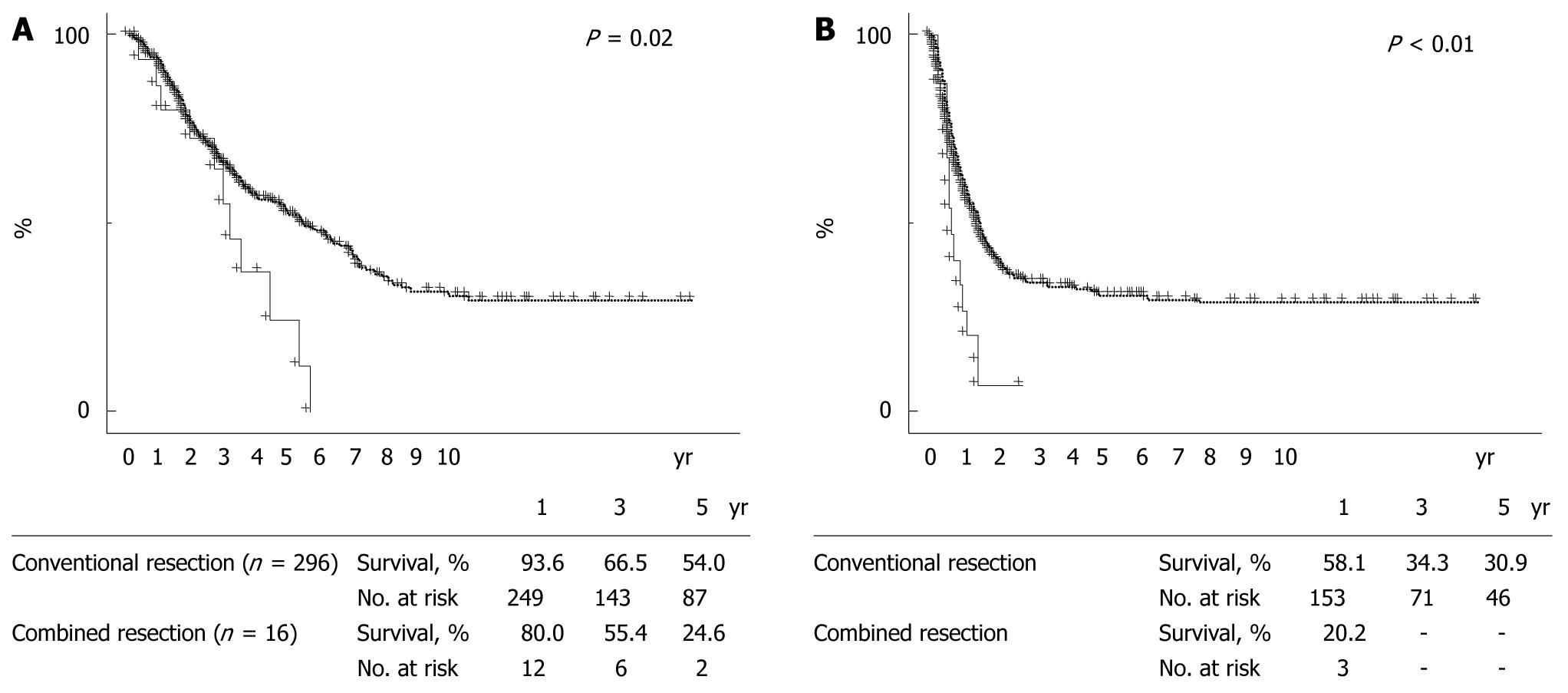
Figure 3 Overall survival (A) and disease-free rate (B) in years since a first liver resection.
When patients undergoing initial liver resections were divided into those with combined major vessel resection during hepatectomy (continuous lines, n = 16) vs with conventional hepatectomy (broken lines, n = 296), overall survival (panel A, P = 0.02) and disease-free rates (panel B, P < 0.01) were poorer in the combined resection group than in the conventional resection group.
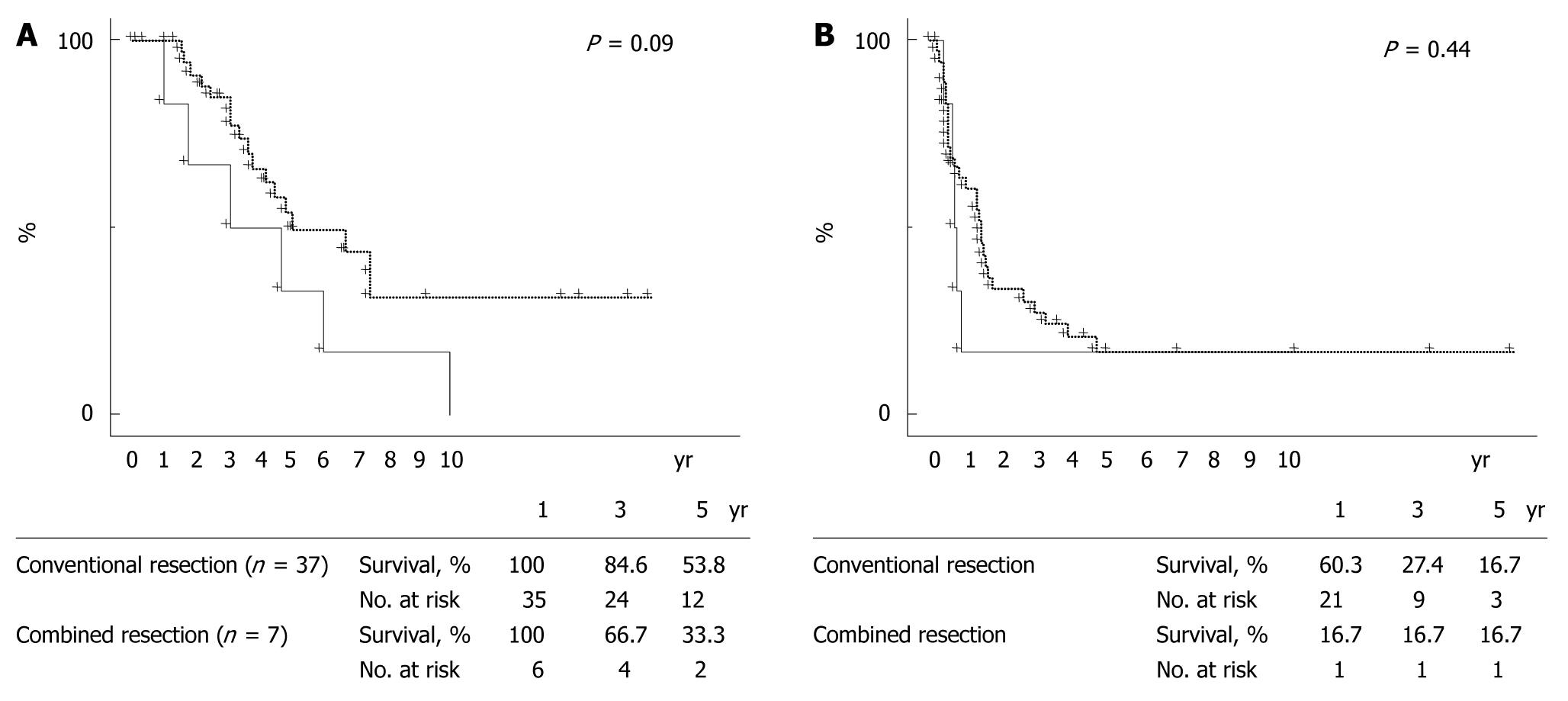
Figure 4 Overall survival (A) and disease-free rate (B) in years since repeat resection for liver recurrence.
When patients were divided into a combined resection group (continuous lines, n = 7) and a conventional group (broken lines, n = 37), overall survival (panel A, P = 0.09) tended to be poorer in the combined resection group than in the conventional resection group.
- Citation: Tanaka K, Matsuyama R, Takeda K, Matsuo K, Nagano Y, Endo I. Aggressive liver resection including major-vessel resection for colorectal liver metastases. World J Hepatol 2009; 1(1): 79-89
- URL: https://www.wjgnet.com/1948-5182/full/v1/i1/79.htm
- DOI: https://dx.doi.org/10.4254/wjh.v1.i1.79