INTRODUCTION
Mesenchymal stem cells (MSCs) are refined as undifferentiated cells that are capable of self renewal and differentiation into several cell types such as chondrocyte, adipocyte, osteocyte, myocyte and neuron-like cells[1,2]. MSC can be isolated from bone marrow, umbilical cord blood, adipose tissue, placenta etc. Although bone marrow (BM) has been regarded as a major source of MSC, umbilical cord blood has recently been regarded as an alternative source for isolation of MSC[3,4]. Human umbilical cord blood-derived mesenchymal stem cells (hUCB-MSCs) have a capacity similar to that of BM-MSCs for multi-lineage differentiation[5]. In addition, hUCB-MSCs also possess activities for immune modulation, tumor tropism and nursing effect[6,7]. When compared with other MSCs from various sources, hUCB-MSCs could be considered a fascinating source for use in stem cell therapy. In this review, we introduce the general characteristics of hUCB-MSCs and its application in various disease models.
GENERAL CHARACTERISTICS OF hUCB-MSCS
Immunogenic phenotypes of hUCB-MSCs
Immune rejection in recipient patients is the primary issue associated with use of MSCs as an allogeneic cell source for cell based therapy involving transplantation. In fact, previous studies of the properties of immune-privilege have been carried out primarily in BM-MSCs where the surface immunogenic markers were hypo-immunogenic which may prevent proliferation of allogeneic lymphocytes[8-10]. In the same fashion as BM-MSCs, major histocompatibility complex-II class molecules and costimulatory molecules, such as CD40, CD40 ligand, CD80 and CD86 which are involved in T cell activation response for transplant rejection, are not expressed in hUCB-MSCs even when mitogenic or allogeneic stimulated signals are delivered. In addition, differentiation of hUCB-MSCs into chondrocyte or neuron-like cells did not elicit expression of these immunogenic surface molecules and could not provoke allocative lymphocyte proliferation in mixed lymphocyte reactions (MLR) in vitro[11-13]. Compared with BM-MSCs, hUCB-MSCs showed lower immunogenicity than BM-MSCs because of primitive characters originating from UCB. Indeed, undifferentiated or differentiated hUCB-MSCs can be successfully transplanted for cell based therapy due to permission of a greater degree of HLA mismatch without graft versus host disease but not in BM-MSCs. Therefore, immunogenic phenotypes of hUCB-MSCs can retain low immunogenicity under certain biological conditions which provide advantages for development of off-the-shelf products for clinical application of cell transplantation. Thus, hUCB-MSCs show promise as a source for stem cell therapy.
Immune regulation properties of hUCB-MSC
MSCs are known to have immune suppressive action on lymphocyte proliferation in MLR by alloantigen and mitogens such as phytohemagglutinin and to reduce the level of proinflammatory cytokines such as interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α). Recent evidence has demonstrated that hUCB-MSCs can suppress not only the function of mature dendritic cells but also increase the portion of regulatory T cells related to immune regulation[12,13]. This regulation of immune response by MSCs is mediated by soluble factors and cell to cell contact mechanisms. At present, several soluble factors involved in immune suppression have been reported including transforming growth factor-β (TGF-β)[14]. However, induction of these cytokines was not observed under conditions of immune suppression by hUCB-MSCs and study of contact dependent inhibition by hUCB-MSCs is in progress. In fact, based on our unpublished data, hUCB-MSCs elevated the level of prostaglandin E2 and induced indoleamine 2, 3-dioxygenase (IDO). In addition, the surface molecule HLA-G which is involved in immune tolerance in pregnancy was detected in hUCB-MSCs by fluorescence activated cell sorter analysis. It has been suggested that the molecular mechanism(s) or strategy for immune regulation by MSCs is dependent on species and tissue origin[15,16].
Consequently, to understand and utilize the immune regulation properties of hUCB-MSCs for application in the treatment of a number of human immunological diseases, the molecular mechanism underlying the immune modulatory functions of hUCB-MSCs should be further investigated.
APPLICATION OF hUCB-MSCS IN DISEASE MODELS
hUCB-MSCs for cartilage regeneration
Since MSCs are capable of differentiation into mesodermal origin, several groups have tried cell therapy for osteoarthritis (OA), the most common type of arthritis. Two representative common diseases of cartilage degeneration include OA and rheumatoid arthritis (RA). OA is a progressive degenerative disease of the cartilage that is induced by complex factors that include increasing age, mechanical stress and inflammation leading to primary focal cartilage degradation and its functional loss. RA is a chronic autoimmune disease characterized by inflammation of the lining of the synovium or joints that causes long term joint damage, particularly in cartilage[17]. MSCs are known for differentiation into mesodermal derived tissue such as cartilage, bone, adipose and muscle. In fact, hUCB-MSCs have much higher chondrogenic differentiation potential among mesodermal differentiation potentials which might lead to regeneration of damaged cartilage. In addition to this chondrogenic differentiation potential of MSCs, recent advances in our understanding of the regeneration mechanism for cartilage defects have demonstrated that MSCs also show potent immunosuppression and anti-inflammatory effects[11-14]. These properties might be due in part to specific secreted factors, including some types of cytokines and growth factors. For instance, it has been reported that thrombospondin-1, 2 (TSP-1, 2) functions as an anti-inflammatory factor in RA by suppressing production of proinflammatory mediators such as IFN-γ and TNF-α, inducing depletion of synovium residing T cells and reducing infiltration of monocytes/macrophages in articular tissues[18,19]. In this fashion, chondrogenic differentiation and paracrine actions might be involved in replacement of damaged cartilage tissues and stimulation of the regeneration process.
However, several research teams have conducted studies to demonstrate the therapeutic potential of BM-MSCs for OA or RA[20-24] but few studies have reported on hUCB-MSCs. Despite growing experience and knowledge of these attempts, the molecular mechanisms underlying cartilage repair and regeneration by MSCs remain uninvestigated. Therefore, extensive studies of hUCB-MSCs therapeutic mechanisms are required for an understanding of their regenerative potential and for efficient and safe clinical application. Fortunately, supported by our clinical trial phase I/II results (NCT01041001), we believe that adult stem cell therapy using hUCB-MSCs for cartilage degenerative disease is a promising alternative to previous treatments if optimal hUCB-MSCs therapy conditions are adjusted by a full understanding of the important regeneration mechanism for diseases of cartilage degeneration.
hUCB-MSCs for glioma
Interestingly, MSCs have been shown to migrate toward glioma[25]. This phenomenon could be applied to tumor therapy with MSCs loaded tumor therapeutic agent. TRAIL, IL-12, IFN-β and cytosine deaminase have been used as therapeutic agents in MSCs-mediated delivery. In particular, TRAIL-secreting hUCB-MSCs showed therapeutic effects in an intracranial glioma model[26]. Injection of engineered MSCs inhibited tumor-growth and prolonged the lifespan of glioma-bearing mice compared with control. Although this glioma tropism has been demonstrated, the exact molecular mechanism has not been elucidated. As glioma over expressed interleukin-8 (IL-8), our group tested IL-8 action in hUCB-MSCs migration toward glioma. Interestingly, a high level of IL-8 was detected in the conditioned media of co-cultured glioma cells with hUCB-MSCs. Recombinant IL-8 treatment of hUCB-MSCs enhanced migration to the lower chamber under the Transwell system. This effect was reduced by pre-treatment of hUCB-MSCs with antibody against CXC chemokine receptor 1 (CXCR1) and CXCR2, IL-8 receptor. Therefore, IL-8 will be an attracting factor for hUCB-MSCs migration toward glioma[27]. We expect that IL-8 receptor over expression in hUCB-MSCs will efficiently deliver cancer drugs to glioma. For application of hUCB-MSCs in human glioma, more efficient and safe methods of therapeutic gene expression in hUCB-MSCs should be established.
hUCB-MSCs for ischemic brain damage
Because brain injury due to ischemia cannot be recovered and can result in severe functional defects in the brain, stroke is a primary disease target for stem cell therapy. In ischemia studies, most data show that cell therapy is performed using hUCB. The first evidence of a therapeutic effect of hUCB came from Chopp’s laboratory, where rat was used for middle cerebral artery occlusion to induce focal ischemia. Intravenous administration of hUCB reduces behavioral deficits after stroke in rats[28]. Recently, infarct volume was reduced 1 d after intra arterial delivery of hUCB-MSCs in canine cerebral ischemia whereas infarct volume was increased in the control groups. Transplanted hUCB-MSCs were differentiated into neurons and astrocytes in and around endothelial cells and secreted brain-derived neurotrophic factor and vascular endothelial growth factor at 4 wk after transplantation[29]. Jeong et al[30] reported that transplantation of hUCB-MSCs into contralateral regions of injured rat brain at 7 d after injury resulted in significant behavioral improvement. In addition, PKH26-labled hUCB-MSCs differentiated into neural cells at the injured site at 4 wk after transplantation. These results suggested that transplantation of hUCB-MSCs could be used in clinical trials for ischemia. Despite these interesting data, stem cell therapy using hUCB-MSCs have to make critical decisions with regard to the route of transplantation, type of injected cell (hUCB vs hUCB-MSCs) and timing of transplantation.
hUCB-MSCs for lung diseases
Progression of acute respiratory distress syndrome is demonstrated by loss of lung tissue as a result of inflammation and fibrosis. Human umbilical cord cells derived from Wharton’s jelly with a phenotype consistent with that of MSCs (uMSCs) were treated using a bleomycin induced-lung injury mouse model[31]. After 2 wk, systemic administration of uMSCs was located in the area of inflammation and fibrosis. Injected uMSCs reduced inflammation and inhibited expression of TGF-β, IFN-γ and proinflammatory cytokines, including macrophage migratory inhibitory factor and TNF-α. Furthermore, collagen level was decreased due to up-regulation of matrix metalloproteinase-2 and reduced endogenous inhibitors, tissue inhibitors of matrix metalloproteinases. These results suggested that uMSCs participate in anti-fibrosis in lung injury. Interestingly, hUCB-MSCs transplantation can attenuate hyperoxia-induced lung injury in immunocompetent newborn rats[32]. A single dose of PKH26 labeled hUCB-MSCs was administered intratracheally (2 × 106 cells) at postnatal day 5. Two abilities of hUCB-MSCs, immune modulation and differentiation potential, were evaluated after hUCB-MSCs administration. The hyperoxia-induced increase in the number of dead cells, myeloperoxidase activity, abnormal alveolarization and level of IL-6 mRNA were significantly decreased with intratracheal hUCB-MSCs administration. Furthermore, increased level of TNF-α, TGF-β mRNA, α-SMA protein and collagen were significantly reduced by hUCB-MSCs. As pKH26-labeled differentiated lung epithelial cells were observed in damaged lung, collectively, hUCB-MSCs could be used for cell therapy via both anti-inflammation and regeneration in hypoxia induced lung injury.
hUCB-MSCs for liver diseases
Cirrhosis is a consequence of chronic hepatic injury characterized by replacement of liver tissue by fibrosis and scar tissue. Cirrhosis is most commonly caused by alcoholism, fatty liver and hepatitis B and C. No effective therapy is currently available for this disease[33]. Recent reports have shown that MSCs have the capacity for differentiation into hepatocytes. In carbon tetrachloride (CCl4)-induced cirrhosis in a rat model, hUCB-MSCs infusion showed inhibition of TGF-β1, collagen type I and α-SMA expression. In addition, CM-DiI-labeled hUCB-MSCs expressed hepatocyte-specific markers, human albumin and α-fetoprotein in injured liver[34]. Similar data was observed by Yan et al[35]. Interestingly, terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate (dUTP)-biotin nick end labeling and proliferating cell nuclear antigen staining showed that transplanted hUCB-MSCs could prevent hepatocyte cell death and stimulate proliferation. According to these data, hUCB-MSCs could be useful in liver therapy. Liver contains endogenous abundant progenitor cells for recovery of liver damage. Therefore, it is currently difficult to determine which stem/progenitor cell populations are best for liver disease therapy.
CONCLUSION
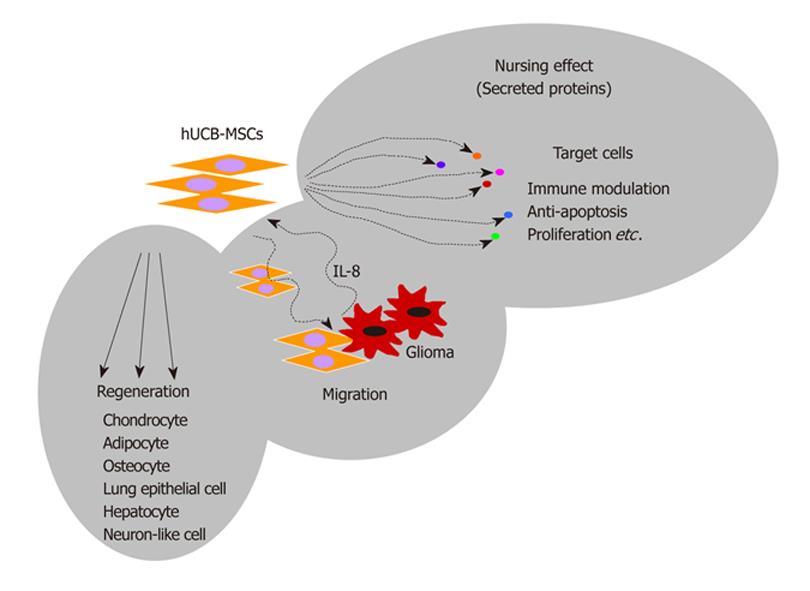
In the effort to overcome incurable disease, stem cell therapy has been regarded as the next solution. In particular, adult stem cells such as hUCB-MSCs have shown therapeutic efficacy in various animal disease models. Compared to embryonic stem cells, adult stem cells have several advantages for use in stem cell therapy. Adult stem cells are relatively free of ethical issues, immune rejection and tumor formation. In particular, hUCB-MSCs are obtained from discarded umbilical cord blood after child birth. If informed consent is available from pregnant mothers, hUCB-MSCs can be easily isolated from cord blood under aseptic conditions. Since public and private cord blood banking systems are well established in Korea, basic and clinical investigation into development of cell therapies has been intense. Furthermore, immunological safety has been proven in several journals although application of hUCB-MSCs is based on allogeneic transplantation. In addition, there have been no reports of tumor formation after transplantation of hUCB-MSCs in animals or humans. From this review, we could conclude that regeneration of target tissue by differentiation and nursing effect by secreted proteins are among the molecular mechanism of hUCB-MSCs action in various diseases (Figure 1). In the early days of stem cell research, regenerative medicine was the main stream of research. However, paracrine action of stem cells under pathological conditions is now emerging. The study of hUCB-MSCs is incomplete compared to that of BM-MSCs. However, once basic scientific understanding of hUCB-MSCs have shown further advancement and conditions for isolation and expansion of hUCB-MSCs are well established for the clinic, hUCB-MSCs will be a fascinating source for use in stem cell therapy.
Figure 1 Multifunctional therapeutic activities of human umbilical cord blood-derived mesenchymal stem cells (hUCB-MSCs).
Transplanted hUCB-MSCs participate in cartilage, lung and liver regeneration through differentiation of damaged tissues as well as attenuation of inflammation and apoptosis. Interestingly, hUCB-MSCs can migrate toward glioma. When migrated hUCB-MSCs express apoptotic gene such as TRAIL in glioma region, tumor size will be decreased by secreted TRAIL from hUCB-MSCs.