Copyright
©The Author(s) 2025.
World J Gastroenterol. Feb 21, 2025; 31(7): 100973
Published online Feb 21, 2025. doi: 10.3748/wjg.v31.i7.100973
Published online Feb 21, 2025. doi: 10.3748/wjg.v31.i7.100973
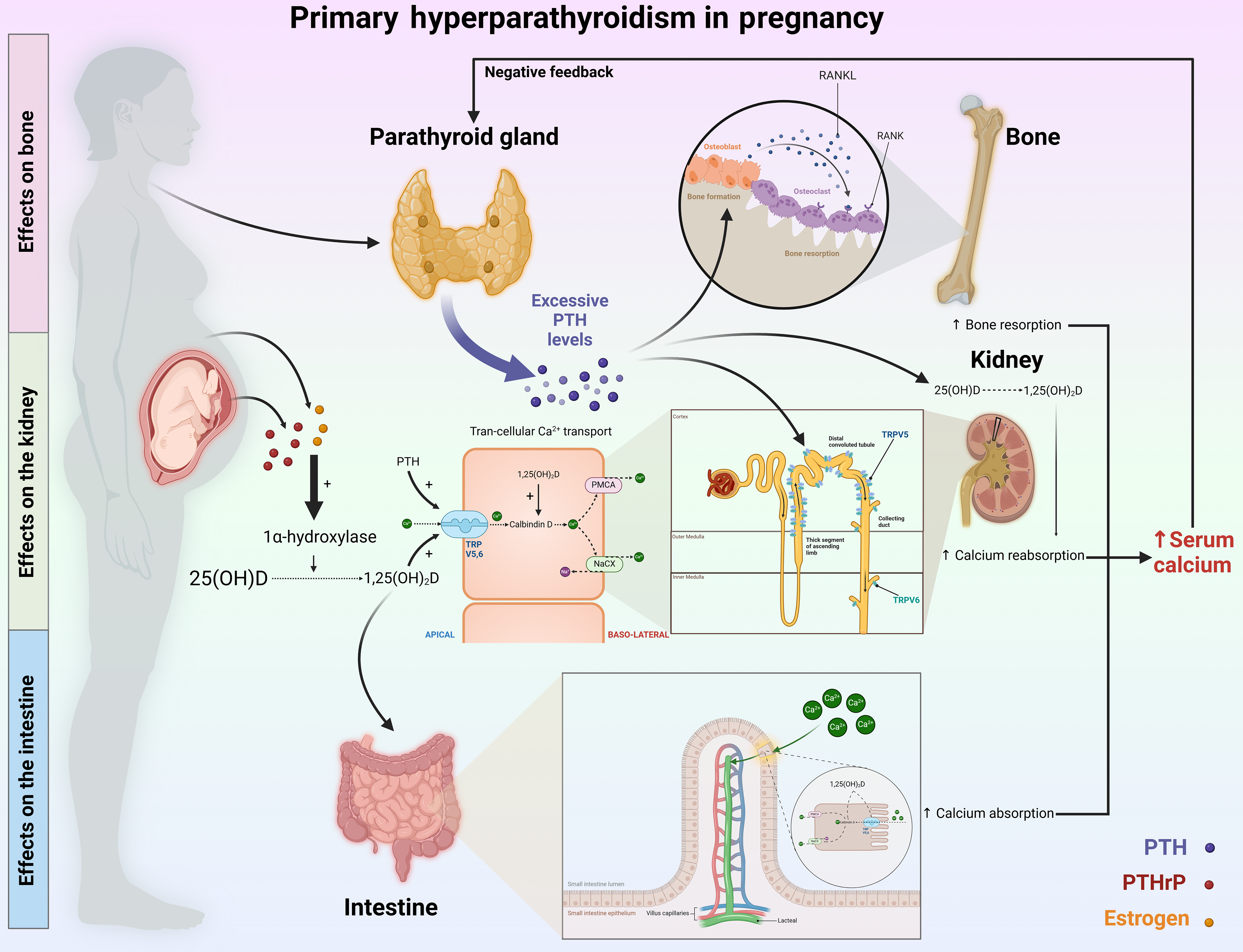
Figure 1 Key mechanisms of calcium regulation in pregnant individuals with primary hyperparathyroidism.
In patients with primary hyperparathyroidism, excessive secretion of parathyroid hormone (PTH) leads to hypercalcemia by impacting bones, kidneys, and intestines. It initiates this process in bones by promoting the secretion of receptor activators of nuclear factor kappa beta ligand, which activates osteoclasts to increase bone resorption, releasing calcium into the bloodstream. Concurrently, in the kidneys, PTH enhances calcium reabsorption by increasing transient receptor potential vanilloid 5 activity and stimulating the enzyme 1α-hydroxylase, which is crucial for converting vitamin D into its active form, 1,25-dihydroxyvitamin D, which is essential for effective calcium metabolism. PTH also indirectly influences intestinal calcium and phosphate absorption by upregulating transport proteins such as transient receptor potential vanilloid 6, calbindin, and adenosine triphosphate-dependent calcium pumps. During pregnancy, the situation is compounded by increased levels of estrogen and PTH-related protein, which activate 1-alpha hydroxylase, facilitating the conversion of 25-hydroxyvitamin D to calcitriol. This increase in calcitriol levels further increases the expression of calcium transport proteins in the intestines, thereby exacerbating hypercalcemia. PTH: Parathyroid hormone; PTHrP: Parathyroid hormone-related protein; 25(OH)D: 25-hydroxyvitamin D; NACX: Sodium-calcium exchanger; PMCA: Plasma membrane calcium adenosine triphosphatase; RANK: Receptor activator of nuclear factor kappa beta; TRPV5: Transient receptor potential vanilloid 5.
- Citation: Luong TV, Le LD, Nguyen NVD, Dang HNN. Persistent challenges in the diagnosis of acute pancreatitis due to primary hyperparathyroidism during pregnancy. World J Gastroenterol 2025; 31(7): 100973
- URL: https://www.wjgnet.com/1007-9327/full/v31/i7/100973.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i7.100973