Copyright
©The Author(s) 2023.
World J Gastroenterol. Aug 28, 2023; 29(32): 4831-4850
Published online Aug 28, 2023. doi: 10.3748/wjg.v29.i32.4831
Published online Aug 28, 2023. doi: 10.3748/wjg.v29.i32.4831
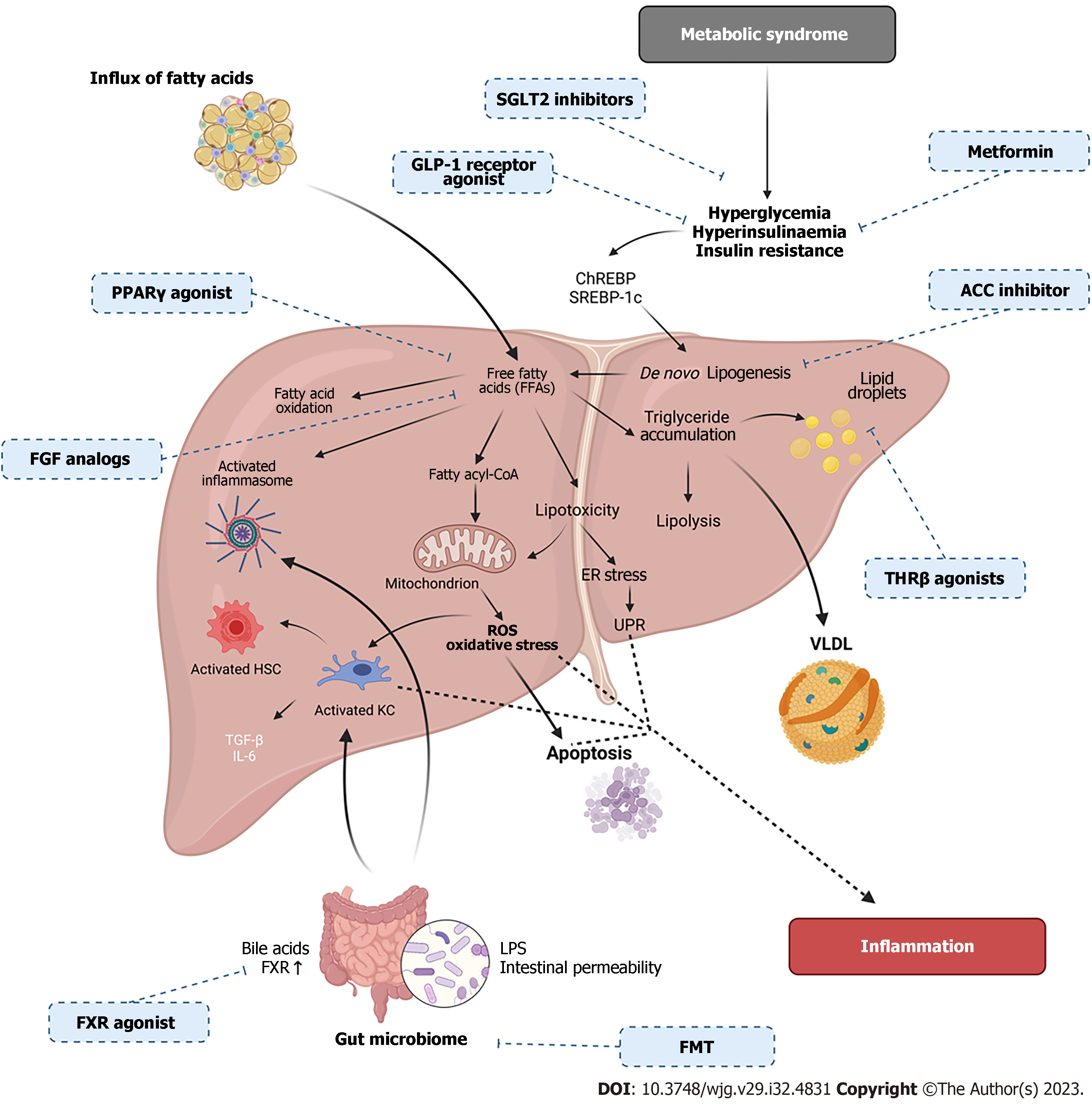
Figure 4 Overview of the metabolic and molecular mechanisms occurring in non-alcoholic fatty liver disease pathogenesis with therapeutic targets.
Non-alcoholic fatty liver disease (NAFLD) is a multifactorial disease, including metabolic syndrome, insulin resistance (IR) and gut microbiome changes. IR and metabolic syndrome cause increased free fatty acids (FFAs) which lead to endoplasmic reticulum stress, reactive oxygen species accumulation, oxidative stress, apoptosis, immune cell activation and inflammasome activation. Changes in the gut barrier can cause changes to bile acids and intestinal permeability causing lipopolysaccharides translocation from the gut causing immune activation, thus, inducing inflammation. FFA’s can also activate transcription factors such as sterol regulatory binding protein-1c and carbohydrate response element binding protein causing the storage of FFAs as triglycerides in lipid droplets. Accumulated triglycerides can be exported as very low-density lipoprotein or oxidized by mitochondrial β-oxidation. Pharmacologic treatments for NAFLD are identified with corresponding drug mechanism of action (created with BioRender.com). ROS: Reactive oxygen species; LPS: Lipopolysaccharide; UPR: Unfolded protein response; FMT: Faecal microbiota transplant; VLDL: Very low-density lipoproteins; PPAR-γ: Peroxisome proliferator-activated receptor-γ; KC: Kupffer cells; HSC: Hepatic stellate cells; FXR: Farnesoid X Receptor; SGLT2: Sodium-glucose cotransporter 2; SREBP-1c: Sterol regulatory binding protein-1c; ChREBP: Carbohydrate response element binding protein.
- Citation: Petagine L, Zariwala MG, Patel VB. Non-alcoholic fatty liver disease: Immunological mechanisms and current treatments. World J Gastroenterol 2023; 29(32): 4831-4850
- URL: https://www.wjgnet.com/1007-9327/full/v29/i32/4831.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i32.4831