Published online Aug 14, 2023. doi: 10.3748/wjg.v29.i30.4701
Peer-review started: May 31, 2023
First decision: July 8, 2023
Revised: July 11, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: August 14, 2023
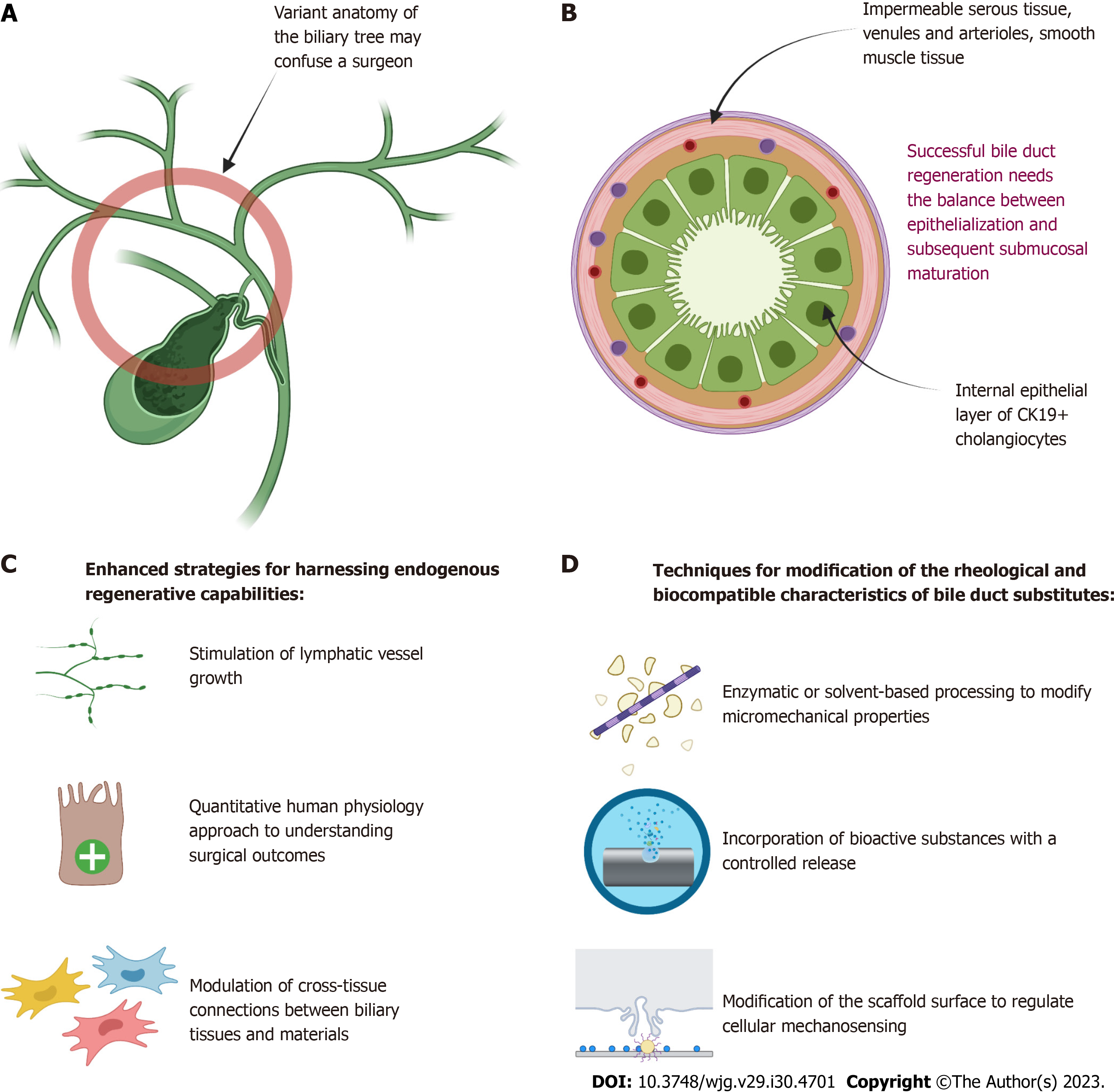
Current abdominal surgery has several approaches for biliary reconstruction. However, the creation of functional and clinically applicable bile duct substitutes still represents an unmet need. In the paper by Miyazawa and colleagues, approaches to the creation of bile duct alternatives were summarized, and the reasons for the lack of development in this area were explained. The history of bile duct surgery since the nineteenth century was also traced, leading to the conclusion that the use of bioabsorbable materials holds promise for the creation of bile duct substitutes in the future. We suggest three ideas that may stimulate progress in the field of bile duct substitute creation. First, a systematic analysis of the causative factors leading to failure or success in the creation of bile duct substitutes may help to develop more effective approaches. Second, the regene
Core Tip: Progress towards the development of clinically applicable bile duct substitutes can be achieved by applying an interdisciplinary approach. This approach should include the utilization of quantitative mathematical methods, principles of cross-tissue interactions for epithelial and submucosal tissues, as well as deep retrospective data analysis of the causes of success and failure in studies on the creation of bile duct substitutes.
- Citation: Klabukov ID, Baranovskii DS, Shegay PV, Kaprin AD. Pitfalls and promises of bile duct alternatives: There is plenty of room in the regenerative surgery. World J Gastroenterol 2023; 29(30): 4701-4705
- URL: https://www.wjgnet.com/1007-9327/full/v29/i30/4701.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i30.4701
We read with great interest the paper by Miyazawa et al[1], who analyzed the drawbacks and advantages of various alternatives for bile ducts. The authors described the current approaches for substituting the bile duct and acknowledged that a suitable graft has not yet been developed due to limited understanding of the mechanisms involved in the healing and regeneration of bile duct tissue. They are convinced that the use of bioabsorbable materials may facilitate the creation of bile duct substitutes in the future.
The authors have fairly mentioned that there is a 100-year history of attempts to create satisfactory bile duct substitutes[2]. However, despite significant advancements in material and life sciences, the development of engineered bile ducts has not been successful. None of the grafts currently available are reliable enough for use in clinical practice. Addi
One of the most valuable features of the paper by Miyazawa et al[1] is the systematization and analysis of the early attempts to create bile duct alternatives, as application of a systematic approach. The authors traced the history of reconstructive hepatobiliary surgery since the 1880s and discussed many intriguing studies. However, we noticed that the causes of negative or positive results are not usually analyzed or systematized in these studies. For example, in the study by Doillon et al[5], it was shown that pre-exposure of a venous graft in glycerol improves surgical outcomes, but the fundamental reasons for such improvement were not investigated in this study, as well as in many other papers.
First, we want to emphasize that the analysis of the causes of negative and positive results is just as important as the results themselves. Additionally, studies that describe the unsuccessful use of rubber tubes[6], polyvinyl chloride[7], silastic[8], lyophilized and siliconized dura mater[9] in both humans and animals are valuable as they shed light on the various causes of postoperative surprises. We believe that a systematic analysis of the factors that contribute to failure or success in creating bile duct substitutes could help develop more effective approaches. It is important to note that such a systematic review has never been conducted before.
Secondly, quantitative methods of analysis can also highlight interesting patterns. Specifically, the studies reviewed by the authors revealed the limitations of bile duct epithelialization, which was found to be approximately 3 cm long and not more than 1-2 mm per week[10-12]. Additionally, the required time for submucosal maturation was estimated to be around 6-12 mo[10,13]. These findings provide support for the hypothesis that there are several deterministic mechanisms of bile duct regeneration that have yet to be discovered and completely understood. Furthermore, this suggests that the regeneration of the bile duct is delicately balanced between epithelialization and subsequent sub
Thirdly, the utilization of the organism’s endogenous regeneration abilities may enhance the effectiveness of bile duct substitutes. Cross-tissue interactions play a crucial role in the process of regeneration, as they determine the normal and pathological proliferation and maturation of tissues[14]. Moreover, in interconnected tissues, not only interactions but also division of labor and competition between different tissues become relevant[15]. This phenomenon has gained significant importance, particularly in relation to the biliary microbiota’s role in inflammatory diseases of the biliary tract[16]. Therefore, the correct surgical approach with incompatible tissues, or the reconstruction of biliary tissues with incompatible materials, may lead to the development of chronic disorders and require additional supplementation. For example, some methods that have been underestimated include the stimulation of not only blood vessel growth but also lymphatic vessel growth in the interstitium, as well as the specific chemotaxis of mesenchymal stromal cells to the site of injury (Figure 1C).
Miyazawa et al[1] have demonstrated a connection between vascularization/angiogenesis and the maturation of biliary glands, as well as the stabilization of inflammation[17]. Considering the recently discovered crucial role played by vascular endothelial growth factor in biliary tree development and cell cycle regulation[18], inducing angiogenesis could be a promising avenue for future research. It is worth noting that the use of grafts may yield varying outcomes, mainly due to differences in their structure, immunogenicity, and vascular density, regardless of whether they are autologous or allogeneic. Therefore, the mechanical (rheological) and cyto compatible properties of the substitute material are important (Figure 1D).
The functional and biomimetic properties of the bile duct substitute are expected to promote the growth of resident cells and facilitate tissue regeneration[19]. However, significant advancements in regenerative medicine necessitate innovative ideas from interdisciplinary fields. The application of mathematical logic to human physiology has the potential to accelerate progress in tissue engineering[20]. For example, the phase space method, well known in physics, can provide new insights into physiological relevance in bioengineering[21]. This promising and novel concept relies on the application of mathematical logic and machine learning to forecast surgical outcomes, commonly referred to as theoretical surgery[22].
We assume that the views of the surgeon and the biophysicist on the same facts and problems differ, particularly in terms of abstract concepts. This highlights the necessity for collaborative work among specialists from various fields (Table 1). We firmly believe that the integration of quantitative methods and retrospective analysis in bioengineering will open up new avenues for developing models of inter-tissue interaction, ultimately yielding groundbreaking outcomes in bile duct engineering.
| Clinical evidences | Understanding of a surgeon | Understanding of a physiologist |
| There are many negative results of the use of materials for bile duct repair | Materials associated with complications are not suitable for clinical practice | The causes of failure are what we need to determine. Can we cluster these causes to understand the underlying mechanisms? If we only consider successful cases, we will commit survival bias and be unable to determine the reasons for successful outcomes |
| Bile duct epithelialization never exceed the following limits: About 3 cm long and growth not more than 1-2 mm per week | We must avoid implanting grafts (autografts) longer than 3 cm. This is an interesting fact. My experience supports these values, so I am aware of the potential outcomes that may be achieved after a surgical procedure | The presence of stable values indicates the conservatism of the underlying regenerative mechanisms, which are not dependent on the surgeon’s skills or the quality of the materials |
| The normal human bile is not sterile and contains both living cholangiocytes and normal biliary microbiota | These are interesting facts, but we still lack the necessary tools to support endogenous regeneration in routine clinical practice. The application of cells remains unproven | The presence of living cells in bile may support the existence of unknown ways for the migration of bile duct cells. These methods need to be discovered and applied for bile duct regeneration |
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Tissue Engineering and Regenerative Medicine International Society, 6416.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Midgley AC, China; Wang G, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Miyazawa M, Aikawa M, Takashima J, Kobayashi H, Ohnishi S, Ikada Y. Pitfalls and promises of bile duct alternatives: A narrative review. World J Gastroenterol. 2022;28:5707-5722. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 2] [Cited by in F6Publishing: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Ahrendt SA, Pitt HA. A history of the bilioenteric anastomosis. Arch Surg. 1990;125:1493-1500. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Kowalczyk KA, Majewski A. Analysis of surgical errors associated with anatomical variations clinically relevant in general surgery. Review of the literature. Transl Res Anat. 2021;23:100107. [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 4. | Żytkowski A, Tubbs RS, Iwanaga J, Clarke E, Polguj M, Wysiadecki G. Anatomical normality and variability: historical perspective and methodological considerations. Transl Res Anat. 2021;23:100105. [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Doillon C, Dureau G, Clendinnen G, Eloy R. Effects of glycerol pretreatment upon biliary or venous grafts in bile duct replacement. Surg Gynecol Obstet. 1981;152:613-620. [PubMed] [Cited in This Article: ] |
| 6. | Sullivan AG. Reconstruction of the Bile Ducts. JAMA. 1909;53:774-777. [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Apalakis A. An experimental evaluation of the types of material used for bile duct drainage tubes. Br J Surg. 1976;63:440-445. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Cantor MO. Silicone rubber t tubes for common duct drainage. Am J Surg. 1964;107:666-668. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Gagni G, Favaretto P, Luzzani A, Ferrini S, Marchi F, Ciprian V, Gadioli P, Mastropasqua D, Dal Cortivo G, Sovran C. Choledochal prostheses with lyophilized and siliconed dura mater. Experimental research; preliminary results. Minerva Chir. 1979;34:1209-1216. [PubMed] [Cited in This Article: ] |
| 10. | Montalvo-Javé EE, Mendoza Barrera GE, Valderrama Treviño AI, Piña Barba MC, Montalvo-Arenas C, Rojas Mendoza F, León Mancilla B, García Pineda MA, Jaime Limón Á, Albores Saavedra J, Tapia-Jurado J. Absorbable bioprosthesis for the treatment of bile duct injury in an experimental model. Int J Surg. 2015;20:163-169. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Heistermann HP, Palmes D, Stratmann U, Hohlbach G, Hierlemann H, Langer M, Spiegel HU. A new technique for reconstruction of the common bile duct by an autologous vein graft and a biodegradable endoluminal stent. J Invest Surg. 2006;19:57-60. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Palmes D, Wolters H, Spiegel HU, M Ller E, Minin E, Heistermann HP. Morphological changes during creation of a neo-bile duct using a vein and a biodegradable endoluminal stent. J Invest Surg. 2009;22:435-444. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Lahey FH, Pyrtek LJ. Experience with the operative management of 280 strictures of the bile ducts, with a description of a new method and a complete follow-up study of the end results in 229 of the cases. Surg Gynecol Obstet. 1950;91:25-56. [PubMed] [Cited in This Article: ] |
| 14. | Cote LE, Feldman JL. Won't You be My Neighbor: How Epithelial Cells Connect Together to Build Global Tissue Polarity. Front Cell Dev Biol. 2022;10:887107. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 4] [Reference Citation Analysis (0)] |
| 15. | Adler M, Moriel N, Goeva A, Avraham-Davidi I, Mages S, Adams TS, Kaminski N, Macosko EZ, Regev A, Medzhitov R, Nitzan M. Emergence of division of labor in tissues through cell interactions and spatial cues. Cell Rep. 2023;42:112412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 7] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 16. | Liu Y, Sun LY, Zhu ZJ, Wei L, Qu W, Zeng ZG. Bile microbiota: new insights into biliary complications in liver transplant recipients. Ann Transl Med. 2020;8:354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Shang H, Zeng JP, Wang SY, Xiao Y, Yang JH, Yu SQ, Liu XC, Jiang N, Shi XL, Jin S. Extrahepatic bile duct reconstruction in pigs with heterogenous animal-derived artificial bile ducts: A preliminary experience. World J Gastroenterol. 2020;26:7312-7324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Mariotti V, Fiorotto R, Cadamuro M, Fabris L, Strazzabosco M. New insights on the role of vascular endothelial growth factor in biliary pathophysiology. JHEP Rep. 2021;3:100251. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Sun Q, Shen Z, Liang X, He Y, Kong D, Midgley AC, Wang K. Progress and Current Limitations of Materials for Artificial Bile Duct Engineering. Materials (Basel). 2021;14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Klabukov ID, Krasilnikova OA, Baranovskii DS. Quantitative human physiology: An introduction guide for advanced tissue engineering. Biotechnol J. 2021;e2100481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 21. | Klabukov I, Tenchurin T, Shepelev A, Baranovskii D, Mamagulashvili V, Dyuzheva T, Krasilnikova O, Balyasin M, Lyundup A, Krasheninnikov M, Sulina Y, Gomzyak V, Krasheninnikov S, Buzin A, Zayratyants G, Yakimova A, Demchenko A, Ivanov S, Shegay P, Kaprin A, Chvalun S. Biomechanical Behaviors and Degradation Properties of Multilayered Polymer Scaffolds: The Phase Space Method for Bile Duct Design and Bioengineering. Biomedicines. 2023;11. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 22. | Lorenz W, Rothmund M. Theoretical surgery: a new specialty in operative medicine. World J Surg. 1989;13:292-299. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |