Copyright
©The Author(s) 2022.
World J Gastroenterol. Dec 21, 2022; 28(47): 6662-6688
Published online Dec 21, 2022. doi: 10.3748/wjg.v28.i47.6662
Published online Dec 21, 2022. doi: 10.3748/wjg.v28.i47.6662
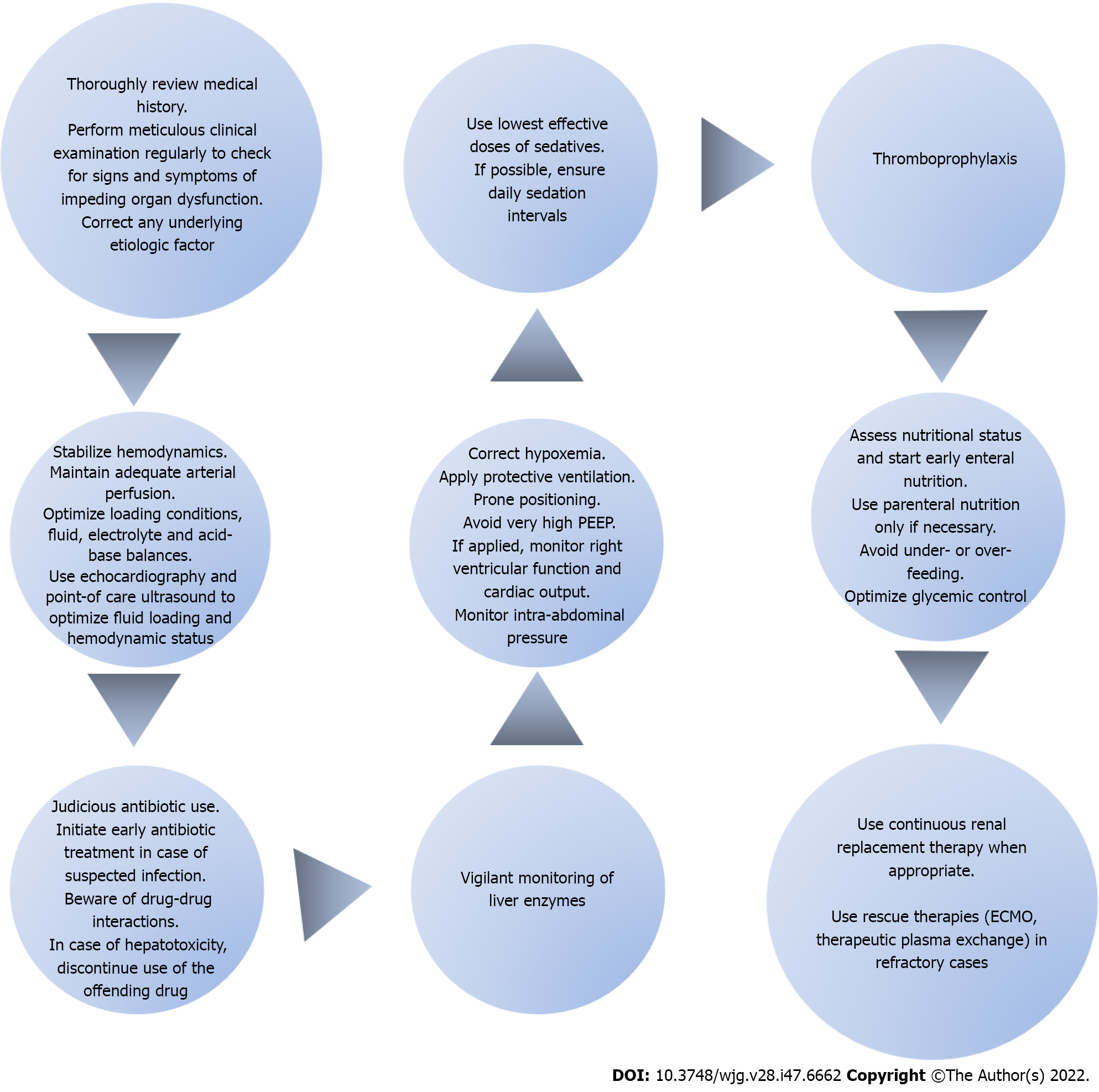
Figure 2 Steps of the intensive care unit therapeutic approach in patients with coronavirus disease 2019 induced acute liver injury.
The intensive care unit (ICU) therapeutic approach for coronavirus disease 2019 patients with acute liver injury (ALI) lies in preventive measures and is exclusively supportive once ALI ensues. After obtaining a detailed medical history, a thorough physical examination should be performed on a regular basis. Upon recognition of any signs of impeding liver dysfunction, the possible etiologic factor should be systematically sought and appropriately addressed. Hemodynamic stabilization of the patient is of paramount importance. The goal is to maintain adequate arterial perfusion in order to prevent liver ischemia. The use of echocardiography and point-of-care ultrasonography will help determine the hemodynamic status and optimize loading conditions. It is important to constantly maintain fluid, electrolyte and acid-base balances. Furthermore, early identification and management of sepsis cannot be overemphasized. Prompt initiation of appropriate antibiotic therapy is the mainstay of sepsis management. Antibiotics should be used judiciously with an increased level of awareness for possible drug-drug interactions. In case of hepatotoxicity, the administration of the responsible pharmacologic agent should be discontinued. Close monitoring of liver enzymes is advised at all times. Furthermore, hypoxia should be consistently addressed and corrected. In mechanically ventilated patients, a lung-protective ventilation strategy should be implemented with the use of low tidal volumes coupled with a target of plateau pressure < 30 cm H2O. The application of very high positive end-expiratory pressure should be avoided because it could compromise right ventricular performance and precipitate passive liver congestion. Moreover, prone positioning is recommended in order to improve hypoxia. Intra-abdominal pressure should also be monitored so as to prevent any potential increases related to mechanical ventilation which could jeopardize liver function. Additionally, optimal sedation strategies should be applied with the lowest effective doses and daily sedation intervals. Thromboprophylaxis is strongly recommended as a preventive measure in all ICU patients. Besides that, nutritional status should be regularly assessed and efforts should focus on initiating early enteral feeding while avoiding parenteral nutrition. Under- or over- feeding should be avoided and glycemic control should be optimized. Finally, renal replacement therapy can be used whenever indicated. In refractory cases, rescue therapies may be employed with the use of extracorporeal membrane oxygenation and therapeutic plasma exchange in an attempt to provide circulatory and respiratory support and reverse end-organ failure. PEEP: Positive end-expiratory pressure; ECMO: Extracorporeal membrane oxygenation.
- Citation: Polyzogopoulou E, Amoiridou P, Abraham TP, Ventoulis I. Acute liver injury in COVID-19 patients hospitalized in the intensive care unit: Narrative review. World J Gastroenterol 2022; 28(47): 6662-6688
- URL: https://www.wjgnet.com/1007-9327/full/v28/i47/6662.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i47.6662