Copyright
©The Author(s) 2021.
World J Gastroenterol. Jun 7, 2021; 27(21): 2850-2870
Published online Jun 7, 2021. doi: 10.3748/wjg.v27.i21.2850
Published online Jun 7, 2021. doi: 10.3748/wjg.v27.i21.2850
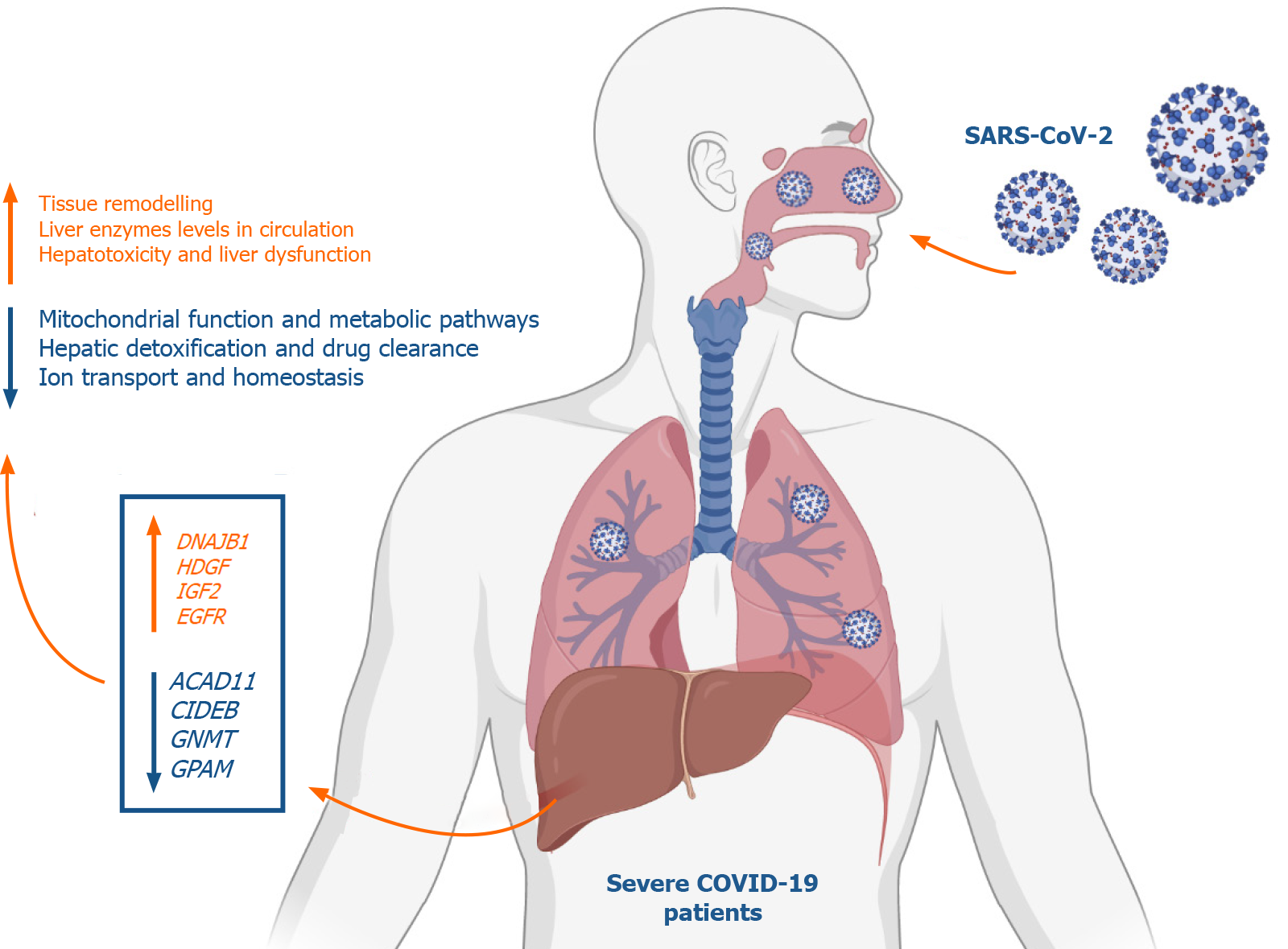
Figure 9 Summary of the study findings.
At advanced stages, severe acute respiratory syndrome coronavirus 2 infection appears to elicit transcriptional shifts in liver tissue resulting in increased G-coupled protein receptors signaling, tissue remodeling, transmembrane transport, vesicle formation and cell projections morphogenesis. On the other hand, metabolic and biosynthetic pathways including metabolism of drugs and xenobiotics as well as mitochondrial processes and ions homeostasis regulatory mechanisms appear to be suppressed in coronavirus disease 2019 (COVID-19) patients. In response to these transcriptional shifts, we speculate that severe COVID-19 patients would be subjected to hepatic injury and tissue remodeling which may results in the clinically observed liver dysfunction, low liver detoxification capacity and increased liver enzymes. Figure was created with BioRender.com. DNAJB1: DnaJ heat shock protein family (Hsp40) member B1; HDGF: Hepatoma-derived growth factor; IGF2: Insulin growth factor 2; EGFR: Epidermal growth factor receptor; ACAD11: Acyl-CoA dehydrogenases 11; CIDEB: Cell death-inducing DNA fragmentation factor alpha-like effector B; GNMT: Glycine N-methyltransferase; GPAM: Glycerol-3-phosphate acyltransferase and metabolism.
- Citation: Hammoudeh SM, Hammoudeh AM, Bhamidimarri PM, Mahboub B, Halwani R, Hamid Q, Rahmani M, Hamoudi R. Insight into molecular mechanisms underlying hepatic dysfunction in severe COVID-19 patients using systems biology. World J Gastroenterol 2021; 27(21): 2850-2870
- URL: https://www.wjgnet.com/1007-9327/full/v27/i21/2850.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i21.2850