Copyright
©The Author(s) 2020.
World J Gastroenterol. Jan 28, 2020; 26(4): 383-392
Published online Jan 28, 2020. doi: 10.3748/wjg.v26.i4.383
Published online Jan 28, 2020. doi: 10.3748/wjg.v26.i4.383
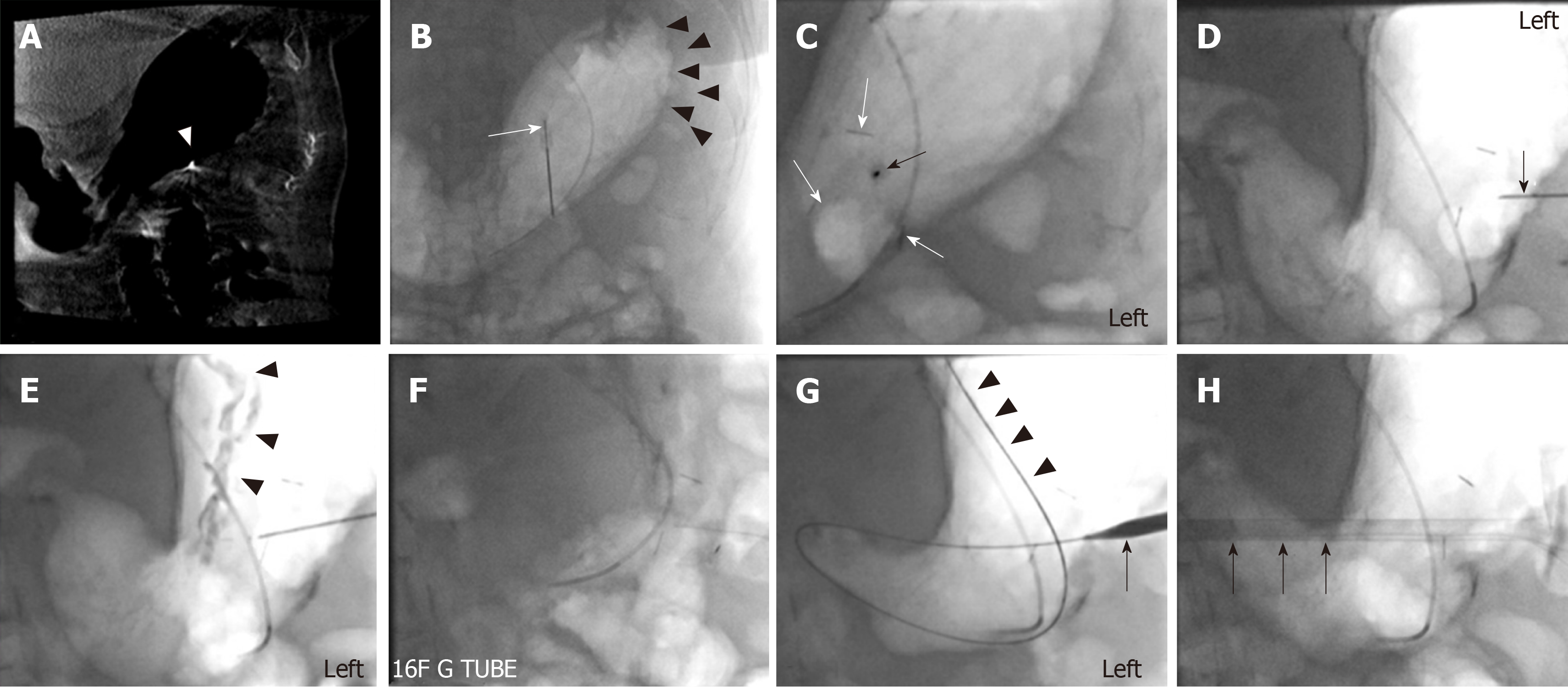
Figure 4 Ninety-four-year-old female with a history of moderately differentiated adenocarcinoma of the esophagus referred for percutaneous gastrostomy tube placement.
A 16-French gastrostomy tube was placed through a 20-French peel-away sheath. Procedure time was 21 min. Fluoroscopy time was 6 min 18 s and Air Kerma was 81.5 mGy. The gastrostomy tube was started to be used for enteral feeding 24 h after the procedure. A: A pre-procedural cone-beam CT was obtained since no CT abdomen was available. A 5-French MPA catheter was placed along with a 0.035 Glidewire. The stomach was manually inflated with air. Arrowhead points to a 21-gauge short local anesthetic needle left in place for entry site planning; B: Placement of the first T-bar fastener (white arrow). Again, note the inflated stomach (arrowheads); C: Note the three T-bar fasteners as linear densities (white arrows). An 18-French needle was visualized at the access site in the left anterior oblique projection lined. The needle (black arrow) was in line with the radiation beam and was aiming towards the antrum and pylorus; D: In the right anterior oblique projection, the depth of the needle (black arrow) can be visualized penetrating the gastric wall; E, F: With iodinated contrast injection, the gastric rugae (arrowheads) could be visualized, thus confirming the intragastric location of the needle; G: The advancement of the 0.035 Amplatz wire (arrowheads) over the needle was pursued. After subsequent tract dilatation the peel-way sheath (arrow) was advanced over the Amplatz; H: The gastrostomy tube (arrow) was advanced through the peel-away sheath. After completion of the procedure the MPA catheter was removed.
- Citation: Partovi S, Li X, Moon E, Thompson D. Image guided percutaneous gastrostomy catheter placement: How we do it safely and efficiently. World J Gastroenterol 2020; 26(4): 383-392
- URL: https://www.wjgnet.com/1007-9327/full/v26/i4/383.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i4.383