Copyright
©The Author(s) 2020.
World J Gastroenterol. Jan 28, 2020; 26(4): 383-392
Published online Jan 28, 2020. doi: 10.3748/wjg.v26.i4.383
Published online Jan 28, 2020. doi: 10.3748/wjg.v26.i4.383
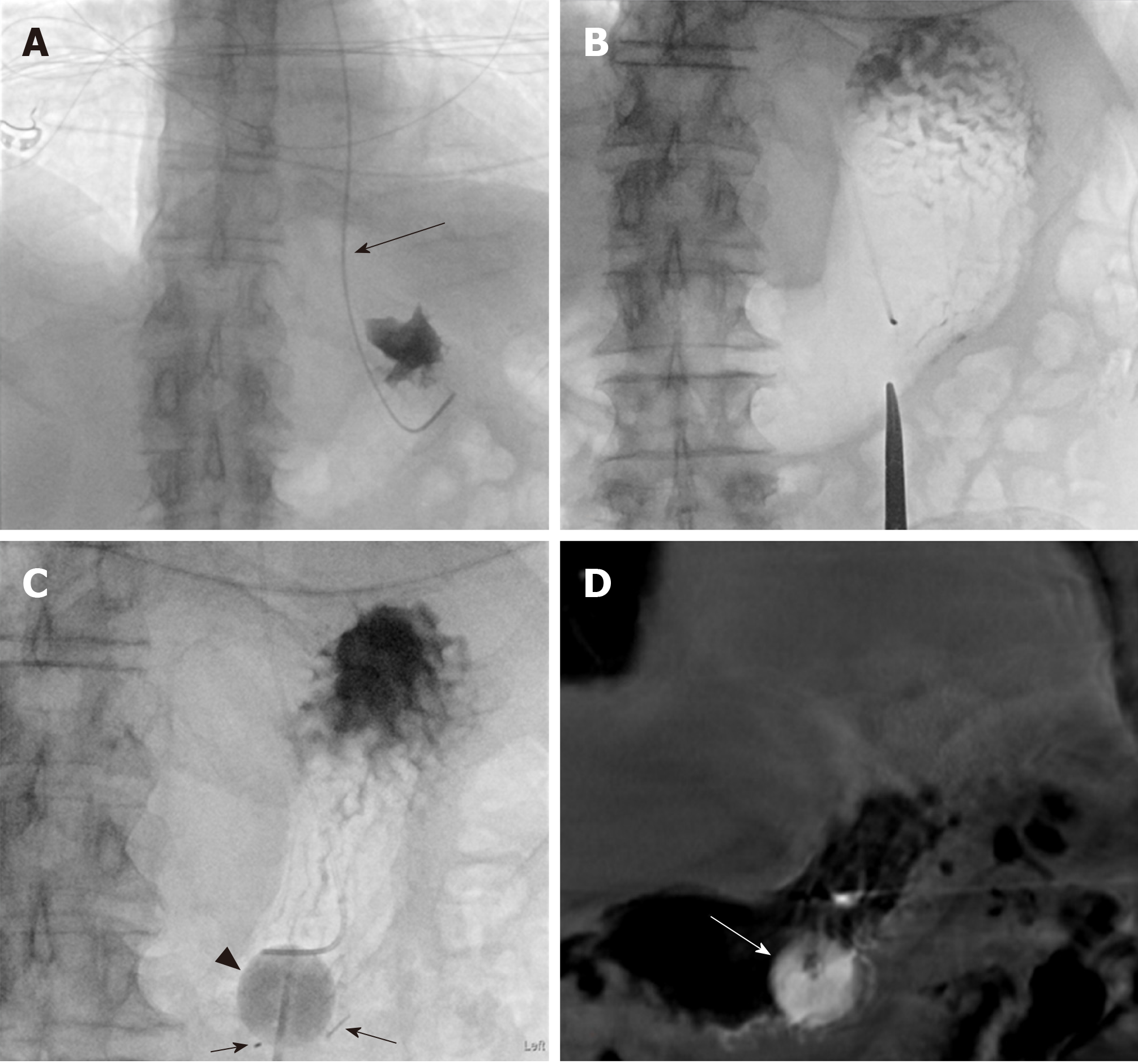
Figure 2 Eighty-one-year-old male with a past medical history of diabetes mellitus, hypertension, perforated diverticulitis status post resection with colostomy and adenocarcinoma of the esophagus status post neoadjuvant chemotherapy.
Patient was admitted for failure to thrive and percutaneous gastrostomy tube placement was requested. An 18-French Entuit gastrostomy tube was placed within a 22-French peel-away sheath. The procedure time was 44 min. Fluoroscopy time was 8 min 6 s and Air Kerma was 280 mGy. This procedure was challenging due to the inability to keep the stomach inflated and glucagon was avoided given the medical history of diabetes mellitus. The gastrostomy tube was started to be used for enteral feeding 24 h after the procedure. A: Advancement of a 5-French MPA catheter (arrow) into the stomach along with a 0.035 Glidewire. The position of the MPA catheter was confirmed with a small amount of iodinated contrast injection; B: Insufflation of the stomach with air though the MPA catheter. A hemostat was used to mark the entry site; C: Placement of the three T-bar fasteners (arrows) as well as the gastrostomy tube with balloon inflated using a mixtures of sterile water with minimal amount of contrast (arrowhead); D: A post-procedural cone-beam computed tomography was performed due to the challenge of keeping the stomach insufflated with air. The cone beam computed tomography showed the gastrostomy tube with the inflated balloon (arrow) in the gastric body. Of note the gastrostomy balloon appears slightly radiopaque due to inflation using a mixture of sterile water with minimal amount of contrast. After completion of the procedure the 5-French MPA catheter was removed.
- Citation: Partovi S, Li X, Moon E, Thompson D. Image guided percutaneous gastrostomy catheter placement: How we do it safely and efficiently. World J Gastroenterol 2020; 26(4): 383-392
- URL: https://www.wjgnet.com/1007-9327/full/v26/i4/383.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i4.383