Copyright
©The Author(s) 2019.
World J Gastroenterol. Mar 28, 2019; 25(12): 1457-1464
Published online Mar 28, 2019. doi: 10.3748/wjg.v25.i12.1457
Published online Mar 28, 2019. doi: 10.3748/wjg.v25.i12.1457
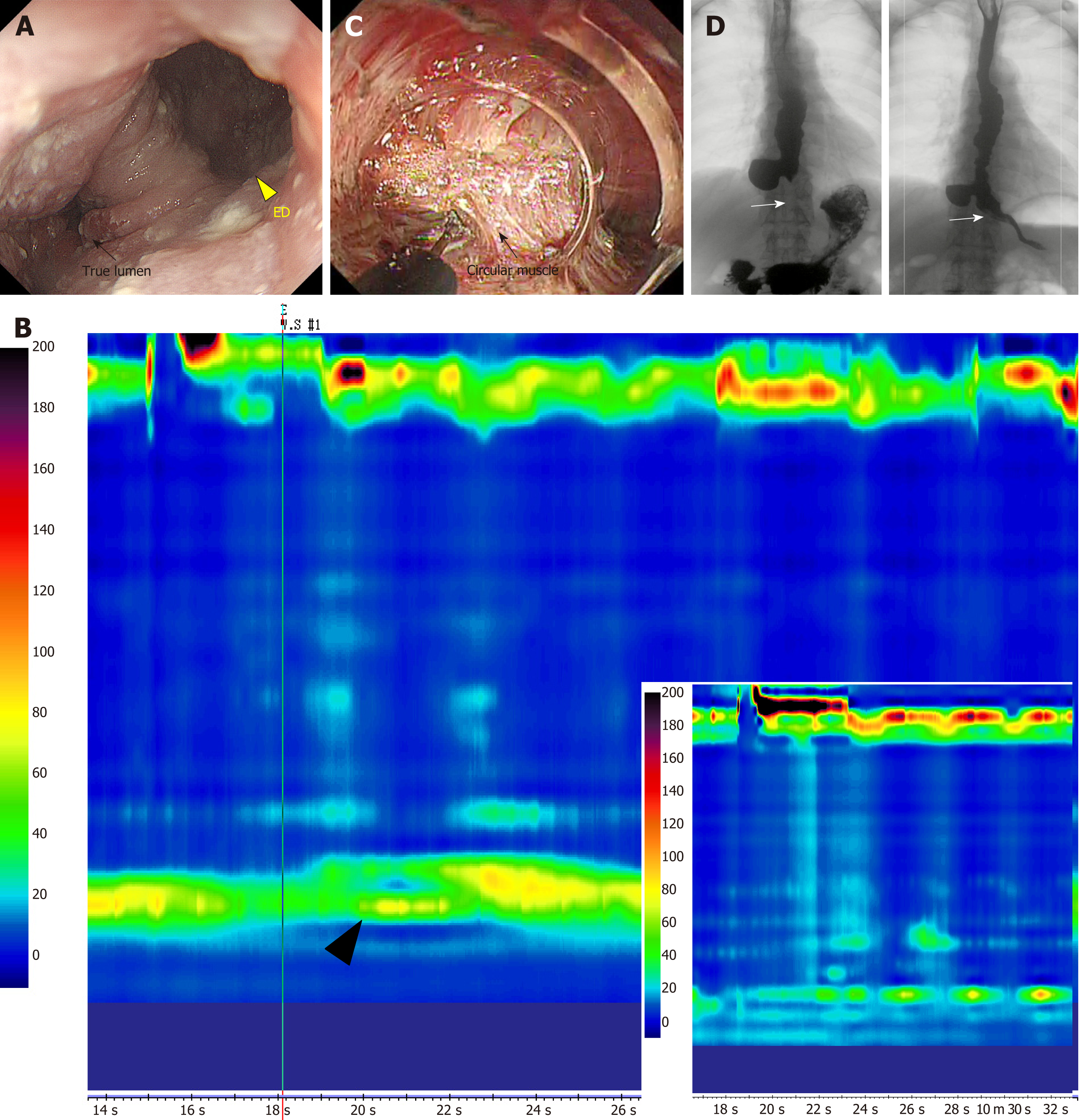
Figure 1 Epiphrenic diverticulum with achalasia treated using salvage peroral endoscopic myotomy.
A: A giant epiphrenic diverticulum (yellow triangle) is visible in the right anterior wall through gastrointestinal endoscopy. The true lumen is compressed and never opens (black arrow); B: On high resolution manometry (HRM), the mean lower esophageal sphincter (LES) pressure is elevated (black triangle) and no normal peristalsis is observed. The patient is diagnosed with type I achalasia. The right lower insert shows the HRM findings after salvage peroral endoscopic myotomy (s-POEM), showing decreased LES pressure; C: s-POEM: Posterior wall myotomy (of the side opposite to the diverticulum, black arrow) is performed longitudinally from the oral terminus of the diverticulum to the gastric terminus, through the LES; D: Preoperative esophagography (left) showing barium inflow into the diverticulum. Some stagnant barium is observed in the mid to lower esophagus. After s-POEM (right), barium flow through the true lumen shows significant improvement and pathologic muscle contraction in the LES area is relieved (white arrow). ED: Epiphrenic diverticulum.
- Citation: Sato H, Takeuchi M, Hashimoto S, Mizuno KI, Furukawa K, Sato A, Yokoyama J, Terai S. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol 2019; 25(12): 1457-1464
- URL: https://www.wjgnet.com/1007-9327/full/v25/i12/1457.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i12.1457