Copyright
©The Author(s) 2017.
World J Gastroenterol. Sep 28, 2017; 23(36): 6694-6704
Published online Sep 28, 2017. doi: 10.3748/wjg.v23.i36.6694
Published online Sep 28, 2017. doi: 10.3748/wjg.v23.i36.6694
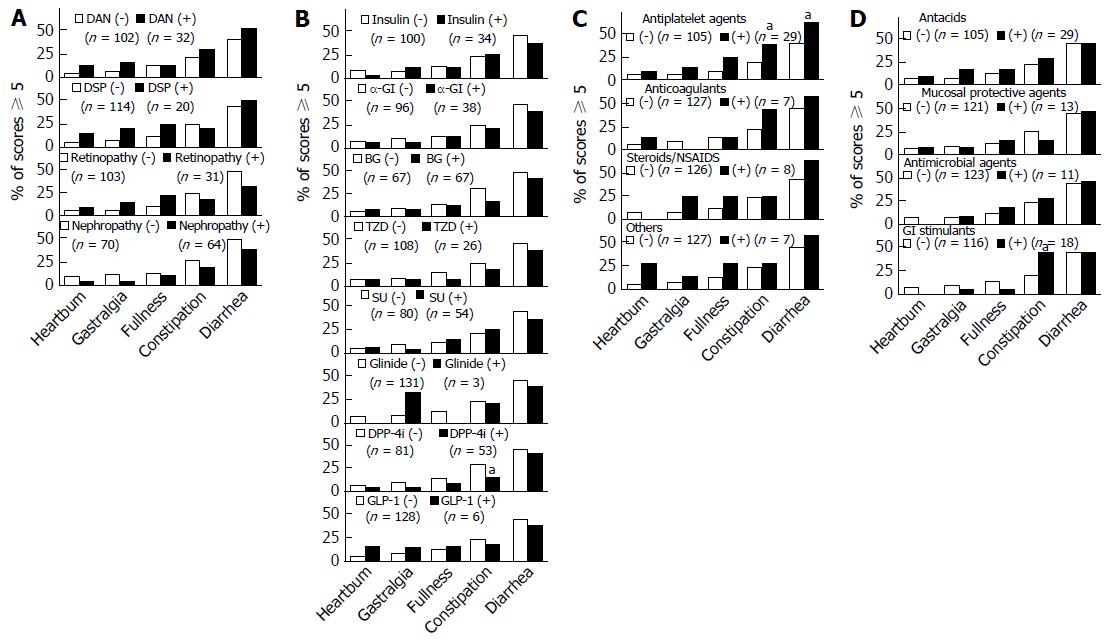
Figure 3 Relationships between various parameters and gastrointestinal symptoms involving each gastrointestinal region (“Heartburn” for esophagus, “Gastralgia” and “Postprandial Fullness” for upper abdomen, and “Constipation” and “Diarrhea” for lower abdomen).
Bars: White indicates the absence and black the presence of each parameter. The percentages of subjects with a score of 5 or higher, for each GI region, considered to be sufficiently symptomatic to cause impaired quality of life, are shown. aP < 0.05, significant difference between presence and absence of each parameter, as analyzed by Fisher’s exact test. A: Comparison between subjects with and without diabetic microangiopathy. The indicated percentages were obtained by dividing the number of subjects with a score of 5 or higher by the total number of patients in the same group (with or without diabetic microangiopathy); B: Comparisons between groups of patients with and without antidiabetic agent administration; C: Comparisons between groups of patients with and without antithrombotic or anti-inflammatory agents. ‘Others’ includes other antithrombotic agents such as prostaglandin E1 derivatives, prostaglandin I2 derivatives, or ethyl esters of eicosapentaenoic acid; D: Comparisons between groups of patients with and without GI agents. αGI: Alpha-glucosidase inhibitors; DAN: Diabetic autonomic neuropathy; DPP-4i: Dipeptidyl-peptidase 4 inhibitor; DSP: Distal symmetric polyneuropathy; GI: Gastrointestinal; GLP-1: Glucagon-like peptide-1; NSAIDs: Nonsteroidal anti-inflammatory drugs; SU: Sulphonyl urea; TZD: Thiazolidinedione.
- Citation: Fujishiro M, Kushiyama A, Yamazaki H, Kaneko S, Koketsu Y, Yamamotoya T, Kikuchi T, Sakoda H, Suzuki R, Kadowaki T. Gastrointestinal symptom prevalence depends on disease duration and gastrointestinal region in type 2 diabetes mellitus. World J Gastroenterol 2017; 23(36): 6694-6704
- URL: https://www.wjgnet.com/1007-9327/full/v23/i36/6694.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i36.6694