Copyright
©The Author(s) 2017.
World J Gastroenterol. Jul 14, 2017; 23(26): 4779-4787
Published online Jul 14, 2017. doi: 10.3748/wjg.v23.i26.4779
Published online Jul 14, 2017. doi: 10.3748/wjg.v23.i26.4779
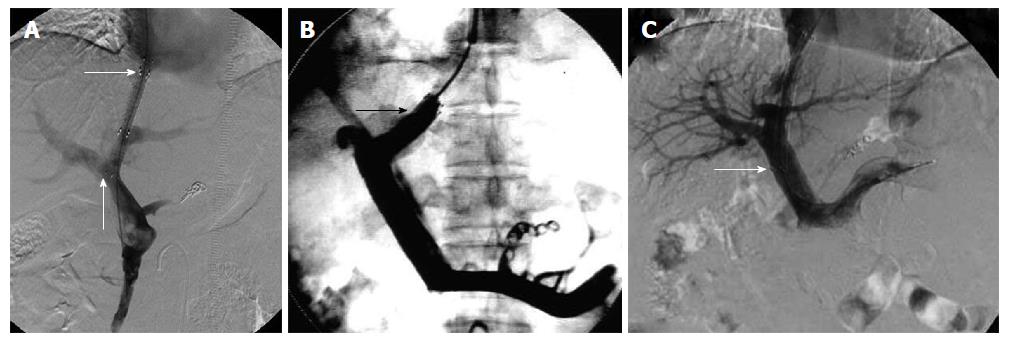
Figure 1 Stent was positioned as described in the study design for each group.
A: Ideal position of the stent endpoint in the TIPS procedure. The transverse arrow indicates the proximal end of the stent at the junction of the hepatic vein and IVC. No angle was formed between the stent and left branch of the portal vein. The proximal end of the stent was located at the junction of the hepatic vein and IVC and did not cause stenosis or occlusion, and did not affect liver transplantation. The arrow pointing up indicates the distal end of the stent located at the left branch of the portal vein. The stent was in parallel to the direction of blood flow, therefore, it was not easy to cause stent stenosis or occlusion; B: The proximal end of the stent in the hepatic vein in the TIPS procedure. The arrow indicates the proximal end of the stent in the hepatic vein. The stent endpoint caused stenosis or occlusion due to blood flow shear force and vascular intimal hyperplasia; C: Distal end of the stent in the main hepatic vein in the TIPS procedure. The arrow indicates the distal end of the stent in the main hepatic vein in the transjugular intrahepatic portosystemic shunt procedure. The distal end of the stent was prone to stimulate the blood vessel wall and interfered with the portal vein blood flow. The stent endpoint caused stenosis or occlusion due to blood flow shear force and vascular intimal hyperplasia. TIPS: Transjugular intrahepatic portosystemic shunt; IVC: Inferior vena cava.
- Citation: Luo SH, Chu JG, Huang H, Yao KC. Effect of initial stent position on patency of transjugular intrahepatic portosystemic shunt. World J Gastroenterol 2017; 23(26): 4779-4787
- URL: https://www.wjgnet.com/1007-9327/full/v23/i26/4779.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i26.4779