Copyright
©The Author(s) 2017.
World J Gastroenterol. Jun 28, 2017; 23(24): 4369-4380
Published online Jun 28, 2017. doi: 10.3748/wjg.v23.i24.4369
Published online Jun 28, 2017. doi: 10.3748/wjg.v23.i24.4369
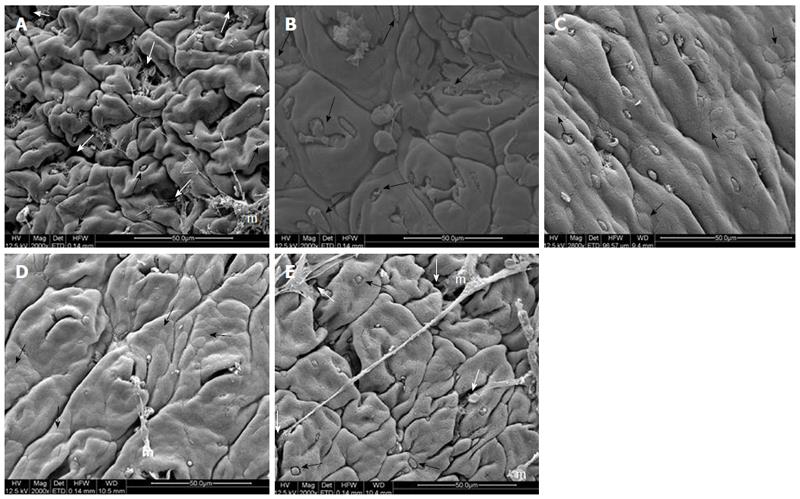
Figure 3 Electromicrographs (scanning electron microscopy) of colon samples from different experimental groups.
Crypts (white arrows), goblet cells (black arrows) and mucin (m). In A (non-colitic group): regular mucosal architecture with polygonal units as structural subunits, regular microvilli giving a smooth velvety appearance, crypts (white arrows), goblet cells (black arrows) and mucin (m) extruded; In B (TNBS control group): complete loss of the smooth velvety appearance and polygonal shape of absorptive cells, hyperplasia of goblet cells (white arrows), absence of mucin extrusion and crypts, characteristics of ulcerative colitis and Crohn’s disease; In C (PACO2 25 mg/kg-treated group): slight recovery of polygonal shape (black arrows) of absorptive cells, however the number of goblet cells remained elevated; In D (PACO2 50 mg/kg-treated group): smaller number of goblet cells, greater recovery of polygonal appearance (black arrows) and increased mucin (m) compared to TNBS control group; In E (PACO2 100mg/kg-treated group): good recovery of mucosa architecture, with goblet cells (black arrows) similar to healthy animals including crypts (white arrows) and mucin (m) for protection.
- Citation: Almeida Junior LD, Quaglio AEV, de Almeida Costa CAR, Di Stasi LC. Intestinal anti-inflammatory activity of Ground Cherry (Physalis angulata L.) standardized CO2 phytopharmaceutical preparation. World J Gastroenterol 2017; 23(24): 4369-4380
- URL: https://www.wjgnet.com/1007-9327/full/v23/i24/4369.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i24.4369