Copyright
©The Author(s) 2017.
World J Gastroenterol. Jun 7, 2017; 23(21): 3934-3944
Published online Jun 7, 2017. doi: 10.3748/wjg.v23.i21.3934
Published online Jun 7, 2017. doi: 10.3748/wjg.v23.i21.3934
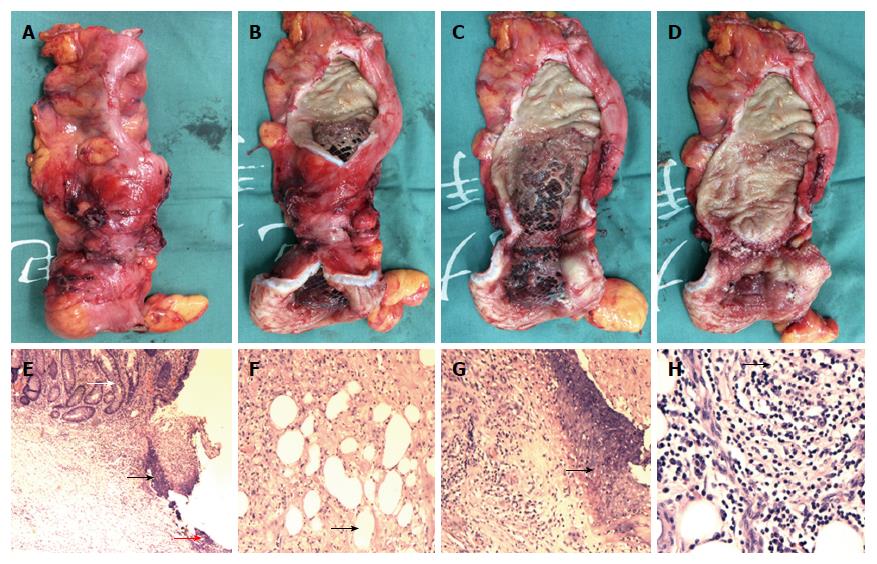
Figure 10 Specimen and pathological analysis.
The resected specimen showed stenotic sigmoid colon (A and B), with obvious compression by the metallic stent visible (C and D). Pathological analysis showed multiple ulcers in the mucosa (E, black arrow head), with the deepest ulcer penetrating through the muscle layer and reaching the mesenteric adipose tissue (F and H, black arrow head). Fibrous scar tissue (E, red arrow head) was visible at the ulcer base (G, black arrow head), but the structure of the mucosa around the ulcer was roughly normal (E, white arrow head), with no granuloma, vasculitis, lymphatic tissue hyperplasia, or full-thickness inflammatory changes (E-H). Hematoxylin and eosin staining; magnification of × 40 for E, × 100 for F and G, × 200 for H.
- Citation: Zhang ZM, Lin XC, Ma L, Jin AQ, Lin FC, Liu Z, Liu LM, Zhang C, Zhang N, Huo LJ, Jiang XL, Kang F, Qin HJ, Li QY, Yu HW, Deng H, Zhu MW, Liu ZX, Wan BJ, Yang HY, Liao JH, Luo X, Li YW, Wei WP, Song MM, Zhao Y, Shi XY, Lu ZH. Ischemic or toxic injury: A challenging diagnosis and treatment of drug-induced stenosis of the sigmoid colon. World J Gastroenterol 2017; 23(21): 3934-3944
- URL: https://www.wjgnet.com/1007-9327/full/v23/i21/3934.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i21.3934