Copyright
©The Author(s) 2016.
World J Gastroenterol. Dec 28, 2016; 22(48): 10482-10501
Published online Dec 28, 2016. doi: 10.3748/wjg.v22.i48.10482
Published online Dec 28, 2016. doi: 10.3748/wjg.v22.i48.10482
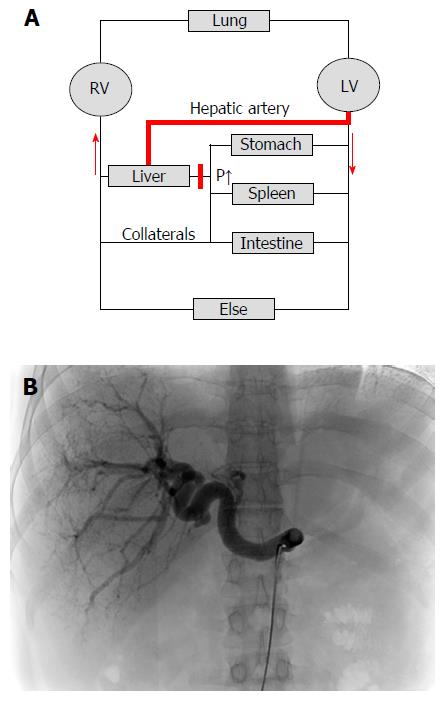
Figure 5 Cirrhotic livers are primarily supplied with blood by the hepatic artery (arterialization).
A: Hemodynamics of the low-pressure organ liver in the context of systemic circulation. Cirrhosis causes an increased vascular resistance, collateral formation and increased hepatic arterial flow to maintain hepatic perfusion. Elevated hepatic arterial flow can be observed already before the onset of fibrosis. It eventually leads to a complete arterialization of the cirrhotic liver. In some cases, portal flow completely reverses (so called hepatofugal flow) and hepatic blood exits the liver both via hepatic and portal veins. Note that the blood circulation (red arrows) is functionally maintained by two serial pumps (RV and LV). A dysbalance of these two pumps such as observed during right heart failure can also cause higher SP (congestion) and ultimately cardiac liver cirrhosis; B: Cirrhotic livers are characterized by predominant arterial blood supply. CT angiography of a patient with liver cirrhosis showing a prominent hepatic artery in 31 years old female patient with cryptogenic liver cirrhosis Child A (courtesy of Dr. B. Radeleff, University of Heidelberg). Under such conditions, the hepatic artery supplies the liver with more than 80% of blood. RV: Right ventricle; LV: Left ventricle; CT: Computed tomography.
- Citation: Mueller S. Does pressure cause liver cirrhosis? The sinusoidal pressure hypothesis. World J Gastroenterol 2016; 22(48): 10482-10501
- URL: https://www.wjgnet.com/1007-9327/full/v22/i48/10482.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i48.10482