Published online Nov 7, 2016. doi: 10.3748/wjg.v22.i41.9247
Peer-review started: June 5, 2016
First decision: July 29, 2016
Revised: August 9, 2016
Accepted: August 23, 2016
Article in press: August 23, 2016
Published online: November 7, 2016
Hepatic epithelioid hemangioendothelioma (HEHE) is a rare category of vascular tumor with uncertain malignant potential. It commonly presents nonspecific and variable clinical manifestations, ranging from asymptomatic to hepatic failure. In addition, laboratory measurements and imaging features also lack specificity in the diagnosis of HEHE. The aim of the present study is to highlight the dilemma and challenges in the preoperative diagnosis of HEHE, and to enhance awareness of the range of hepatobiliary surgery available in patients with multiple hepatic nodular lesions on imaging. In these patients, HEHE should at least be considered in the differential diagnosis.
Core tip: Hepatic epithelioid hemangioendothelioma (HEHE) is a rare category of vascular tumor with uncertain malignant potential. In the present study, by illustrating a case, we aimed to highlight the dilemma and challenges in the preoperative diagnosis of HEHE, and to enhance awareness of the range of hepatobiliary surgery available in patients with multiple hepatic nodular lesions on imaging. In these patients, HEHE should at least be considered in the differential diagnosis.
- Citation: Hu HJ, Jin YW, Jing QY, Shrestha A, Cheng NS, Li FY. Hepatic epithelioid hemangioendothelioma: Dilemma and challenges in the preoperative diagnosis. World J Gastroenterol 2016; 22(41): 9247-9250
- URL: https://www.wjgnet.com/1007-9327/full/v22/i41/9247.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i41.9247
Originating from endothelial cells, hepatic epithelioid hemangioendothelioma (HEHE) is a rare category of vascular tumor with uncertain malignant potential, and some present as slow-growing lesions while others are rapidly progressive tumors[1,2]. HEHE was first identified by Ishak et al[3] in 1984 and usually presents as a multi-nodular lesion imitating metastases with low-to-intermediate grade malignancy[1,3-5]. Based on radiological imaging, HEHE can be classified into a solitary nodular or diffuse nodular phenotype. The clinical biological features of HEHE are similar to those of a benign hemangioma and malignant angiosarcoma[6]. HEHE is resistant to chemotherapy and radiotherapy, thus, complete surgical resection is performed in patients with early stage monolobar disease, and liver transplantation is the only curative treatment in specific patients with diffuse liver involvement[7-9]. However, HEHE commonly presents nonspecific and variable clinical manifestations, ranging from asymptomatic to portal hypertension, Budd-Chiari syndrome or hepatic failure[10,11]. In addition, laboratory measurements also lack specificity in the diagnosis of HEHE, which typically manifests as a “halo” sign and “capsular retraction” on imaging[3,12]. However, most lesions have nonspecific features. Thus, the preoperative diagnosis of HEHE is difficult and most previously published cases were misdiagnosed as metastatic carcinoma, hepatocellular carcinoma, cholangiocarcinoma, or other types of vascular lesions preoperatively[13,14].
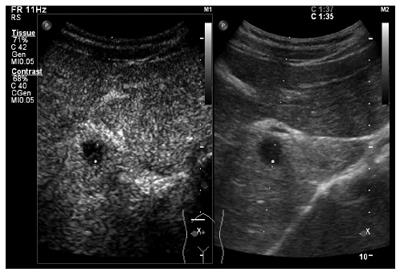
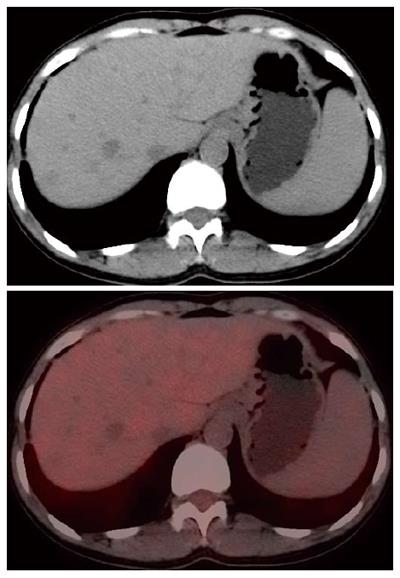
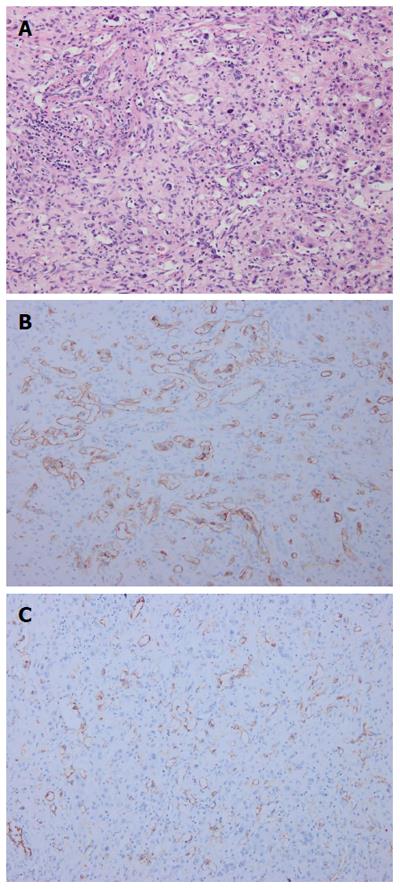
We report a patient whose primary diagnosis was metastatic carcinoma while the final pathological diagnosis was HEHE. The 40-year-old female patient was investigated due to persistent right epigastric pain for more than two months. She had no previous history of gastrointestinal or immunological diseases or previous surgical history. Physical examination was unremarkable. Laboratory tests, including liver biochemical tests, routine blood examination and serum tumor markers, were all within the normal range. Serological testing for hepatitis B and C were also negative. Abdominal contrast-enhanced computerized tomography revealed multiple low density nodular lesions scattered in the liver parenchyma, involving the right lobe and left medial segment, with inhomogeneous enhancement (Figure 1). Contrast-enhanced ultrasonography indicated multiple hypoechoic nodules with peripheral hyper-enhancement during the arterial phase and hypo-enhancement during the portal phase (Figure 2). Thus, an initial diagnosis of metastatic carcinoma was made and 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) was then performed. The hepatic masses showed low glycometabolism (Figure 3) and no specific primary lesion was found, precluding metastases. We then obtained intraoperative frozen sections and the patient underwent extended right hemihepatectomy with complete resection of all lesions under the guidance of intraoperative ultrasonography. The lesions were grey-white in color and ranged in size from 0.7 to 5 cm. The results of hematoxylin/eosin staining were suspicious for a tumor of vascular origin (Figure 4A). Immunohistochemically, the lesions were positive for CD34 (Figure 4B), and CD31 (Figure 4C), supporting the diagnosis of HEHE.
For patients with liver masses, correct preoperative diagnosis is necessary to guarantee an appropriate therapeutic approach. Given the rarity and unpredictable natural of HEHE, it is not possible to make an accurate diagnosis from heterogeneous clinical manifestations and nonspecific laboratory measurements. Most of these lesions also lack typical manifestations such as a “halo” sign and “capsular retraction” on imaging and present with nonspecific features. Thus, only histopathological results can guarantee an accurate diagnosis. In this study, the patient who had multiple hepatic nodules was examined using preoperative contrast-enhanced computerized tomography and contrast-enhanced ultrasonography, which indicated a diagnosis of metastatic carcinoma. PET-CT was then performed to detect the primary lesions. Surprisingly, no primary lesion was identified, and the hepatic lesions with low glycometabolism did not support the diagnosis of metastatic carcinoma. Thus, a tumor of vascular origin was then suspected and after clinical discussion, an extended right hemihepatectomy was carried out and the final histological results confirmed the diagnosis of HEHE.
HEHE has heterogeneous clinical features, nonspecific radiological characteristics and a variable natural history with a highly unpredictable clinical course. PET-CT may provide more information to help with the preoperative differential diagnosis; however, PET-CT is associated with high costs and sometimes only provides us with a reference and cannot guarantee an accurate diagnosis. One of the aims of the current study was to enhance awareness of the range of hepatobiliary surgery available in patients with multiple nodular lesions on imaging. In these patients, HEHE should at least be considered in the differential diagnosis. Multicenter studies based on the analysis of more practical and economic diagnostic tools are required to establish better regimens and subsequently guide the preoperative diagnosis of HEHE. Further studies focusing on the etiology of HEHE to improve preoperative diagnosis are also required.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Morales-Gonzalez J, Strom SC S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Campione S, Cozzolino I, Mainenti P, D’Alessandro V, Vetrani A, D’Armiento M. Hepatic epithelioid hemangioendothelioma: Pitfalls in the diagnosis on fine needle cytology and “small biopsy” and review of the literature. Pathol Res Pract. 2015;211:702-705. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562-582. [PubMed] [Cited in This Article: ] |
| 3. | Ishak KG, Sesterhenn IA, Goodman ZD, Rabin L, Stromeyer FW. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study of 32 cases. Hum Pathol. 1984;15:839-852. [PubMed] [Cited in This Article: ] |
| 4. | Mistry AM, Gorden DL, Busler JF, Coogan AC, Kelly BS. Diagnostic and therapeutic challenges in hepatic epithelioid hemangioendothelioma. J Gastrointest Cancer. 2012;43:521-525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Uchimura K, Nakamuta M, Osoegawa M, Takeaki S, Nishi H, Iwamoto H, Enjoji M, Nawata H. Hepatic epithelioid hemangioendothelioma. J Clin Gastroenterol. 2001;32:431-434. [PubMed] [Cited in This Article: ] |
| 6. | Hsieh MS, Liang PC, Kao YC, Shun CT. Hepatic epithelioid hemangioendothelioma in Taiwan: a clinicopathologic study of six cases in a single institution over a 15-year period. J Formos Med Assoc. 2010;109:219-227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Mosoia L, Mabrut JY, Adham M, Boillot O, Ducerf C, Partensky C, Baulieux J. Hepatic epithelioid hemangioendothelioma: long-term results of surgical management. J Surg Oncol. 2008;98:432-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Remiszewski P, Szczerba E, Kalinowski P, Gierej B, Dudek K, Grodzicki M, Kotulski M, Paluszkiewicz R, Patkowski W, Zieniewicz K. Epithelioid hemangioendothelioma of the liver as a rare indication for liver transplantation. World J Gastroenterol. 2014;20:11333-11339. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 35] [Cited by in F6Publishing: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Lakkis Z, Kim S, Delabrousse E, Jary M, Nguyen T, Mantion G, Heyd B, Lassabe C, Borg C. Metronomic cyclophosphamide: an alternative treatment for hepatic epithelioid hemangioendothelioma. J Hepatol. 2013;58:1254-1257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Wang LR, Zhou JM, Zhao YM, He HW, Chai ZT, Wang M, Ji Y, Chen Y, Liu C, Sun HC. Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg. 2012;36:2677-2683. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Thin LW, Wong DD, De Boer BW, Ferguson JM, Adams L, Macquillan G, Delriviere L, Mitchell A, Jeffrey GP. Hepatic epithelioid haemangioendothelioma: challenges in diagnosis and management. Intern Med J. 2010;40:710-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Woodall CE, Scoggins CR, Lewis AM, McMasters KM, Martin RC. Hepatic malignant epithelioid hemangioendothelioma: a case report and review of the literature. Am Surg. 2008;74:64-68. [PubMed] [Cited in This Article: ] |
| 13. | Deng Y, Zhou Y, Cheng N. Laparoscopic liver biopsy in the diagnosis of hepatic epithelioid hemangioendothelioma: A case report. Oncol Lett. 2014;8:1317-1319. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Ben-Haim M, Roayaie S, Ye MQ, Thung SN, Emre S, Fishbein TA, Sheiner PM, Miller CM, Schwartz ME. Hepatic epithelioid hemangioendothelioma: Resection or transplantation, which and when? Liver Transp Surg. 1999;5:526-531. [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 81] [Article Influence: 3.2] [Reference Citation Analysis (0)] |