Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 28, 2016; 22(4): 1433-1448
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1433
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1433
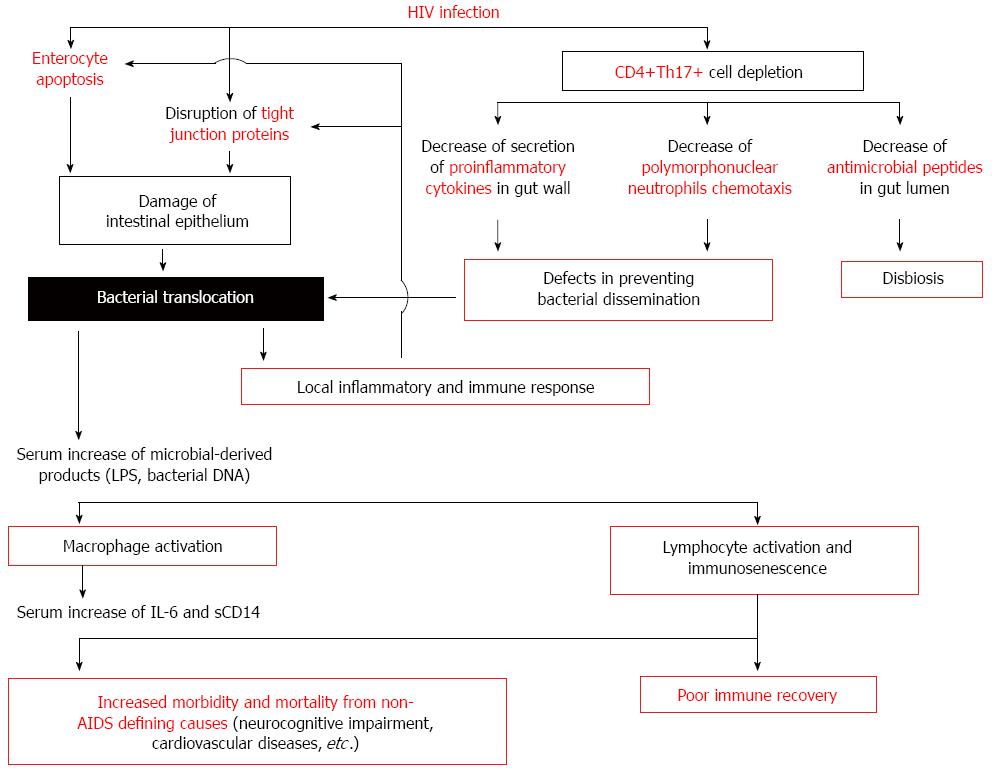
Figure 1 Effect of bacterial translocation on innate and acquired immune activation in human immunodeficiency virus-infected patients.
In the gastrointestinal tract, human immunodeficiency virus (HIV) infection induces a Th17 CD4+ T helper cells depletion and a damage of intestinal epithelium as a consequence of the HIV exposure itself or by immune-induced enterocyte damage. The consequence of the alteration in gut barrier is the bacterial translocation. Increased plasma concentrations of several markers indicative of pathological bacterial translocation [lipopolysaccharide (LPS), bacterial DNA] have been detected in these patients. These molecules induce a monocyte and lymphocyte activation implicated in the increased morbidity and mortality from non-acquired immunodeficiency syndrome (AIDS) defining causes (neurocognitive impairment, cardiovascular diseases, etc.) and in the poor immune recovery. IL: Interleukin; sCD14: Soluble CD14.
- Citation: Márquez M, Fernández Gutiérrez del Álamo C, Girón-González JA. Gut epithelial barrier dysfunction in human immunodeficiency virus-hepatitis C virus coinfected patients: Influence on innate and acquired immunity. World J Gastroenterol 2016; 22(4): 1433-1448
- URL: https://www.wjgnet.com/1007-9327/full/v22/i4/1433.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i4.1433