Copyright
©The Author(s) 2016.
World J Gastroenterol. May 21, 2016; 22(19): 4673-4684
Published online May 21, 2016. doi: 10.3748/wjg.v22.i19.4673
Published online May 21, 2016. doi: 10.3748/wjg.v22.i19.4673
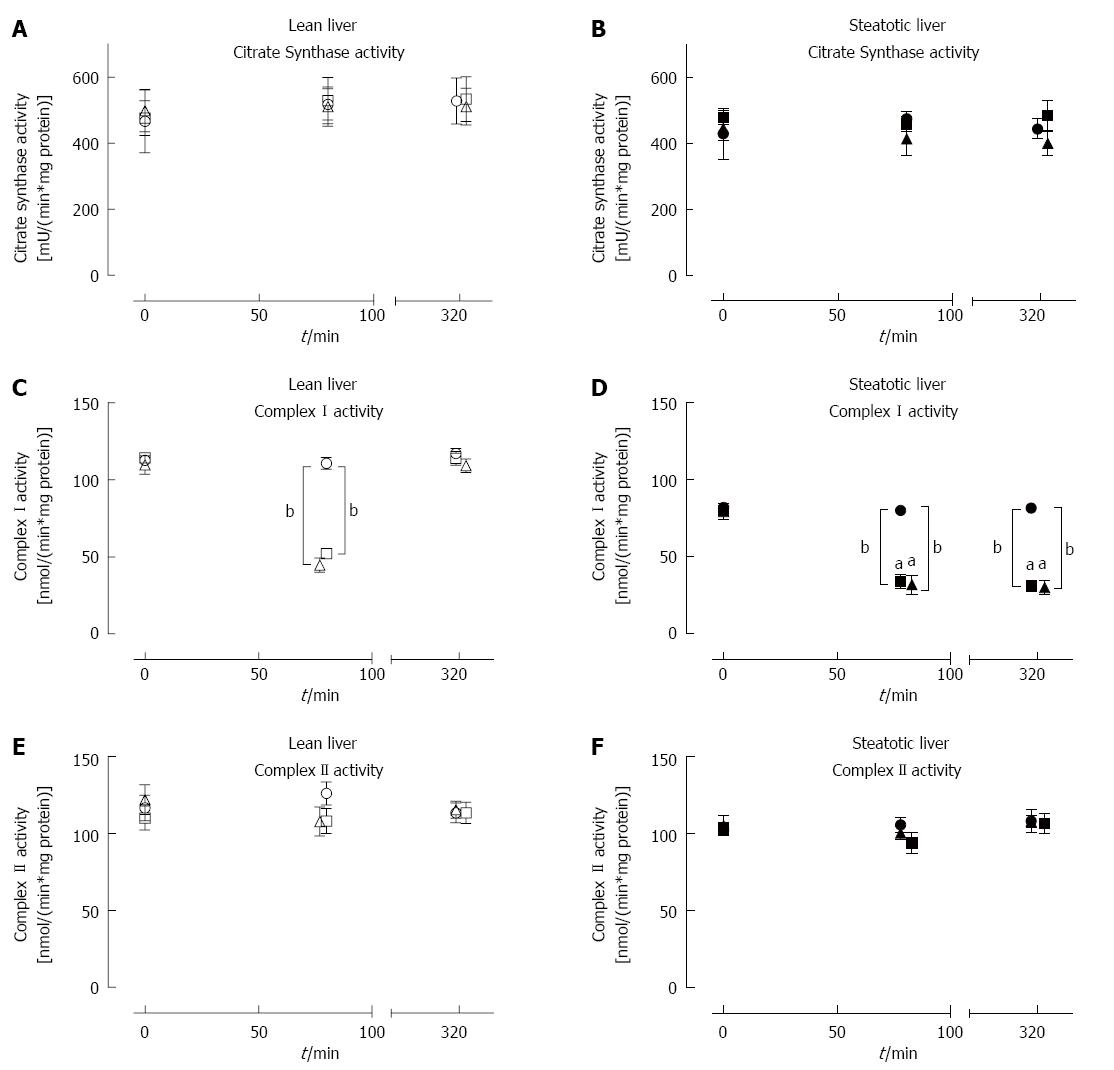
Figure 5 Citrate synthase, Complex I and Complex II activity at baseline, following ischemia and post-reperfusion in lean and steatotic livers.
CS activity was similar between lean (A) and steatotic livers (B) throughout the procedure and was not affected by IRI or IPC. Baseline CI enzyme activity in steatotic livers were lower than lean livers (C, D). After ischemia, CI enzyme activity was significantly lower in lean and steatotic livers compared to sham livers. Additionally, CI enzyme activity (D) was lower in steatotic livers post-ischemia compared to lean livers. After reperfusion, CI activity remained lower in Steatotic-IRI and Steatotic-IPC livers (D) compared to Steatotic-Sham or lean livers. CII activity (E, F) remained stable throughout the procedure and was similar between both types of livers. IPC did not have a significant effect on CI or CII activity in both types of livers. Data are expressed as mean ± SE (n = 10 rat/group; Lean-Sham, open circle; Lean-IRI, open square; Lean-IPC, open triangle; Steatotic-Sham, closed circle; Steatotic-IRI, closed square; Steatotic-IPC, closed triangle). aP < 0.05, bP < 0.001 vs time- and group-matched lean livers. CS: Citrate synthase; CI: Complex I; CII: Complex II; IRI: Ischemia-reperfusion injury; IPC: Ischemic preconditioning.
- Citation: Chu MJ, Premkumar R, Hickey AJ, Jiang Y, Delahunt B, Phillips AR, Bartlett AS. Steatotic livers are susceptible to normothermic ischemia-reperfusion injury from mitochondrial Complex-I dysfunction. World J Gastroenterol 2016; 22(19): 4673-4684
- URL: https://www.wjgnet.com/1007-9327/full/v22/i19/4673.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i19.4673