Published online Mar 21, 2016. doi: 10.3748/wjg.v22.i11.3212
Peer-review started: October 15, 2015
First decision: November 13, 2015
Revised: November 27, 2015
Accepted: December 30, 2015
Article in press: December 30, 2015
Published online: March 21, 2016
Processing time: 150 Days and 20.8 Hours
AIM: To determine the correlation between the hepatic venous pressure gradient and the endoscopic grade of esophageal varices.
METHODS: From September 2009 to March 2013, a total of 176 measurements of hepatic venous pressure gradient (HVPG) were done in 146 patients. Each transjugular HVPG was measured twice, first using an end whole catheter (EH-HVPG), and then using a balloon catheter (B-HVPG). The HVPG was compared with the endoscopic grade of esophageal varices (according to the general rules for recording endoscopic findings of esophagogastric varices), which was recorded within a month of the measurement of HVPG.
RESULTS: The study included 110 men and 36 women, with a mean age of 56.1 years (range, 43-76 years). The technical success rate of the pressure measurements was 100% and there were no complication related to the procedures. Mean HVPG was 15.3 mmHg as measured using the end hole catheter method and 16.5 mmHg as measured using the balloon catheter method. Mean HVPG (both EH-HVPG and B-HVPG) was not significantly different among patients with different characteristics, including sex and comorbid factors, except for cases with hepatocellular carcinoma (B-HVPG, P = 0.01; EH-HVPG, P = 0.02). Portal hypertension (> 12 mmHg HVPG) occurred in 66% of patients according to EH-HVPG and 83% of patients according to B-HVGP, and significantly correlated with Child’s status (B-HVPG, P < 0.000; EH-HVGP, P < 0.000) and esophageal varies observed upon endoscopy (EH-HVGP, P = 0.003; B-HVGP, P = 0.006). One hundred and thirty-five endoscopies were performed, of which 15 showed normal findings, 27 showed grade 1 endoscopic esophageal varices, 49 showed grade 2 varices, and 44 showed grade 3 varices. When comparing endoscopic esophageal variceal grades and HVPG using univariate analysis, the P value was 0.004 for EH-HVPG and 0.002 for B-HVPG.
CONCLUSION: Both EH-HVPG and B-HVPG showed a positive correlation with the endoscopic grade of esophageal varices, with B-HVPG showing a stronger correlation than EH-HVPG.
Core tip: This retrospective study aimed to determine the correlation between the hepatic venous pressure gradient (HVPG) and the endoscopic grade of esophageal varices. Our results showed a good correlation between the endoscopic grade of esophageal varices and the HVPG measured by using either end-hole catheter or balloon catheter techniques. HVPG measured with the balloon catheter method showed a stronger correlation with esophageal varix grade upon endoscopy than when measured with the end-hole catheter method. HVPG measured using the balloon catheter method provides useful information that will allow practitioners to predict the risk of esophageal varix bleeding and guide patients towards appropriate treatment.
- Citation: Lee E, Kim YJ, Goo DE, Yang SB, Kim HJ, Jang JY, Jeong SW. Comparison of hepatic venous pressure gradient and endoscopic grading of esophageal varices. World J Gastroenterol 2016; 22(11): 3212-3219
- URL: https://www.wjgnet.com/1007-9327/full/v22/i11/3212.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i11.3212
It is well known that the hepatic venous pressure gradient (HVPG) correlates well with the clinical severity and prognosis of the symptoms of liver cirrhosis, including esophageal variceal bleeding[1]. Thus, HVPG has been used as a prognostic predictor of cirrhosis severity and in pharmacological prevention of variceal bleeding. Commonly used methods for measuring HPVG are end-hole and balloon catheter techniques. It has been reported that the balloon catheter is more accurate and reproducible[2,3]. However, whether differences in pressure measurements obtained from the end-hole and balloon catheter techniques are clinically relevant remains unclear.
Esophageal varices are common complication of liver cirrhosis, and variceal bleeding is closely related to the mortality and morbidity of these patients. The reported mortality from acute bleeding episodes accounts for approximately 15%-20% in liver cirrhosis patients[4]. In addition, the endoscopic grade of esophageal varices closely correlates with variceal bleeding[5]. In a recent literature review, we found few reports on the relationship between HVPG measurement methods and esophageal varices grade based on endoscopic findings. The purpose of the present study, therefore, is to determine the correlation between the hepatic venous pressure gradient and the endoscopic grade of esophageal varices, while also comparing the pressures obtained with the use of end-hole and balloon catheter techniques.
From September 2009 to March 2013, a total of 176 HVPG measurements were carried out in 146 liver cirrhosis patients in the interventional radiology unit at our institution. This study was reviewed and approved by the Institutional Review Board on Human Subjects Research and Ethics Committees of Soonchunhyang University Seoul Hospital. The HVPG measurements were done before any medical treatment or during transjugular intrahepatic portosystemic shunt (TIPS) or balloon-occluded retrograde transvenous obliteration. Inclusion criteria for the study were: diagnosis of cirrhosis (based on clinical, serological and imaging findings including abdominal computed tomography and/or ultrasound); stable hemodynamic state with no active variceal bleeding at the time of HVPG measurement; no large ascites that might affect intra-abdominal pressure and patients with endoscopic exams within a month (before or after) the HVPG measurements. The study included 110 male and 36 female patients with a mean age of 56.1 years (range, 43-76 years). The etiologies of liver cirrhosis were alcoholism (n = 76, 52%), hepatitis B (n = 57, 39%), hepatitis C (n = 8, 5.5%), and other (n = 5, 3.5%) including cryptogenic and autoimmune hepatitis. Forty-six patients had a Child-Pugh status of A (31.5%), 81 patients had a status of B (55.5%), and 19 patients had a status of C (13%). Comorbid factors were documented based on a review of patients’ medical records.
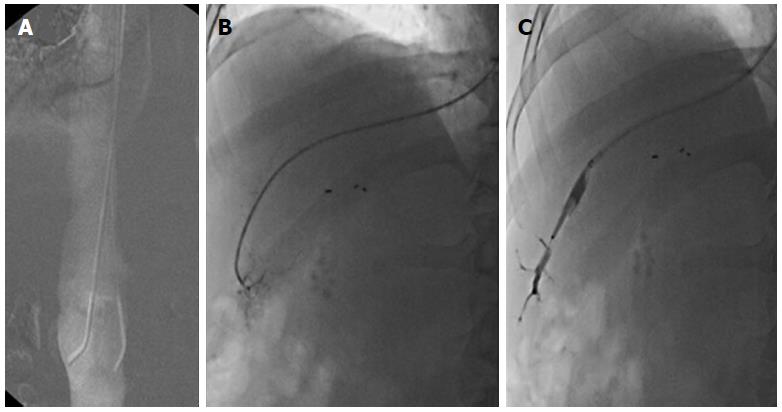
Two attending interventional radiologists, with 10 and 20 years of experience, performed the procedures after receiving information on the patients’ diagnoses and clinical statuses. All measurements were performed in fasting patients in the supine position, and no intravenous or oral medication known to affect portal vein pressure had been administered for at least 24 h before the procedures. The right internal jugular vein approach was used in all cases with a 7-F introducer sheath (Teleflex, Westmeath, Ireland). Systemic venous pressure [measured in the infrarenal inferior vena cava (IVC)] was taken with a 5-F end-hole vascular catheter (KMP, AA M.M., Gyunggido, South Korea) and wedged hepatic venous pressure (WHVP) was measured in the right hepatic vein with a 5-F, 7mm balloon catheter (Clearstream technologies, Wexford, Ireland). Contrast material (Iomeron® 300, Braco) was used for IVC and wedged hepatic venograms. Systemic venous pressure was assessed by the placement of a catheter in the IVC at the level of the renal vein. For measurements of WHVP, the end-hole catheter was advanced until the technician felt resistance or a slight bowing in the catheter shaft was seen on fluoroscopy. The balloon catheter was inflated until likewise achieving a wedged position. All procedures associated with placement of catheters were carried out under fluoroscopic guidance (Figure 1). Adequate occlusion of the hepatic vein was confirmed by the absence of backflow following dye injection. Prior to recording of the tracings, both systemic venous pressure and wedge hepatic venous pressure were allowed to stabilize for at least 45-60 s. In this study, the hepatic venous pressure gradient was determined by subtracting the IVC pressure from the wedged hepatic venous pressure. Portal hypertension is defined as an HVPG over 12 mmHg.
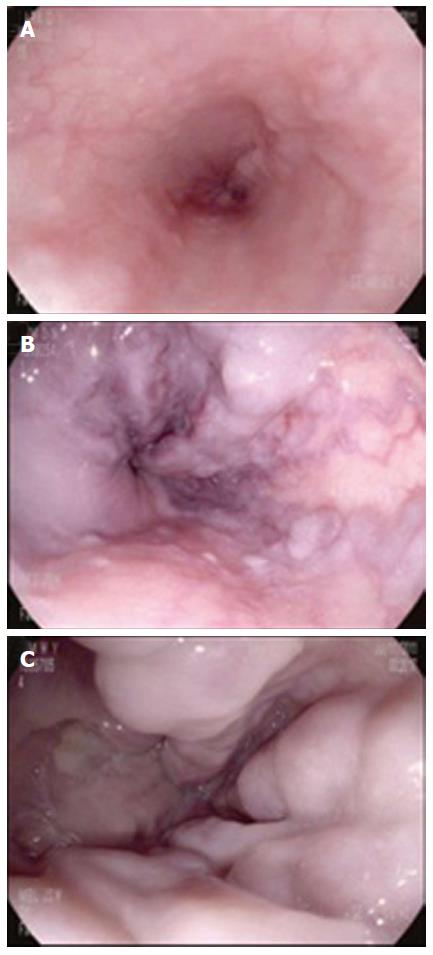
Endoscopic exams were carried out in 135 cases in 146 patients within a month (before or after) the HVPG measurements. Two board-certificated gastroenterologists with 2 and 10 years of experience performed the endoscopic procedures after receiving information on the patients’ diagnoses and clinical statuses. Endoscopic grading of esophageal varices is based on “The General rules for recording endoscopic findings of esophageal varices,” published by the Japanese Research Society for Portal Hypertension. Esophageal varix form was classified as follows: F1, small straight varix; F2, enlarged tortuous varix that occupies less than one-third of the lumen; F3, large coil-shaped varix that occupies more than one-third of the lumen (Figure 2). The two gastroenterologists separately reviewed the endoscopic exam findings and came to a consensus on the final grade for each patient.
The Mann-Whitney U test and the Kruskal-Wallis test were used to identify differences in HVPG (both EH-HVPG and B-HVPG) among the patients with different characteristics, including sex, etiology of liver cirrhosis, and comorbid factors. To examine the correlation between hemodynamic status and HVPG values, a Spearmann correlation was used. A χ2 test was used to identify the possible confounder effect of severity of liver cirrhosis. To evaluate the association between the severity of liver cirrhosis (Child-Pugh status) and the HVPG, a χ2 test and univariate ANOVA with Turkey’s B were used. Fisher’s exact test was used to evaluate the correlation between the HVPG measurement taken with each method (end-hole and balloon catheter) and the presence of an esophageal varix on the endoscopic exam. The Spearman correlation was used to evaluate the correlation between the two HVPG measurement methods and the endoscopic grade of esophageal varices. Statistical analysis was carried out using the SPSS 14.0 software package (SPSS Inc., Chicago, IL), and statistical significance was defined as P < 0.05.
Measurement of HVPG in was carried out with both end-hole and balloon catheter methods in each patient. The technical success rate was 100% in all cases and there were no procedure-related complications. The mean pressures were 15.7 mmHg in the IVC (at the renal vein level) and 30.9 mmHg in the WHVP as measured with the end-hole catheter method, and 32.1 mmHg in WHVP as measured with the balloon catheter method. The mean HVPG was 15.3 mmHg with the end hole catheter method and 16.5 mmHg with the balloon catheter method. Portal hypertension (HVPG > 12 mmHg) was identified in 66% of the patients using EH-HVPG and in 83% of the patients using B-HVPG.
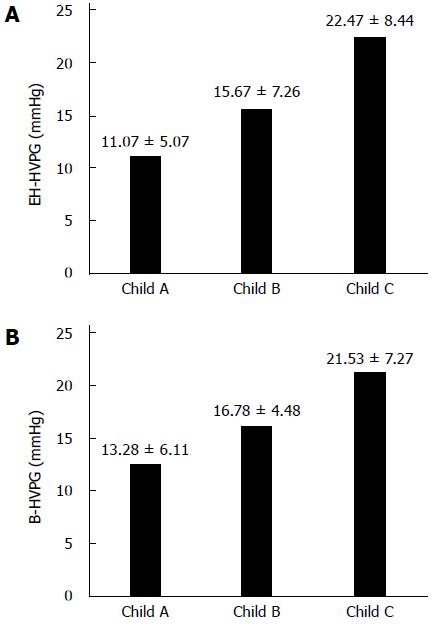
The baseline Child-Pugh status was recorded in all patients. The analysis of the correlation between HVPG and the severity of liver cirrhosis was carried out using a χ2 test. A Child-Pugh status of C reflects the most severe liver cirrhosis. 20/46 patients (43%) with Child’s A, 58/81 patients (71%) with Child’s B and 17/19 patients (89%) with Child’s C showed portal hypertension using the end-hole catheter method. With the balloon catheter method, 29/46 patients (63%) with Child’s A, 73/81 patients (90%) with Child’s B and 18/19 patients (94%) with Child’s C showed portal hypertension. A significantly higher proportion of patients with Child’s B and C status showed portal hypertension using both methods (P < 0.000) (Tables 1 and 2). In both methods, HVPG increases as the Child-Pugh score increases. When using the end-hole catheter method, the mean HVPG in patients with Child’s A was 11.07 ± 5.07 mmHg, in patients with Child’s B it was 15.67 ± 7.26 mmHg, and in those with Child’s C it was 22.47 ± 8.44 mmHg. Using the balloon catheter method, the mean HVPG in patients with Child’s A was 13.28 ± 6.11 mmHg, in those with Child’s B it was 16.78 ± 4.48 mmHg, and in those with Child’s C it was 21.53 ± 7.27 mmHg. Univariate ANOVA analysis showed that the mean HVPG increases as the Child’s status increases, and the mean HVPG value of each status is significantly different regardless of which measurement method was used (P < 0.000) (Figure 3). Post-hoc analysis (Tukey’s B test) showed that the mean HVPG values among the Child status groups were significantly different.
| Normal | Portal HTN | Total | |
| Child A | 26 | 20 | 46 |
| Child B | 23 | 58 | 81 |
| Child C | 2 | 17 | 19 |
| Total | 51 | 95 | 146 |
| Normal | Portal HTN | Total | |
| Child A | 17 | 29 | 46 |
| Child B | 8 | 73 | 81 |
| Child C | 1 | 18 | 19 |
| Total | 26 | 120 | 146 |
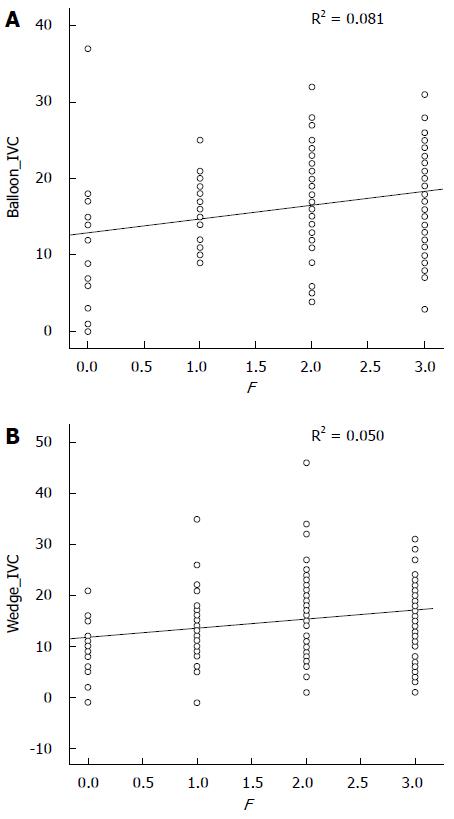
Endoscopy was carried out in 135 cases in 146 patients. Normal findings were seen in 15 cases (11%). The endoscopic grade of esophageal varix, based on the “General rules for recording endoscopic findings of esophageal varices,” was F1 in 27 cases (20%), F2 in 49 cases (36%), and F3 in 44 cases (33%). Of the 135 cases, 93 (69%) showed moderate to large varices. 83/87 patients (95%) with portal hypertension showed an esophageal varix upon endoscopic examination using the end-hole catheter method (P = 0.003), and 103/111 patients (92%) with portal hypertension showed an esophageal varix upon endoscopic examination using the balloon catheter method (P = 0.006). Although esophageal varices were found in both the normal and portal hypertension groups, the incidence was significantly higher in the portal hypertension group using either method (P = 0.003, end-hole catheter; P = 0.006, balloon catheter). Univariate ANOVA analysis showed that both EH-HVPG and B-HVPG were positively correlated with the endoscopic grading of esophageal varices. B-HVPG (r = 0.081, P = 0.002) showed a stronger positive relationship with the endoscopic grading of esophageal varices than did EH-HVPG (r = 0.050, P = 0.004) (Figure 4).
Hemodynamic factors including systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) that might affect HVPG had no significant correlation with HVPG when using the end-hole catheter method (SBP, P = 0.38; DBP, P = 0.36; HR, P = 0.56) or the balloon catheter method (SBP, P = 0.66; DBP, P = 0.25; HR, P = 0.14).
In this study, the number of male patients was about 3 times greater than the number of female patients (M:F = 110:35). However, there was no significant difference seen with EH-HVPG (P = 0.40) or B-HVPG (P = 0.32) depending on sex.
The etiologies of liver cirrhosis were alcoholism (n = 76, 52%), hepatitis B (n = 57, 39%), hepatitis C (n = 8, 5.5%), and other (n = 5, 3.5%) including cryptogenic and autoimmune hepatitis. As there were a small number of hepatitis C patients, we evaluated etiologies in three groups: viral (hepatitis B and C), alcoholism, and other. There was no significant difference seen with EH-HVPG (P = 0.10) or B-HVPG (P = 0.10) among the groups.
Percent of forty-eight (71/146) of patients had one or more comorbid factor. The comorbid factors were hypertension (n = 14), diabetes mellitus (n = 29), hepatocellular carcinoma (n = 41), gastric cancer (n = 2), chronic renal failure with no hemodialysis (n = 1), Moyamoya disease (n = 1), systemic lupus erythematosus (n = 1), and thyroid cancer (n = 1). Thirty-two percent (23/71) of patients had more than one comorbid factor. When we compared HVPG between the comorbid group and the non-comorbid group, we found no significant difference whether EH-HVPG (P =0.22) or B-HVPG (P = 0.07) was used. However, there was a significant difference in HVPG between the group with hepatocellular carcinoma (HCC) and the group with no HCC (EH-HVPG, P = 0.02; B-HVPG, P = 0.01). The mean HVPG value was lower in the HCC group (EH-HVPG, 12.3 mmHg; B-HVPG, 14.4 mmHg) than in the non-HCC group (EH-HVPG, 16.0 mmHg; B-HVPG, 16.9 mmHg). However, it should be noted that the non-HCC group had a significantly larger number of patients with Child-Pugh class B and C status (P = 0.002).
In this study, HVPG measured with both the end-hole and balloon catheter methods showed a good correlation with Child-Pugh status, representing the severity of liver cirrhosis, and the presence of high-grade esophageal varices. B-HVPG showed a stronger positive relationship with the endoscopic grading of esophageal varices than did EH-HVPG.
One strength of this study is that it included data from a relatively large number of patients. Also, as the WHVP measurements were done with two different methods (end-hole and balloon catheter), the rate of intra-patient measurement error is probably low. Moreover, this study compared two different HVPG measurement methods and showed that the balloon catheter method had a better correlation with esophageal varix grade.
As the grading of esophageal varices is based on visual inspection upon endoscopy, the evaluation of the severity of esophageal varices is relatively subjective, and not quantitative. We confirmed the relationship between the esophageal varix grade based upon endoscopic findings and the semi-quantitative data based on hepatic pressure gradient, which provides support for the use of endoscopy in estimating variceal bleeding risk. Silkauskaite et al[6] demonstrated a positive relationship between HVPG and the size of esophageal varices. As all bleeders had large varices and non-bleeders had both small and large varices, those researchers analyzed large varices separately to eliminate confounding variables. The analysis of large varices alone shows that HVPG is significantly higher in bleeders compared to non-bleeders. Kim et al[7] also showed that the variceal bleeding risk significantly increases as HVPG increases. In addition, patients with high-grade endoscopic esophageal varices had a higher bleeding risk, and the esophageal varix grade tended to increase as HVPG increased, even though those results were not statistically significant. Wadhawan et al[8] reported similar results. A possible explanation for the variable results seen with respect to the relationship between variceal size and HVPG is that various portosystemic shunts used to treat portal hypertension may have resulted in the partial displacement of HVPG into the esophageal varices[9].
Direct methods used to measure portal pressure, such as splenic pulp puncture and percutaneous transhepatic approaches, are invasive and involve complications such as hemorrhage, portal vein thrombosis, or intrahepatic arteriovenous fistula, especially in liver cirrhosis patients with a high risk of bleeding and ascites. Thus, measuring HPVP indirectly by assessing wedged hepatic venous pressure is a good alternative[1]. Currently, the preferred method for determining portal pressure is hepatic vein catheterization, which measures a different pressure than that of the hepatic vein and inferior vena cava (IVC). In this study, we used the pressure measured in the infrarenal inferior vena cava as the systemic venous pressure. Usually, systemic venous pressure is measured in the free hepatic vein (free hepatic venous pressure, FHVP) by maintaining the tip of the catheter free in the hepatic vein, at 2-4 cm from its opening into the inferior vena cava. FHVP is usually close to the IVC pressure, with a difference of less than 2 mmHg. However, there are situations in which the difference is greater than 2 mmHg, such as partial or complete wedging of the catheter, inadequate placement of the catheter, or hepatic vein occlusion. In addition, systemic venous pressure measurement in the hepatic vein and IVC junction can be affected by respiratory motion. Thus, we used the IVC pressure measured at the infrarenal level as the systemic venous pressure in order to eliminate variability in pressure measurement. Wedged hepatic venous pressure is measured by occluding the hepatic vein, either by wedging an end-hole catheter into a small branch of the hepatic vein or by inflating a balloon at the tip of a catheter in a distal branch of the hepatic vein. Previous studies have shown that HVPG measurement using the balloon catheter method is more consistent and reproducible than measurement using an end-hole or non-balloon catheter[2,3,10]. Also, the values measured with the end-hole catheter method tend to vary when the catheter is wedged in different hepatic veins because of the heterogeneity of sinusoidal involvement of liver cirrhosis[11]. On the other hand, the balloon catheter method allows measurement of the hepatic veins at the lobar and sublobar levels and, thus, more consistently represents the true portal venous pressure[12]. The current study also demonstrates that HVPG measurement using a balloon catheter correlates better with the endoscopic grade of esophageal varices (P = 0.002 for the balloon catheter method and P = 0.004 for the end-hole catheter method), which supports the use of the balloon catheter method in HVPG measurement.
We evaluated differences in HVPG according to patient characteristics. There was no significant correlation between HVPG and hemodynamic factors including systemic blood pressure and heart rate. In this study, the number of male patients was about 3 times greater than the number of female patients (M:F = 110:35), which may have resulted in a selection bias. However, there was no significant difference seen using EH-HVPG (P = 0.40) or B-HVPG (P = 0.32) between male and female patients. Also, there was no significant difference seen using EH-HVPG (P = 0.10) or B-HVPG (P = 0.10) depending on the etiology of liver cirrhosis. Forty-eight percent (71/146) of patients had one or more comorbid factor, and there was no significant difference in HVPG between the comorbid group and the non-comorbid group. However, patients with HCC at the time of HVPG measurement had significantly different HVPG measurements than did those without HCC. In a secondary analysis of a randomized, controlled trial in patients with compensated cirrhosis, Ripoll et al[13] reported that HVPG is an independent factor for HCC, in addition to albumin levels and viral etiology. Also, in patients with well-compensated cirrhosis and resectable HCC, the presence of clinically significant portal hypertension markedly increased the risk of unresolved hepatic decompensation occurring within 3 mo of hepatic resection[14]. Our study showed the opposite result, that the HCC group showed significantly lower mean HVPG values, regardless of measurement method. The probable explanation for this result is that the non-HCC group included a significantly larger number of Child-Pugh class B and C patients (P = 0.002) and the severity of underlying liver cirrhosis is a confounding factor. Also, as the number of patients known to have HCC was relatively small, it is difficult to generalize from our results.
This present study has several limitations. First, this is a retrospective study that used records from a single medical center; thus, further studies using larger sample sizes and prospective studies are necessary for verification of our results. Second, HVPG measurement and endoscopic grading of esophageal varices were not performed blindly. As both HVPG measurement and endoscopy are invasive procedures, the subjects were limited to patients with cirrhosis of the liver. Also, regarding the assignment of endoscopic variceal grades, two gastroenterologists separately reviewed and determined the final grades in consensus. Third, as direct portal pressure was not measured, the extent to which the balloon or end-hole techniques reflected true portal pressure is not clear. However, this problem is offset to some degree by the relatively close correlation of the pressure values obtained by both methods, and also by the positive correlation with variceal size, which is known to be closely correlated with portal pressure. Further studies comparing pressure measured via direct portal vein puncture to that measured with balloon and end-hole catheters will be helpful in supporting our results. Forth, IVC pressure and wedged hepatic venous pressure were measured only once per patient in a branch of the right hepatic vein, which may affect the reliability of the measurements. Nevertheless, we traced pressures for at least 45-60 s in order to stabilize the measurements and attempted to minimize variability in pressure measurement. Fifth, we did not analyze data based on bleeding events or attempt to compare long-term follow up results with prognosis. It is known that a higher HVPG and a larger variceal size are related to higher risk of initial bleeding and a higher risk of repeat bleeding after pharmacological treatment. Thus, further studies are needed, including long-term follow up and comparison of variceal bleeding events with prognosis.
Both EH-HVPG and B-HVPG show a positive correlation with the endoscopic grade of esophageal varices, with B-HVPG showing a stronger correlation than EH-HVPG. Thus, the use of balloon catheters for HVPG measurement may provide more useful information when practitioners attempt to predict the risk of esophageal variceal bleeding and choose appropriate treatment.
Portal vein pressure closely correlates with the severity of liver cirrhosis and complications including esophageal varices, and is used as a prognostic predictor in liver cirrhosis. It is known that the hepatic vein pressure gradient (HVPG) adequately reflects portal pressure in liver cirrhosis patients, especially those with HBV and HCV-related cirrhosis. HVPG values greater than 10 mmHg are regarded as clinically significant value; they are associated with portal hypertensive syndrome. HVPG is usually measured either with an end-hole catheter or a balloon catheter. In this study, we evaluated the correlation between the hepatic venous pressure gradient and the endoscopic grade of esophageal varices, while simultaneously comparing the pressures obtained with the use of end-hole and balloon catheters.
It is important to measure HVPG with reliable and appropriate methods for proper management of liver cirrhosis. Few studies have been done on the relationship between esophageal varix grading based on endoscopic findings and HVPG measured with end-hole and balloon catheters.
In this study, HVPG measured with both the end-hole and the balloon catheter methods showed a good correlation with Child-Pugh status, representing the severity of liver cirrhosis, and the presence of high-grade esophageal varices on endoscopic exams. HVPG measured with the balloon catheter method showed a stronger positive relationship with the endoscopic grading of esophageal varices than did HVPG measured with the end-hole catheter method.
HVPG measured with the balloon catheter method showed a stronger positive relationship with the endoscopic grading of esophageal varices than did EH-HVPG. This result supports the use of the balloon catheter method in HVPG measurement.
FHVP: Free hepatic venous pressure is pressure of a non-occluded hepatic vein and should be similar to pressure in the inferior vena cava (systemic venous pressure). In this study, it was measured at the level of the infrarenal inferior vena cava. WHVP: The wedged hepatic venous pressure reflects portal venous pressure at the sinusoidal level. Two methods can be used for WHVP measurement, the balloon catheter method and the end-hole catheter method. HVPG: Hepatic venous pressure gradient is determined by subtracting the IVC pressure from the WHVP. It is known that HVPG adequately reflects portal pressure in liver cirrhosis patients. EH-HVPG: HVPG measured by the end-hole catheter method. B-HVPG: HVPG measured by the balloon catheter method.
The authors of this study evaluated the correlation between the hepatic venous pressure gradient using two different methods (end-hole and balloon catheters) and the endoscopic grade of esophageal varices. The results showed that both methods showed a good correlation with endoscopic grade of esophageal varices, but measurements taken with the balloon catheter method showed a stronger positive correlation. Further studies with a larger number of subjects and evaluation of prognosis will be valuable. Also, further studies comparing HVPG measurements using direct methods such as portal vein puncture and indirect methods such as balloon and end-hole catheters will be helpful in strengthening this results.
P- Reviewer: Aytac E, Cao GW, Cuadrado-Garcia A S- Editor: Qi Y L- Editor: A E- Editor: Ma S
| 1. | Bosch J, Abraldes JG, Berzigotti A, García-Pagan JC. The clinical use of HVPG measurements in chronic liver disease. Nat Rev Gastroenterol Hepatol. 2009;6:573-582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 451] [Cited by in F6Publishing: 482] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 2. | Smith TP, Kim CY, Smith AD, Janas G, Miller MJ, Sopko DR, Suhocki PV. Hepatic venous pressure measurements: comparison of end-hole and balloon catheter methods. J Vasc Interv Radiol. 2012;23:219-26.e6. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Zipprich A, Winkler M, Seufferlein T, Dollinger MM. Comparison of balloon vs. straight catheter for the measurement of portal hypertension. Aliment Pharmacol Ther. 2010;32:1351-1356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | D'Amico G, Garcia-Pagan JC, Luca A, Bosch J. Hepatic vein pressure gradient reduction and prevention of variceal bleeding in cirrhosis: a systematic review. Gastroenterology. 2006;131:1611-1624. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 367] [Cited by in F6Publishing: 326] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 5. | Tajiri T, Yoshida H, Obara K, Onji M, Kage M, Kitano S, Kokudo N, Kokubu S, Sakaida I, Sata M. General rules for recording endoscopic findings of esophagogastric varices (2nd edition). Dig Endosc. 2010;22:1-9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 197] [Cited by in F6Publishing: 227] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 6. | Silkauskaite V, Pranculis A, Mitraite D, Jonaitis L, Petrenkiene V, Kupcinskas L. Hepatic venous pressure gradient measurement in patients with liver cirrhosis: a correlation with disease severity and variceal bleeding. Medicina (Kaunas). 2009;45:8-13. [PubMed] [Cited in This Article: ] |
| 7. | Kim MY, Baik SK, Suk KT, Yea CJ, Lee IY, Kim JW, Cha SH, Kim YJ, Um SH, Han KH. [Measurement of hepatic venous pressure gradient in liver cirrhosis: relationship with the status of cirrhosis, varices, and ascites in Korea]. Korean J Hepatol. 2008;14:150-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Wadhawan M, Dubey S, Sharma BC, Sarin SK, Sarin SK. Hepatic venous pressure gradient in cirrhosis: correlation with the size of varices, bleeding, ascites, and child’s status. Dig Dis Sci. 2006;51:2264-2269. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Lebrec D, De Fleury P, Rueff B, Nahum H, Benhamou JP. Portal hypertension, size of esophageal varices, and risk of gastrointestinal bleeding in alcoholic cirrhosis. Gastroenterology. 1980;79:1139-1144. [PubMed] [Cited in This Article: ] |
| 10. | Maleux G, Willems E, Fieuws S, Heye S, Vaninbroukx J, Laleman W, Cassiman D, Verslype C, Nevens F. Prospective study comparing different indirect methods to measure portal pressure. J Vasc Interv Radiol. 2011;22:1553-1558. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Keiding S, Vilstrup H. Intrahepatic heterogeneity of hepatic venous pressure gradient in human cirrhosis. Scand J Gastroenterol. 2002;37:960-964. [PubMed] [Cited in This Article: ] |
| 12. | Groszmann RJ, Wongcharatrawee S. The hepatic venous pressure gradient: anything worth doing should be done right. Hepatology. 2004;39:280-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 406] [Cited by in F6Publishing: 363] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 13. | Ripoll C, Groszmann RJ, Garcia-Tsao G, Bosch J, Grace N, Burroughs A, Planas R, Escorsell A, Garcia-Pagan JC, Makuch R. Hepatic venous pressure gradient predicts development of hepatocellular carcinoma independently of severity of cirrhosis. J Hepatol. 2009;50:923-928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 284] [Cited by in F6Publishing: 275] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 14. | Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology. 1999;30:1434-1440. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1331] [Cited by in F6Publishing: 1393] [Article Influence: 55.7] [Reference Citation Analysis (0)] |