Copyright
©The Author(s) 2015.
World J Gastroenterol. Nov 7, 2015; 21(41): 11502-11521
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11502
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11502
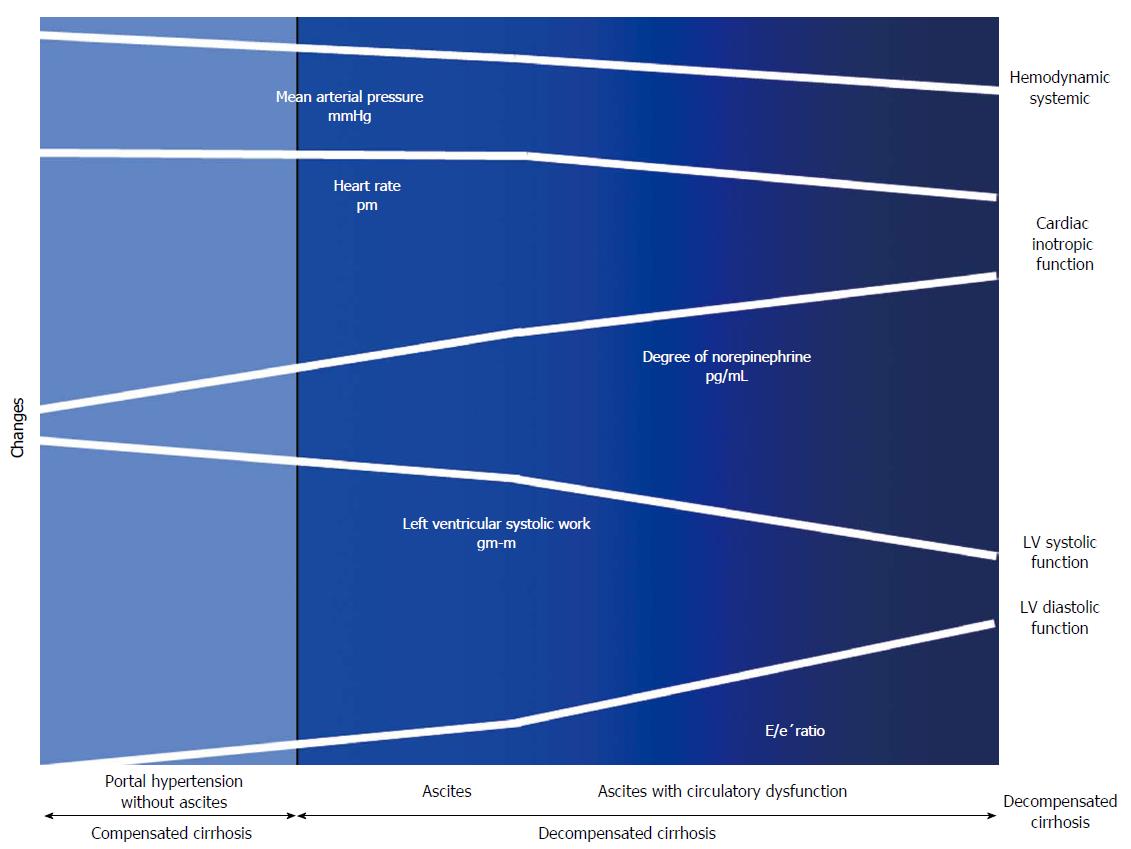
Figure 4 Cardiac and circulatory dysfunction according to presence of compensated and decompensated cirrhosis.
There is a progressive splanchnic arterial vasodilatation due to the overproduction of vasodilator molecules. Initially, circulatory homeostasis is maintained by the development of a hyperdynamic circulation. Later during the course of decompensated cirrhosis, patients develop an activation of the vasoconstrictor systems to maintain arterial pressure. In subsequent stages, the progressive decrease in cardiac afterload is not followed by an increase in HR and CO due to a decrease in cardiac function. Finally, in the advanced phase, when impairment of effective arterial blood volume is extreme, patients showed increased activity of NE concentration, arterial hypotension and reduced LVSF (CO and LV stroke work), and cardiac chronotropic function, and a higher degree in LVDD (E/e’) as compared to those with ascites, but normal NE, or without ascites. E/e’ratio: Peak E-wave transmitral/Peak early diastolic mitral annular velocity.
- Citation: Ruiz-del-Árbol L, Serradilla R. Cirrhotic cardiomyopathy. World J Gastroenterol 2015; 21(41): 11502-11521
- URL: https://www.wjgnet.com/1007-9327/full/v21/i41/11502.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i41.11502