Published online Sep 7, 2015. doi: 10.3748/wjg.v21.i33.9827
Peer-review started: January 19, 2015
First decision: April 13, 2015
Revised: May 20, 2015
Accepted: July 3, 2015
Article in press: July 3, 2015
Published online: September 7, 2015
Processing time: 232 Days and 4.5 Hours
Liposarcomas rarely develop in the aerodigestive tract. Here, we present a primary esophageal liposarcoma that was discovered between the T3 and T7 levels of the esophagus during right pleural exploration of a 51-year-old male patient. The patient had presented with non-specific symptoms, including progressive dysphagia over the previous 6 mo, without complaints of chest or epigastric pain, regurgitation, or weight loss. A radical three-hole esophagectomy was performed. The tumor was extremely large (14 cm × 7.0 cm × 6.5 cm), but completely encapsulated. Upon histological examination, the tumor was diagnosed as a giant, well-differentiated esophageal liposarcoma with a dedifferentiated component. Non-specific radiological and endoscopic results during the clinical work-up delayed diagnosis until post-operative histology was performed. In this report, the clinical, radiological and endoscopic diagnostic challenges specific to the case are discussed, as well as the surgical and pathological findings.
Core tip: Primary esophageal liposarcoma is an extremely rare malignancy. In this case report, a giant, well-differentiated esophageal liposarcoma with a dedifferentiated component was removed from a 51-year-old male patient. The tumor displayed a non-specific appearance on imaging and endoscopy, which prohibited an accurate diagnosis pre-operatively. Therefore, clinical, radiological, and endoscopic aspects of the case, as well as the surgery and pathology of the tumor, are discussed in detail.
- Citation: Lin ZC, Chang XZ, Huang XF, Zhang CL, Yu GS, Wu SY, Ye M, He JX. Giant liposarcoma of the esophagus: A case report. World J Gastroenterol 2015; 21(33): 9827-9832
- URL: https://www.wjgnet.com/1007-9327/full/v21/i33/9827.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i33.9827
Liposarcoma is a rare malignant tumor that usually develops in the soft tissue of the extremities, the trunk or the retroperitoneum, and seldom in the aerodigestive tract. The first report of a primary esophageal liposarcoma was published in 1983[1], and only 30 cases have appeared in the literature since then[2]. Due to the novelty of these tumors, the clinical, radiological, endoscopic, surgical and pathological findings of a case in a Chinese patient are discussed in detail here. Briefly, a giant, well-differentiated esophageal liposarcoma with a dedifferentiated component was identified in a 51-year-old male patient. Treatment included a radical, three-hole esophagectomy to resect the disease.
A 51-year-old Chinese man presented with a 6-mo history of progressive dysphagia without complaints of chest or epigastric pain, regurgitation, or significant weight loss. In the days leading to hospitalization, the patient could not tolerate solid food and had experienced intermittent difficulties ingesting liquids. The clinical history was otherwise unremarkable, and no significant abnormalities were observed upon physical examination.
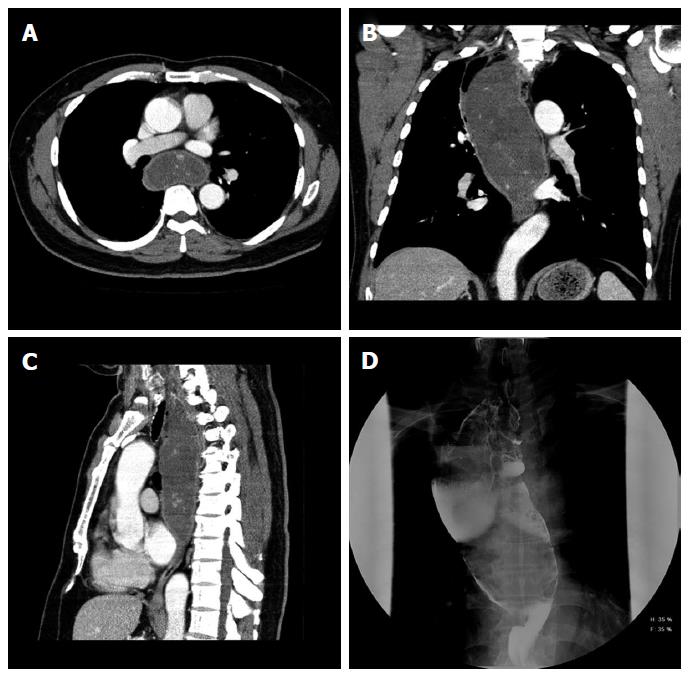
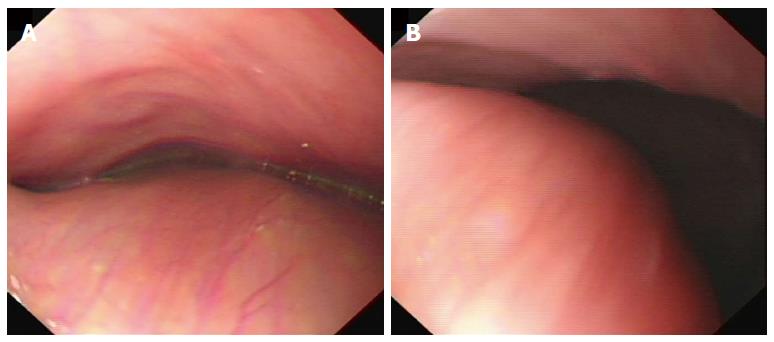
A computed tomographic (CT) scan of the chest and abdomen was performed. The esophagus was found to be extensively dilated (upper and middle thirds) from the thoracic inlet all the way to the inferior pulmonary vein level, over an area of 15 cm in length and 9.5 cm in width (Figure 1A-C). The remaining lower third of the esophagus displayed no abnormalities. An extremely dilated upper and middle esophagus was also evident on the subsequent barium swallow. The contrast passed slowly through the lower third of the esophagus but without any signs of a filling defect (Figure 1D). All radiologic results were consistent with a diagnosis of achalasia. However, further examination performed with a diagnostic flexible esophagoscope revealed a large submucosal lesion or an extrinsic compression encompassing the esophageal lumen at 20 cm to 35 cm from the incisor teeth (Figure 2). The remaining lower region of the esophagus and the gastro-esophageal junction was normal in appearance.
For exploration and radical resection of the disease, a three-hole approach - including a right thoracotomy, midline laparotomy and left cervical incision - was selected due to the gross obstruction and size and location of the lesion. During right pleural exploration, a large tumor was located between levels T3 and T7 in the upper and middle thirds of the esophagus. The tumor was 14 cm × 7.0 cm × 6.5 cm in size. It was remarkably pliable and completely encapsulated. A radical esophagectomy was subsequently performed, and the cervical esophagus was anastomosed end-to-side with a gastric conduit in the neck. The operation was successful, and the patient fully recovered without post-operative complications. The patient was discharged on post-operative day 8 with discharge orders for a soft diet.
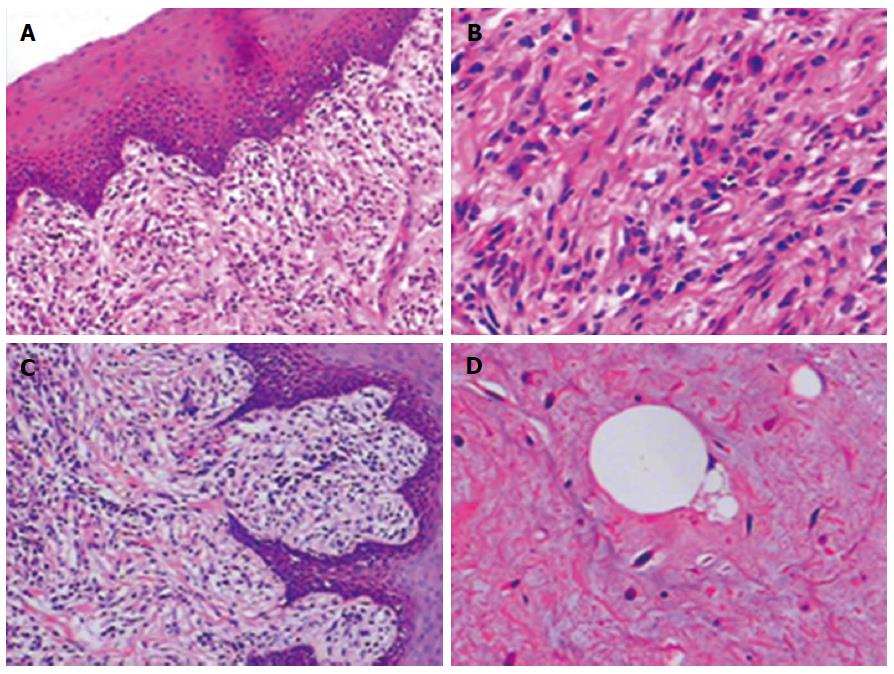
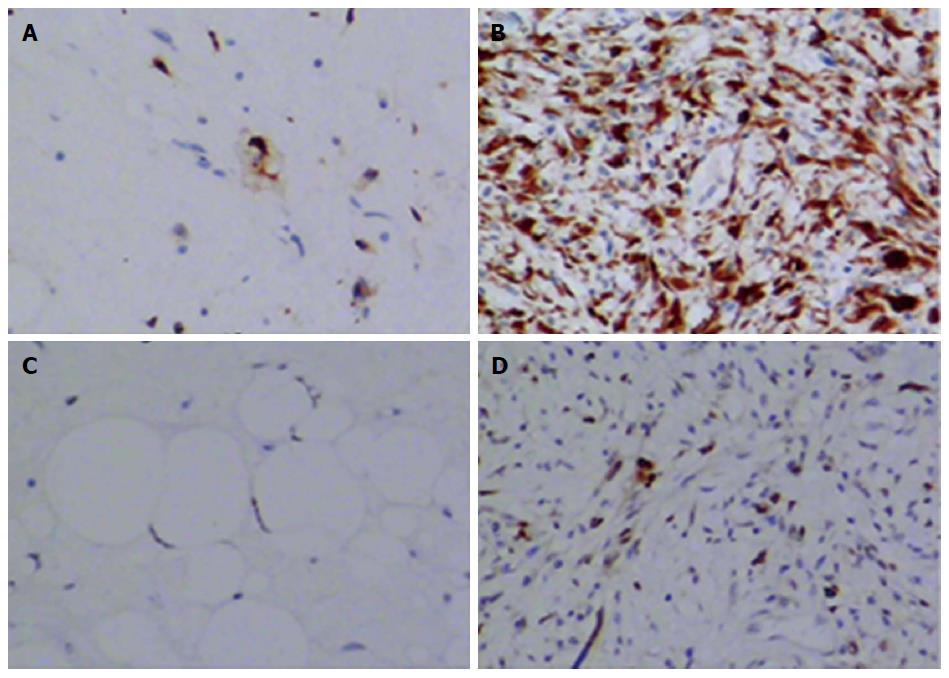
Upon macroscopic examination, the surface of the tumor was found to be covered by normal esophageal mucosa. At one surgical margin of the specimen, a yellow lobulated transmural mass invading the esophageal wall was visible (Figure 3). The diagnosis upon histological examination was a delineated myxoid tumor in the subepithelial stroma. Spindle cells, lipoblasts, and mature fat cells were all present (Figure 4A, B and D). Immunostaining revealed a marker profile (vimentin+, CD117-, S-100+, and CD34+) consistent with a well-differentiated liposarcoma. However, a dedifferentiated component was also present as indicated by the atypia exhibited by the spindle cells in the area between the esophageal mucosa and the tumor (Figure 4C). Immunostaining also revealed strong and weak patterns of expression for CDK4 and MDM2 respectively across both well-differentiated and dedifferentiated areas (Figure 5). Finally, the resection margins and lymph nodes were all free of tumor. The patient therefore required only close follow-up without further treatment.
Although liposarcoma is the most common tumor of mesenchymal origin occurring in adults, development in the esophagus is extremely rare. The incidence of gastrointestinal liposarcoma has been reported to be 0.1% to 5.8% at autopsy, with primary esophageal liposarcomas accounting for only 1.2% to 1.5% of all gastrointestinal lipomas[3,4]. Based on data from the few cases available, esophageal liposarcoma tends to occur predominantly in males (72%) at an average age of 58.4 years (range: 38-73 years) and reaching an average tumor size of 13 cm (range: 4 to 23 cm)[2]. The case in this report also presented with these general clinical features, but the diagnosis remained elusive until surgery and histological analysis had been completed.
Esophageal liposarcoma is generally considered to be a slowly growing tumor. The lesion usually grows until it reaches a considerable size and causes symptoms. The predominant clinical symptoms include progressive dysphagia, nausea, throat discomfort, retrosternal pain, odynophagia, respiratory distress, anemia, tumor regurgitation, and sudden death by asphyxia and foreign body sensation[5]. Progressive dysphagia over a 6-mo period was the main complaint of our patient. However, the symptoms of esophageal liposarcoma might be uncharacteristic making clinical diagnosis difficult. In one case report, it was significant shortness of breath, hoarseness, cough, and chest discomfort that led the patient to hospitalization[6]. In our case, the soft tissue lesion was not identified with the CT scan, and the barium swallow failed to detect any filling defect on the background of a grossly dilated esophagus. In fact, the case was misdiagnosed as achalasia until abnormalities on the esophagoscopy were observed. Thus, the final diagnosis of esophageal liposarcoma was established only after surgery.
Well-differentiated, dedifferentiated, myxoid cell, and pleomorphic are all reported histologic types of esophageal liposarcoma[7]. The most common subtype is well-differentiated esophageal liposarcoma, which comprises up to 70% of all cases[2]. The case presented was also a well-differentiated esophageal liposarcoma, but surprisingly, a small dedifferentiated component was identified in a region between esophageal mucosa and tumor. This finding confirms the existence of heterogeneity in this tumor type and is consistent with the proposal that dedifferentiated liposarcomas are biphasic malignant adipocytic tumors containing areas of well-differentiated liposarcoma with a transition to non-lipogenic sarcoma[8].
The treatment choice for esophageal liposarcoma is surgery. Surgical approaches, however, are diverse and include total or subtotal esophagectomy or minimally invasive approaches, such as endoscopic resection[7,9-11]. The prognosis of esophageal liposarcoma after radical surgery remains unknown as the number of cases published with long-term follow-up is insufficient for rigorous analysis. So far, however, tumors recurred in only 2/15 patients based on the medical records available[12]. Therefore, the local control rate of esophageal liposarcoma by surgery seems acceptable. For the same reason, adjuvant therapy is generally not suggested. Thus, although the exact indications for resection have not been established, total rather than incomplete resection coupled with a close surveillance program is recommended.
The case presented herein involved a well-differentiated liposarcoma of the esophagus harboring a dedifferentiated component. Atypical symptoms and radiological findings led to an initial misdiagnosis of achalasia. This rare, slowly growing tumor thus presents an important differential diagnosis for progressive dysphagia. Surgical resection is recommended as the treatment of choice for both diagnostic and therapeutic purposes.
A 51-year-old Chinese man presented with a 6-mo history of progressive dysphagia without complaints of chest or epigastric pain, regurgitation, or significant weight loss. The patient also experienced difficulties ingesting solid food and liquids immediately prior to consultation.
The patient was diagnosed with a giant, well-differentiated esophageal liposarcoma with a dedifferentiated component measuring 14 cm × 7.0 cm × 6.5 cm in size.
All radiologic results were consistent with a diagnosis of achalasia.
Laboratory tests were not reported.
A computed tomographic scan of the chest and abdomen was performed followed by a barium swallow. Both revealed a grossly dilated esophagus. A final flexible diagnostic esophagoscopy revealed the presence of a large lesion.
The diagnosis upon histological examination was a delineated myxoid tumor in the subepithelial stroma. Spindle cells, lipoblasts, and mature fat cells were all present. A dedifferentiated component was also recognized on the basis of significant atypia in the spindle cells located between the mucosa and tumor.
Treatment included a radical, three-hole esophagectomy and close surveillance without adjuvant therapy.
Approximately 30 cases of esophageal liposarcoma have been reported in the English literature.
A three-hole esophagectomy is a three-incision transthoracic approach for esophagectomy that usually involves a right thoracotomy, a midline laparotomy, and a right cervical incision for esophagogastric anastomosis. Achalasia is a primary esophageal motility disorder characterized by the absence of esophageal peristalsis and impaired relaxation of the lower esophageal sphincter in response to swallowing.
This rare, slowly growing tumor presents an important differential diagnosis for progressive dysphagia. Furthermore, such cases are difficult to diagnose pre-operatively so that surgical resection is recommended as the treatment of choice for both diagnostic and therapeutic purposes.
The manuscript describing a giant esophageal well-differentiated liposarcoma with a dedifferentiated component is of clinical interest due to the rarity of its location and clinical presentation.
P- Reviewer: Gu MJ, Ma YH S- Editor: Yu J L- Editor: A E- Editor: Zhang DN
| 1. | Mansour KA, Fritz RC, Jacobs DM, Vellios F. Pedunculated liposarcoma of the esophagus: a first case report. J Thorac Cardiovasc Surg. 1983;86:447-450. [PubMed] |
| 2. | Sui X, Li Y, Zhao H, Wang J. Giant liposarcoma of the esophagus with Li-Fraumeni-like syndrome. Eur J Cardiothorac Surg. 2011;40:1253-1255. [PubMed] |
| 3. | Hasanabadi MS, Amiri M, Tajedini A, Yazdi AK, Heidarali M, Amali A, Banazadeh M, Mokhtari Z, Azizi MR. Huge myxoid liposarcoma of the esophagus: a case report. Acta Med Iran. 2011;49:118-121. [PubMed] |
| 4. | Fernandez MJ, Davis RP, Nora PF. Gastrointestinal lipomas. Arch Surg. 1983;118:1081-1083. [PubMed] |
| 5. | Chung JJ, Kim MJ, Kim JH, Lee JT, Yoo HS, Kim KW. Imaging findings of giant liposarcoma of the esophagus. Yonsei Med J. 2003;44:715-718. [PubMed] |
| 6. | Smith MA, Kluck E, Jagannath S, Yang SC. Giant multi-polypoid liposarcoma of the esophagus: an atypical presentation. Ann Thorac Surg. 2010;89:610-612. [PubMed] |
| 7. | Jakowski JD, Wakely PE. Rhabdomyomatous well-differentiated liposarcoma arising in giant fibrovascular polyp of the esophagus. Ann Diagn Pathol. 2009;13:263-268. [PubMed] |
| 8. | Torres-Mora J, Moyer A, Topazian M, Alexander J, Wu TT, Seys A, Fritchie K. Dedifferentiated liposarcoma arising in an esophageal polyp: a case report. Case Rep Gastrointest Med. 2012;2012:141693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Aloraini A, Nahal A, Ferri LE. Transoral endoscopic resection of esophageal liposarcoma. Ann Thorac Surg. 2012;94:e121-e122. [PubMed] |
| 10. | Will U, Lorenz P, Urban H, Meyer F. Curative endoscopic resection of a huge pedunculated esophageal liposarcoma. Endoscopy. 2007;39 Suppl 1:E15-E16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Temes R, Quinn P, Davis M, Endara S, Follis F, Pett S, Wernly J. Endoscopic resection of esophageal liposarcoma. J Thorac Cardiovasc Surg. 1998;116:365-367. [PubMed] |
| 12. | Yo I, Chung JW, Jeong MH, Lee JJ, An J, Kwon KA, Rim MY, Hahm KB. Huge liposarcoma of esophagus resected by endoscopic submucosal dissection: case report with video. Clin Endosc. 2013;46:297-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |