Published online Mar 28, 2015. doi: 10.3748/wjg.v21.i12.3671
Peer-review started: September 14, 2014
First decision: October 14, 2014
Revised: November 17, 2014
Accepted: January 8, 2015
Article in press: January 8, 2015
Published online: March 28, 2015
Processing time: 198 Days and 16.2 Hours
AIM: To compare the efficacy and safety of sedation protocols for endoscopic submucosal dissection (ESD) between dexmedetomidine-remifentanil and propofol-remifentanil.
METHODS: Fifty-nine patients scheduled for ESD were randomly allocated into a dexmedetomidine-remifentanil (DR) group or a propofol-remifentanil (PR) group. To control patient anxiety, dexmedetomidine or propofol was infused to maintain a score of 4-5 on the Modified Observer’s Assessment of Alertness/Sedation scale. Remifentanil was infused continuously at a rate of 6 μg/kg per hour in both groups. The ease of advancing the scope into the throat, gastric motility grading, and satisfaction of the endoscopist and patient were assessed. Hemodynamic variables and hypoxemic events were compared to evaluate patient safety.
RESULTS: Demographic data were comparable between the groups. The hemodynamic variables and pulse oximetry values were stable during the procedure in both groups despite a lower heart rate in the DR group. No oxygen desaturation events occurred in either group. Although advancing the scope into the throat was easier in the PR group (“very easy” 24.1% vs 56.7%, P = 0.010), gastric motility was more suppressed in the DR group (“no + mild” 96.6% vs 73.3%, P = 0.013). The endoscopists felt that the procedure was more favorable in the DR group (“very good + good” 100% vs 86.7%, P = 0.042), whereas patient satisfaction scores were comparable between the groups. En bloc resection was performed 100% of the time in both groups, and the complete resection rate was 94.4% in the DR group and 100% in the PR group (P = 0.477).
CONCLUSION: The efficacy and safety of dexmedetomidine and remifentanil were comparable to propofol and remifentanil during ESD. However, the endoscopists favored dexmedetomidine perhaps due to lower gastric motility.
Core tip: Propofol and remifentanil are effectively used for endoscopic procedures. However, deep sedation especially with propofol is frequently associated with cardiorespiratory complications; therefore, it is of interest to identify shallower yet equally effective sedation protocols. Dexmedetomidine allows sedation without respiratory depression, and has also been utilized for sedation for endoscopic procedures. This study compared the efficacy and safety between propofol-remifentanil and dexmedetomidine-remifentanil during endoscopic submucosal dissection (ESD) from the perspective of the endoscopist and the patient. We found that efficacy and safety of dexmedetomidine-remifentanil were comparable to propofol-remifentanil during ESD, but the endoscopists favored the dexmedetomidine-remifentanil regimen perhaps due to lower gastric motility.
- Citation: Kim N, Yoo YC, Lee SK, Kim H, Ju HM, Min KT. Comparison of the efficacy and safety of sedation between dexmedetomidine-remifentanil and propofol-remifentanil during endoscopic submucosal dissection. World J Gastroenterol 2015; 21(12): 3671-3678
- URL: https://www.wjgnet.com/1007-9327/full/v21/i12/3671.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i12.3671
Endoscopic submucosal dissection (ESD) is associated with greater and longer patient discomfort and pain than other endoscopic procedures. Therefore, it is of interest to reduce pain and discomfort associated with ESD[1]. Propofol has been widely used for endoscopic procedures[2,3]. It is safe and effective[4] and is associated with shorter recovery time and better sedation and amnesia levels without an increased risk for cardiopulmonary complications[5] than other traditional sedatives. However, in addition to the dose-dependent respiratory depression of propofol, aspiration pneumonia occurs with an incidence of 2.3% following ESD[6]. Moreover, it is difficult to control sedation depth with propofol[7]. However, its use in combination with other analgesics can offset these complications by reducing the dose of propofol[8].
Dexmedetomidine, a selective α2-adrenoceptor agonist with sedative and analgesic effects, has been successfully used during colonoscopy[9], cystoscopy[10] and ESD[11]. Dexmedetomidine suppresses gastrointestinal motility and inhibits gastric emptying in healthy volunteers[12] whereas propofol does not[13]. Suppressing gastric motility may be crucial for successful ESD.
In this study, we compared the procedural efficacy and patient safety of the use of dexmedetomidine-remifentanil vs propofol-remifentanil during ESD.
This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (ref: 4-2012-0621) and was registered at http://ClinicalTrials.gov (ref: NCT01920113). Written informed consent was obtained from all patients before the procedure. Sixty patients aged > 20 years belonging to American Society of Anesthesiologists classification I-III and scheduled for ESD were enrolled in this prospective, randomized, and endoscopist-blind study from September 2012 to January 2013. Patients with end-organ diseases (i.e., heart failure, respiratory failure, hepatic failure, or renal failure), known drug allergies, or a history of drug abuse were excluded.
The patients were randomly assigned to the dexmedetomidine-remifentanil group (DR group, n = 30) or the propofol-remifentanil group (PR group, n = 30) using a random number table provided by http://www.random.org. Among the 60 patients, data for 59 patients (29 patients in the DR group and 30 patients in the PR group) were analysed; surgical removal was considered in one patient.
Both the endoscopists and patients were blinded to the sedation protocol. None of the patients were pre-medicated. The level of sedation in both groups was targeted to a score of 4-5 on the Modified Observer’s Assessment of Alertness/Sedation scale[14] (MOAA/S, Table 1) for minimal sedation during the entire procedure. For the DR group, a bolus dose of 0.5 μg/kg dexmedetomidine (Precedex®, Abbott, Istanbul, Turkey) was injected intravenously for 5 min before starting the procedure. Thereafter, a continuous infusion dose of 0.3-0.7 μg/kg per hour was given. For the PR group, a bolus injection of 0.5 mg/kg propofol was followed by continuous infusion at a rate of 30 μg/kg per minute (Pofol®, Dongkook Pharm. Co. Ltd., Seoul, South Korea) using an infusion pump (Syringe Pump TE-331, Terumo, Tokyo, Japan). In both groups, remifentanil (Ultiva®, GlaxoSmithKline, Co. Ltd., Genval, Belgium) was infused continuously at the rate of 6 μg/kg per hour beginning 5 min before commencing the procedure.
| Alertness/sedation level | Description |
| 6 | Agitated |
| 5 | Respond readily to name spoken in normal tone (alert) |
| 4 | Lethargic response to name spoken in normal tone |
| 3 | Responds only after name is called loudly, repeatedly, or both |
| 2 | Responds only after mild prodding or shaking |
| 1 | Does not respond to mild prodding or shaking |
| 0 | Does not respond to deep stimulus (asleep) |
We monitored the MOAA/S scale score continuously. If the score was 6 or the patient wanted deeper sedation, a bolus of 10 mg propofol was administered. If the patient complained of pain during the procedure, 0.1 μg/kg remifentanil bolus was administered, and its infusion rate was increased by 0.1 μg/kg per hour.
Hartman’s solution was administered at a rate of 3-5 mL/kg per hour, and 2 L/min oxygen was given through a nasal cannula. Oxygen saturation (SpO2), systolic and diastolic blood pressure (SBP and DBP), electrocardiogram (ECG), and heart rate (HR) were monitored continuously and recorded at 5-min intervals.
The MOAA/S scale score was recorded as follows: just before the procedure (baseline, T0); 1 min after induction of sedation (1 min after a 5 min loading of dexmedetomidine in the DR group and 1 min after the propofol bolus injection in the PR group, T1); as the endoscope was passed into the esophagus (T2); as the tumor margin was marked by argon plasma coagulation (T3); 5 min after an injection of normal saline containing epinephrine (0.01 mg/mL) was given in the gastric submucosa (T4); at dissection of the gastric tumor region from the gastric submucosa (T5); once bleeding control was performed at the gastric bed after dissection (T6); and at the end of the procedure (T7).
The discharge Aldrete score[15] (Table 2) was recorded to document the patient’s general status at the end of the procedure.
| Discharge criteria | Score |
| Activity: Able to move voluntarily or on command | |
| Four extremities | 2 |
| Two extremities | 1 |
| Zero extremities | 0 |
| Respiration | |
| Able to deep breathe and cough freely | 2 |
| Dyspnea, shallow or limited breathing | 1 |
| Apneic | 0 |
| Circulation | |
| Blood pressure ± 20 mmHg of preanesthetic level | 2 |
| Blood pressure ± 20 - 50 mmHg preanesthetic level | 1 |
| Blood pressure ± 50 mmHg of preanesthetic level | 0 |
| Consciousness | |
| Fully awake | 2 |
| Arousable on calling | 1 |
| Not responding | 0 |
| O2 saturation | |
| Able to maintain O2 saturation > 92% on room air | 2 |
| Needs O2 inhalation to maintain O2 saturation > 90% | 1 |
| O2 saturation < 90% even with O2 supplementation | 0 |
All patients were observed in the post-anesthetic care unit (PACU) until their discharge Aldrete score reached 10.
The ease of advancing the scope through the throat (four grades: very easy, easy, slight difficulty, and difficult), gastric motility[16] (four grades: no, mild, moderate, and vigorous) (Table 3), and procedural satisfaction (four grades: very good, good, fair, and bad) were evaluated by the endoscopists. Gastric motility was assessed at the time after the scope had reached to stomach. Thereafter butylscopolamine (20 mg) was administered to suppress gastric motility during the procedure at the request of the endoscopists. The total amount of butylscopolamine used was recorded.
| Grade of gastric motility |
| No |
| No or very weak gating movement of the pyloric ring is observed, but the movement does not show strong contraction |
| → No peristalsis |
| Mild |
| A circular peristaltic wave is formed in the antrum but disappears without reaching the pyloric ring, or circular contraction temporarily occurs immediately before the pyloric ring |
| → Peristaltic wave does not reach the pyloric ring |
| Moderate |
| A pronounced peristaltic wave is formed and reaches the pyloric ring |
| → Peristaltic wave reached the pyloric ring, which opens and closes, showing star-like contraction as a result of the peristaltic wave |
| Vigorous |
| Peristaltic wave is deep and pronounced and proceeds, strangulating the antrum |
| → Peristaltic wave reaches the pyloric ring, and the pyloric ring is totally covered by the wave, the area exhibiting star-like contraction protrudes toward the opening of the pyloric ring, and the mucosa is pushed out from the central part of the opening |
The rate of en bloc resection and complete resection (defined as en bloc resection with tumor-free margins)[17] was compared between the groups.
Patients were also asked about their satisfaction with the procedure (four grades: very good, good, bearable, and unbearable) before discharge from the PACU.
Hemodynamic variables of SBP, DBP, HR, and SpO2 were compared when measuring the MOAA/S score.
All respiratory (apnea and oxygen desaturation) and hemodynamic (hypertension, hypotension, tachycardia, or bradycardia; defined as a change in baseline value of more than 20%) adverse events were recorded. Apnea was defined as not breathing spontaneously for at least 20 s. Oxygen desaturation was defined as SpO2 < 90%. We managed adverse respiratory events with a jaw thrust, mask ventilation, or by increasing oxygen flow. Ephedrine, nicardipine, atropine, or esmolol was administered for adverse hemodynamic events. The total amount of sedative drug and remifentanil were recorded.
The statistical methods of this study were reviewed by statisticians (Mi Kyung Song and Bo Gyoung Ma) from Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, South Korea. Data on baseline characteristics of study participants were presented as mean ± SD for continuous variables or frequency (percentage) for categorical variables. Continuous and categorical variables were tested by using Student’s t test and χ2 test (or Fisher’s exact test), respectively. Repeatedly measured variables such as SpO2, SBP, DBP, and HR were analyzed by a linear mixed model with patient indicator, group, time, and interaction between group and time as fixed effect factors. When the interaction between group and time was significant, post-hoc testing was performed with Bonferroni correction. All statistical tests were two-tailed at a significance level of 0.05. Statistical analyses were performed by using SPSS software (ver. 19.0, SPSS Inc., Chicago, IL, United States) and PASS software (ver. 12, NCSS, LLC, Kaysville, Utah, United States).
The sample size of this study was referred from the previous randomized trial[18] comparing the safety and effectiveness between dexmedetomidine and propofol during oesophagus interventions.
No significant differences were observed in patient demographic data including age, sex ratio, height, weight, snoring history, and ASA classification (Table 4). Tumor characteristics, including histology, macroscopic appearance, location and size measured by the endoscopist were similar between the groups (Table 5).
| DR group(n = 29) | PR group(n = 30) | P value | |
| Age (yr) | 62.1 ± 10.3 | 62.9 ± 12.3 | 0.763 |
| Male | 19 (65.5) | 22 (73.3) | 0.514 |
| Height (cm) | 162.2 ± 7.7 | 164.8 ± 5.8 | 0.274 |
| Weight (kg) | 62.8 ± 8.5 | 65.1 ± 10.2 | 0.276 |
| ASA classification n (%) | 0.390 | ||
| I | 19 (65.5) | 15 (50.0) | |
| II | 9 (31.0) | 12 (40.0) | |
| III | 1 (3.4) | 3 (10.0) | |
| Snoring history | 9 (31.0) | 7 (23.3) | 0.506 |
| DR group(n = 29) | PR group(n = 30) | P value | ||
| Number of lesion | 36 | 32 | ||
| Histology | Adenoma | 19 (52.8) | 17 (53.1) | 0.995 |
| Carcinoma | 16 (44.4) | 14 (43.8) | ||
| Others | 1 (2.8) | 1 (3.1) | ||
| Macroscopic appearance | Elevated | 32 (88.9) | 27 (84.4) | 0.584 |
| Flat or depressed | 4 (11.1) | 5 (15.6) | ||
| Location | Upper body | 3 (8.3) | 3 (9.4) | 0.945 |
| Middle body | 8 (22.2) | 8 (25.0) | ||
| Lower body | 25 (69.4) | 21 (65.6) | ||
| Size (mm) | 15.7 ± 7.0 | 14.0 ± 6.7 | 0.344 |
Dexmedetomidine in the DR group and propofol in the PR group were infused at rates of 0.5 ± 0.3 μg/kg per hour and 23.8 ± 16.5 μg/kg per minute, respectively. The infusion rates of remifentanil were 5.7 ± 1.4 μg/kg per hour and 6.3 ± 4.0 μg/kg per hour in the DR and PR groups, respectively (P = 0.451). Eight and 3 patients in the DR and PR groups, respectively, required propofol as a rescue sedative (P = 0.083) at 16.9 ± 10.3 mg and 13.3 ± 5.8 mg (P = 0.596), respectively (Table 6).
| DR group(n = 29) | PR group(n = 30) | P value | |
| Sedation duration (min) | 42.8 ± 26.7 | 37.6 ± 18.5 | 0.477 |
| Dexmedetomidine infusion rate (μg/kg per hour) | 0.5 ± 0.3 | ||
| Propofol infusion rate (μg/kg per minute) | 23.8 ± 16.5 | ||
| Remifentanil infusion rate (μg/kg per hour) | 5.7 ± 1.4 | 6.3 ± 4.0 | 0.451 |
| Additional propofol required | |||
| Patients | 8 (27.6) | 3 (10.0) | 0.083 |
| Dose (mg) | 16.9 ± 10.3 | 13.3 ± 5.8 | 0.596 |
| Butylscopolamine use | |||
| Patients | 4 (13.8) | 10 (33.3) | 0.078 |
| Dose (mg) | 3.4 ± 9.3 | 10.0 ± 16.4 | 0.066 |
Complete resection was possible with 94.4% of the 36 en bloc resections in the DR group and 100.0% of the 32 en bloc resections in the PR group. Moreover, the duration of sedation was similar (P = 0.477).
Although the endoscope was more easily advanced through the throat in the PR group than in the DR group (P = 0.010), low-grade gastric motility (no or mild) was more frequent in the DR group (96.6% vs 73.3%, P = 0.013). Butylscopolamine was administered to 10 patients of the PR group compared with 4 patients of the DR group (P = 0.078).
While the endoscopists were satisfied with the procedural performance and judged the procedures as favorable in all patients in the DR group and in only 86.7% of patients in the PR group (P = 0.042), patient satisfaction was comparable between the two groups (Table 7).
| DR group(n = 29) | PR group(n = 30) | P value | |
| Advancing scope into throat | 0.010 | ||
| Very easy | 7 (24.1) | 17 (56.7) | |
| Easy | 14 (48.3) | 12 (40.0) | |
| Slight difficult | 1 (3.4) | 1 (3.3) | |
| Difficult | 7 (24.1) | 0 (0.0) | |
| Gastric motility | 0.101 | ||
| No | 21 (72.4) | 16 (53.3) | |
| Mild | 7 (24.1) | 6 (20.0) | |
| Moderate | 1 (3.4) | 7 (23.3) | |
| Vigorous | 0 (0.0) | 1 (3.3) | |
| Low: No + mild | 28 (96.6) | 22 (73.3) | 0.013 |
| High: Moderate + vigorous | 1 (3.4) | 8 (26.7) | |
| Endoscopist’s satisfaction | 0.216 | ||
| Very good | 21 (72.4) | 17 (56.7) | |
| Good | 8 (27.6) | 9 (30.0) | |
| Fair | 0 (0.0) | 2 (6.7) | |
| Bad | 0 (0.0) | 2 (6.7) | |
| Favorable: Very good + good | 29 (100.0) | 26 (86.7) | 0.042 |
| Unfavorable: Fair + bad | 0 (0.0) | 4 (13.3) | |
| Patients’ satisfaction of sedation | 0.616 | ||
| Very good | 4 (13.8) | 7 (23.3) | |
| Good | 21 (72.4) | 20 (66.7) | |
| Bearable | 4 (13.8) | 3 (10.0) | |
| Unbearable | 0 (0.0) | 0 (0.0) |
The Aldrete score at the end of the procedure was not different between the groups (9.5 ± 0.6 in the DR group and 9.4 ± 0.6 in the PR group, P = 0.924) and all patients left the PACU within 30 min (21.2 ± 6.8 min in the DR group and 20.4 ± 5.8 min in the PR group, P = 0.636).
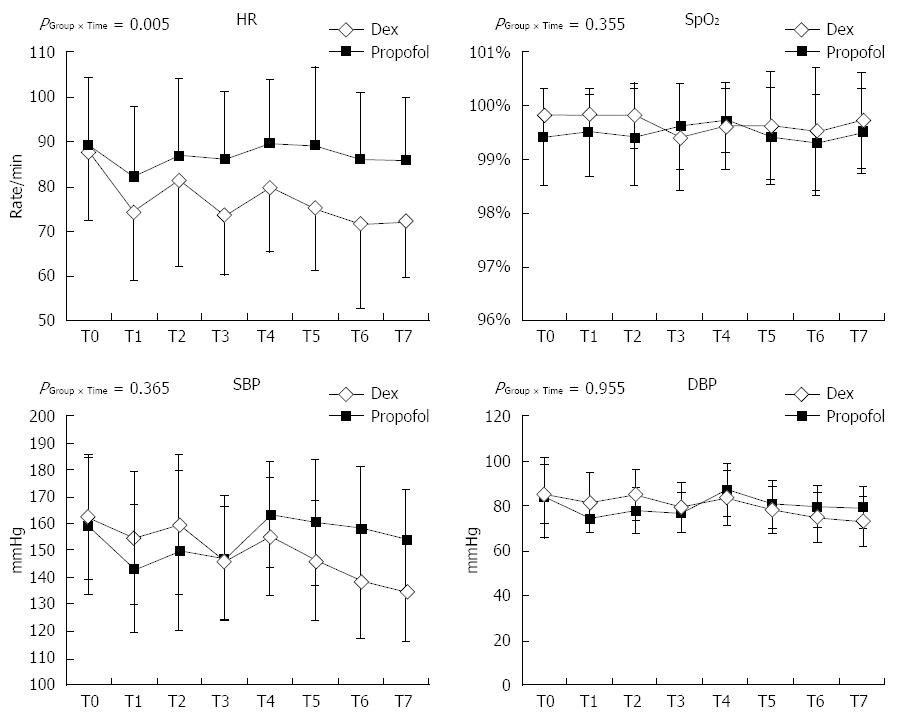
No differences in the MOAA/S scale score, SBP, DBP, or SpO2 were observed. However, the mean change of HR over time was different between DR and PR groups (Figure 1). No cases of oxygen desaturation or any adverse hemodynamic events were observed during the ESD procedures in either group.
We found that minimal sedation using dexmedetomidine-remifentanil could be substituted for propofol-remifentanil during ESD, and that the endoscopists seemed to be satisfied with the procedural efficacy perhaps due to low gastric motility.
This study has some clinical implications regarding the sedating protocol for ESD. First, our results suggest the importance of analgesics and optimal sedation level to avoid patient anxiety. ESD was safely performed under MOAA/S sedation levels of 4-5 if adequate analgesic was provided. As shown in Figure 1, no patient needed management due to hemodynamic instability or adverse respiratory events despite the decreased HR in the DR group. We believe that continuous infusion of remifentanil enabled the patients to tolerate this procedure well in an orientated and anxiety-free state. The analgesic requirement for a painful procedure was evident in a previous colonoscopy trial, which was terminated early before enrolling the planned number of patients because of the higher rate of supplemental fentanyl required and adverse hemodynamic events in the group of patients administered dexmedetomidine alone[19]. International sedation guidelines for gastrointestinal endoscopic procedures[20-22] recommend sedating patients to improve procedural performance. However, the adequate level of sedation for patients has not been well defined (conscious sedation vs deep sedation). Takimoto et al[11] compared the efficacy and safety of conscious sedation for ESD targeting a Ramsay sedation score (RSS) of 2-3 among propofol, dexmedetomidine, and midazolam. They found that dexmedetomidine provided comparable hemodynamic stability and improved oxygen saturation as well as no major surgical complications compared to propofol or midazolam. In comparison, two patients who received propofol or midazolam developed gastric perforation. An RSS of 2-3 represents a level of sedation that is similar to, but slightly deeper than, the MOAA/S of 4-5 used in the present study (MOAA/S 4 = responding to normal verbal tone; RSS 3 = responding to commands). Sasaki et al[19] reported hypoxemia in 15.9%-17.8% of patients and hypotension in 19.3%-34.4% of patients, suggesting a deeper sedation level and a higher rate of complications. In the present study, minimal sedation, regardless of the group, allowed the patients to achieve an Aldrete score of 9.5 at the end of the procedure and to leave the PACU within 30 min. Fast recovery may also be an economic benefit of minimal sedation. However, further pharmaco-economic evaluation between propofol and dexmedetomidine will not be discussed here because of the costal differences of medications among countries.
Second, regarding procedural performance, the endoscopists felt that the endoscope could be more easily advanced into the throat with propofol (endoscopists reported the insertion “very easy” in 7 of 29 patients in the DR group vs 17 of 30 patients in the PR group, P = 0.01). The underlying causes of this difference are unclear but might be explained, in part, by the different effect of propofol and dexmedetomidine on the pharyngeal function. Kiriyama et al[23] assessed the effects of a bolus of 0.5 mg/kg propofol injected before ESD compared to no bolus of propofol and found that the propofol bolus decreased pharyngeal muscle tone and obtunded the scope-stimulated pharyngeal reflex in 77% of patients compared to 21% of patients with no bolus. Therefore, in the present study, the intact pharyngeal function in the DR group may have made it more difficult for the endoscopists to advance the scope into the throat.
Inhibiting gastric motility is crucial for successful performance of ESD, and this is the first report of endoscopist evaluated gastric motility during ESD in relation to two different sedation protocols (Table 7). The endoscopists graded gastric motility as low (no and mild among four grades) in 96.6% of the DR group and in 73.3% of the PR group (P = 0.013). Corroborating the report of lower gastric motility by the endoscopists, patients in the DR group required butylscopolamine less frequently to suppress gastric motility than those in the PR group. The effects of dexmedetomidine on gastric motility seemed to differ according to subject and dosage. In a previous study, infusion with a 1.0 μg/kg loading dose for 20 min followed by infusion of 0.7 μg/kg per hour inhibited gastric emptying in healthy volunteers, as measured by paracetamol absorption compared to 0.1 mg/kg morphine or placebo[12]. In contrast, Memiş et al[24] found no difference in gastric emptying time between propofol (2 mg/kg per hour) and dexmedetomidine (0.2 μg/kg per hour) for 5 h in critically ill patients. This discrepancy may have resulted from the different doses of drugs and measuring methods (direct visualization vs indirect paracetamol absorption test) used in the two studies. Dexmedetomidine itself does not alter gastric motility in rats but markedly enhances the inhibitory effect of morphine on gastric motility[25]. We are uncertain of the interactive effect of dexmedetomidine and remifentanil on gastric motility. We believed that both sedation protocols were effective for ESD considering that the endoscopists were able to perform complete resection at a comparable rate between the two groups (94.4% vs 100%).
However, our study had some limitations. We analyzed a small number of patients, which limited the statistical power of our results. If we carry out the follow-up study, 143 subjects will be needed for each group to keep the statistical power of 80%. Gastric motility did not differ between the two groups (P = 0.101) when measured using the four grades (no, mild, moderate, and vigorous); however, there was a significant difference when just two grades of low (no/mild) and high (moderate/vigorous) were applied (P = 0.013). This same issue was also observed with the statistical analysis of endoscopists’ satisfaction. We did not find any significant difference when the ratings were based on four grades (very good, good, fair, and bad). However, when satisfaction was divided into favorable (very good/good) and unfavorable (fair/bad), the endoscopists were in favor of the dexmedetomidine-remifentanil treatment (favorable, 100% in the DR group vs 86.7% in the PR group, P = 0.042). Although there were no serious adverse respiratory events during ESD in both groups, we could not exclude the possibility of hypercapnia because we did not measure the partial pressure of carbon dioxide (PaCO2) through arterial blood gas analysis. To blind endoscopists from the type of anesthesia, we covered the patients’ venous access sites with a drape; however, we are unsure whether endoscopists were able to correctly identify the type of sedative drugs from the difference in the pharmacologic properties between dexmedetomidine and propofol. Therefore, we could not completely eliminate the bias of personal preference when they answered the questionnaires. Finally, our study design did not include a psychometric test for patients or comprehensive questionnaires to assess patients and endoscopists satisfaction as suggested by Vargo et al[26].
In conclusion, use of dexmedetomidine and remifentanil targeting minimal sedation could be substituted for propofol-remifentanil sedation during ESD procedure. However, the effect of suppressing gastric motility with dexmedetomidine-remifentanil sedation needs further studies with a greater number of subjects.
We thank Mi Kyung Song and Bo Gyoung Ma (Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, South Korea) for critical reading of the manuscript and their statistical support.
Endoscopic submucosal dissection (ESD) is accompanied with greater and longer patient discomfort and pain than conventional endoscopic procedures. Therefore, a combination regimen with a sedative and an analgesic, such as propofol and remifentanil, is recommended. However, propofol depresses respiratory function in a dose-dependent manner and aspiration pneumonia can occur. Dexmedetomidine, another sedative agent with lack of respiratory depression, suppresses gastrointestinal motility and may improve the chances for successful ESD. Thus, we compared the procedural efficacy and patient safety of dexmedetomidine-remifentanil to propofol-remifentanil during ESD.
Aspiration pneumonia occurs with an incidence of 2.3% following ESD under sedation with propofol perhaps due to dose-dependent respiratory depression. Dexmedetomidine, a selective α2-adrenoceptor agonist with sedative and analgesic effects that preserves ventilator function, has been successfully used during colonoscopy. In addition, dexmedetomidine suppresses gastrointestinal motility in healthy volunteers whereas propofol does not.
The sedation level was maintained at MOAA/S of 4-5 with either sedating regimen (propofol-remifentanil or dexmedetomidine-remifentanil). What we found in this study were as follows. The patients tolerated the ESD procedure well and safely under minimal sedation under either sedating regimen with pain adequately controlled. However, the endoscopists favored the regimen of dexmedetomidine-remifentanil perhaps due to the suppression of gastric motility.
Because the endoscopic procedure can vary greatly among patients in regard to anxiety, pain, and duration, it is important to regard sedation and analgesia separately to avoid over-sedation. Dexmedetomidine may provide benefits to the sedation regimen during ESD because it has sedative effects, analgesic effects, the ability to suppress gastric mobility and, more importantly, the ability to preserve respiratory drive.
The endoscopic submucosal dissection procedure lasts for hours and is accompanied by pain. Propofol and dexmedetomidine are commonly used sedative agents that work through GABAA receptor and a selective α2-adrenoceptor, respectively. Remifentanil is a synthetic opioid with rapid onset and offset of action.
The authors compared the efficacy and safety of sedation between dexmedetomidine-remifentanil and propofol-remifentanil for use during ESD. Fifty-nine patients scheduled for ESD were randomly assigned to a dexmedetomidine-remifentanil group or a propofol-remifentanil group. The efficacy and safety of dexmedetomidine and remifentanil were comparable to propofol and remifentanil during ESD. The endoscopists favored dexmedetomidine mainly due to lower gastric motility.
P- Reviewer: Herszenyi L, Goenka MK, Tepes B, Yoshiji H S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
| 1. | Sasaki T, Tanabe S, Ishido K, Azuma M, Katada C, Higuchi K, Koizumi W. Recommended sedation and intraprocedural monitoring for gastric endoscopic submucosal dissection. Dig Endosc. 2013;25 Suppl 1:79-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Kiriyama S, Gotoda T, Sano H, Oda I, Nishimoto F, Hirashima T, Kusano C, Kuwano H. Safe and effective sedation in endoscopic submucosal dissection for early gastric cancer: a randomized comparison between propofol continuous infusion and intermittent midazolam injection. J Gastroenterol. 2010;45:831-837. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Byrne MF, Chiba N, Singh H, Sadowski DC. Propofol use for sedation during endoscopy in adults: a Canadian Association of Gastroenterology position statement. Can J Gastroenterol. 2008;22:457-459. [PubMed] [Cited in This Article: ] |
| 4. | Wehrmann T, Kokabpick S, Lembcke B, Caspary WF, Seifert H. Efficacy and safety of intravenous propofol sedation during routine ERCP: a prospective, controlled study. Gastrointest Endosc. 1999;49:677-683. [PubMed] [Cited in This Article: ] |
| 5. | Sethi S, Wadhwa V, Thaker A, Chuttani R, Pleskow DK, Barnett SR, Leffler DA, Berzin TM, Sethi N, Sawhney MS. Propofol versus traditional sedative agents for advanced endoscopic procedures: a meta-analysis. Dig Endosc. 2014;26:515-524. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Park CH, Min JH, Yoo YC, Kim H, Joh DH, Jo JH, Shin S, Lee H, Park JC, Shin SK. Sedation methods can determine performance of endoscopic submucosal dissection in patients with gastric neoplasia. Surg Endosc. 2013;27:2760-2767. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Coté GA, Hovis RM, Ansstas MA, Waldbaum L, Azar RR, Early DS, Edmundowicz SA, Mullady DK, Jonnalagadda SS. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8:137-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 185] [Cited by in F6Publishing: 184] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 8. | Shin S, Lee SK, Min KT, Kim HJ, Park CH, Yoo YC. Sedation for interventional gastrointestinal endoscopic procedures: are we overlooking the “pain”? Surg Endosc. 2014;28:100-107. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Dere K, Sucullu I, Budak ET, Yeyen S, Filiz AI, Ozkan S, Dagli G. A comparison of dexmedetomidine versus midazolam for sedation, pain and hemodynamic control, during colonoscopy under conscious sedation. Eur J Anaesthesiol. 2010;27:648-652. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 66] [Cited by in F6Publishing: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Arpaci AH, Bozkırlı F. Comparison of sedation effectiveness of remifentanil-dexmedetomidine and remifentanil-midazolam combinations and their effects on postoperative cognitive functions in cystoscopies: A randomized clinical trial. J Res Med Sci. 2013;18:107-114. [PubMed] [Cited in This Article: ] |
| 11. | Takimoto K, Ueda T, Shimamoto F, Kojima Y, Fujinaga Y, Kashiwa A, Yamauchi H, Matsuyama K, Toyonaga T, Yoshikawa T. Sedation with dexmedetomidine hydrochloride during endoscopic submucosal dissection of gastric cancer. Dig Endosc. 2011;23:176-181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 12. | Iirola T, Vilo S, Aantaa R, Wendelin-Saarenhovi M, Neuvonen PJ, Scheinin M, Olkkola KT. Dexmedetomidine inhibits gastric emptying and oro-caecal transit in healthy volunteers. Br J Anaesth. 2011;106:522-527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Chassard D, Lansiaux S, Duflo F, Mion F, Bleyzac N, Debon R, Allaouchiche B. Effects of subhypnotic doses of propofol on gastric emptying in volunteers. Anesthesiology. 2002;97:96-101. [PubMed] [Cited in This Article: ] |
| 14. | Chernik DA, Gillings D, Laine H, Hendler J, Silver JM, Davidson AB, Schwam EM, Siegel JL. Validity and reliability of the Observer‘s Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244-251. [PubMed] [Cited in This Article: ] |
| 15. | Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7:89-91. [PubMed] [Cited in This Article: ] |
| 16. | Hiki N, Kaminishi M, Yasuda K, Uedo N, Honjo H, Matsuhashi N, Hiratsuka T, Sekine C, Nomura S, Yahagi N. Antiperistaltic effect and safety of L-menthol sprayed on the gastric mucosa for upper GI endoscopy: a phase III, multicenter, randomized, double-blind, placebo-controlled study. Gastrointest Endosc. 2011;73:932-941. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Okada K, Tsuchida T, Ishiyama A, Taniguchi T, Suzuki S, Horiuchi Y, Matsuo Y, Yoshizawa N, Suganuma T, Omae M. Endoscopic mucosal resection and endoscopic submucosal dissection for en bloc resection of superficial pharyngeal carcinomas. Endoscopy. 2012;44:556-564. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Eberl S, Preckel B, Bergman JJ, Hollmann MW. Safety and effectiveness using dexmedetomidine versus propofol TCI sedation during oesophagus interventions: a randomized trial. BMC Gastroenterol. 2013;13:176. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Sasaki T, Tanabe S, Azuma M, Sato A, Naruke A, Ishido K, Katada C, Higuchi K, Koizumi W. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection: a randomized prospective phase II clinical trial. Endoscopy. 2012;44:584-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Heneghan S, Myers J, Fanelli R, Richardson W. Society of American Gastrointestinal Endoscopic Surgeons (SAGES) guidelines for office endoscopic services. Surg Endosc. 2009;23:1125-1129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-American. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004-1017. [PubMed] [Cited in This Article: ] |
| 22. | Cohen LB, Ladas SD, Vargo JJ, Paspatis GA, Bjorkman DJ, Van der Linden P, Axon AT, Axon AE, Bamias G, Despott E. Sedation in digestive endoscopy: the Athens international position statements. Aliment Pharmacol Ther. 2010;32:425-442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Kiriyama S, Naitoh H, Fukuchi M, Fukasawa T, Saito K, Tabe Y, Yamauchi H, Yoshida T, Kuwano H. Evaluation of Pharyngeal Function between No Bolus and Bolus Propofol Induced Sedation for Advanced Upper Endoscopy. Diagn Ther Endosc. 2014;2014:248097. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Memiş D, Dökmeci D, Karamanlioğlu B, Turan A, Türe M. A comparison of the effect on gastric emptying of propofol or dexmedetomidine in critically ill patients: preliminary study. Eur J Anaesthesiol. 2006;23:700-704. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Asai T, Mapleson WW, Power I. Interactive effect of morphine and dexmedetomidine on gastric emptying and gastrointestinal transit in the rat. Br J Anaesth. 1998;80:63-67. [PubMed] [Cited in This Article: ] |
| 26. | Vargo J, Howard K, Petrillo J, Scott J, Revicki DA. Development and validation of the patient and clinician sedation satisfaction index for colonoscopy and upper endoscopy. Clin Gastroenterol Hepatol. 2009;7:156-162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |