Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Dec 7, 2014; 20(45): 16996-17010
Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.16996
Published online Dec 7, 2014. doi: 10.3748/wjg.v20.i45.16996
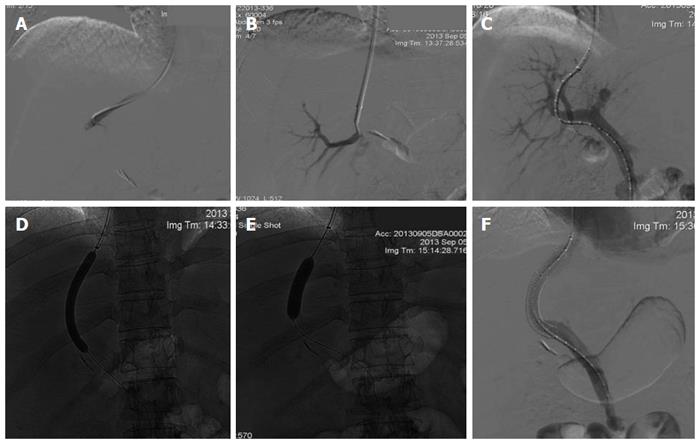
Figure 1 Conventional transjugular intrahepatic portosystemic shunt insertion technique.
A: From a transjugular approach, the right hepatic vein is catheterized; B: A needle inserted through the catheter is used to puncture the liver parenchyma and enters a portal vein branch; C: Transhepatic portogram with the tip of a calibrated catheter at the portosplenic confluence. This catheter is used to measure the length of the parenchymal tract for endograft placement; D: The parenchymal tract is then dilated with an angioplasty balloon to allow passage of the transjugular intrahepatic portosystemic shunt (TIPS) sheath into the portal vein; E: Once stent is fully deployed, an angioplasty balloon is used again to dilate the created tract to obtain the desirable portosystemic gradient (PSG); F: Trans-TIPS portal venography shows flow through the deployed stent. Peripheral portal vein branches are no longer opacified because of reversal of flow.
- Citation: Siramolpiwat S. Transjugular intrahepatic portosystemic shunts and portal hypertension-related complications. World J Gastroenterol 2014; 20(45): 16996-17010
- URL: https://www.wjgnet.com/1007-9327/full/v20/i45/16996.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i45.16996