INTRODUCTION
IgG4-related disease has been widely recognized over the last decade[1]. Type 1 autoimmune pancreatitis is a prototypic manifestation of this systemic condition, and investigations of autoimmune pancreatitis led to the establishment of a novel entity, “IgG4-related disease”[2-4]. IgG4-related autoimmune pancreatitis is sometimes accompanied by synchronous or metachronous lesions at other anatomical sites. Previous studies suggested that retroperitoneal fibrosis is the most commonly associated condition outside the pancreatobiliary system in patients with IgG4-related autoimmune pancreatitis[5,6]. Tubulointerstitial nephritis is another well-known manifestation of IgG4-related disease. Other urinary tract organs that can be affected by IgG4-related disease include the renal pelvis and ureter. Interestingly, reproductive-organ involvements such as IgG4-related prostatitis have been also confirmed in male patients[7-12].
In this paper, we review features of retroperitoneal and reproductive-organ manifestations related to IgG4-related autoimmune pancreatitis to promote their better understanding and management. We did not include IgG4-related tubulointerstitial nephritis, as it has already been well described[13,14].
RESEARCH
A PubMed search was performed for articles published until November 2013 using the keywords of IgG4, pancreatitis, and retroperitoneal fibrosis or testis or prostate. We also referred to studies published in Japanese, as many studies on this entity have been conducted in Japan. Written informed consent was obtained from all the patients for case presentation.
IgG4-RELATED RETROPERITONEAL FIBROSIS: GENERAL ASPECTS
An association between serum IgG4 elevation and autoimmune pancreatitis was first reported by Hamano et al[15] in 2001. The same group also described a case of IgG4-related pancreatitis complicated by retroperitoneal fibrosis, where abundant IgG4-positive plasma cells were histologically identified[16]. This is the first proven case of IgG4-related retroperitoneal fibrosis in the literature. In 2006, Kamisawa et al[17] suggested that IgG4-related pancreatitis and retroperitoneal fibrosis belong to a systemic condition, which is now recognized as IgG4-related disease. Since then, many papers have described IgG4-related retroperitoneal fibrosis, but most of them are case reports.
It is worth emphasizing several aspects of IgG4-related retroperitoneal fibrosis. Firstly, some patients present with isolated IgG4-related retroperitoneal fibrosis with no identifiable extra-retroperitoneal lesions. Secondly, retroperitoneal fibrosis is not always IgG4-related. Only approximately 60% of retroperitoneal fibrosis is IgG4-related. Due to marked overlap in clinical features between IgG4-related and non-related cases, this discrimination is not straightforward without histological analysis[18,19]. Yet, if a patient is younger than 40 years, non-IgG4-related retroperitoneal fibrosis is more likely.
The diagnosis of IgG4-related disease thus requires a multidisciplinary approach, where serological tests, tissue diagnosis, and imaging examination need to be considered. Serum IgG4 elevation is highly sensitive, but not entirely specific for this condition. IgG4 elevations up to twice the upper limit of the normal range (280 mg/dL) in the serum can be seen in a variety of diseases, including both inflammatory and neoplastic conditions. IgG4 elevations of more than 280 mg/dL are highly specific for this condition.
IgG4-RELATED RETROPERITONEAL FIBROSIS: PATHOLOGY
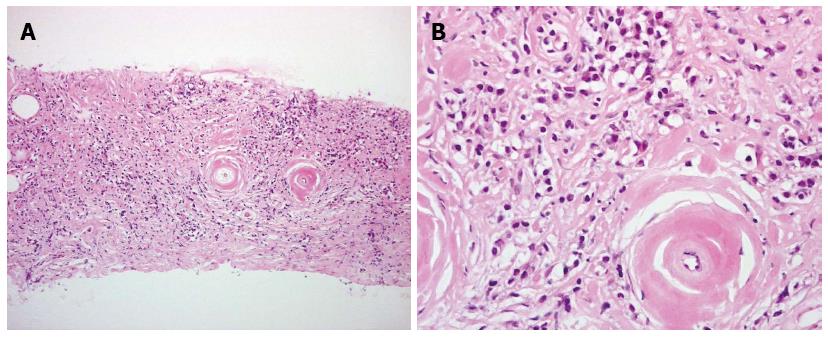
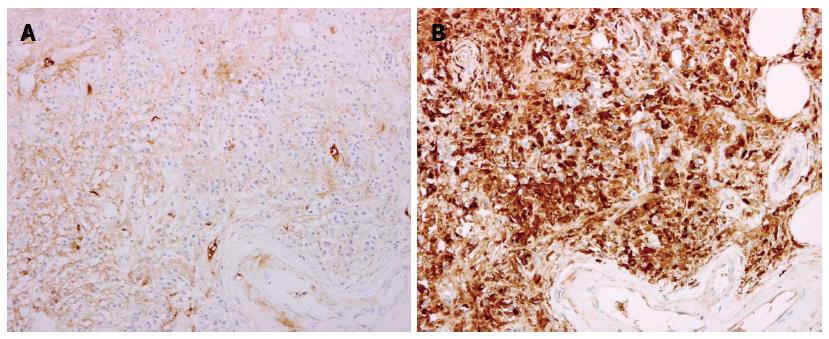
IgG4-related retroperitoneal fibrosis is histologically characterized by massive lymphoplasmacytic infiltration, storiform fibrosis, and obliterative phlebitis (Figure 1)[14,20]. IgG4-positive plasma cells should be diffusely present in inflamed area (> 30 cells/high power field) (Figure 2). The rate of IgG4/IgG-positive plasma cells is at least over 40%, typically over 70%[21]. As IgG4-positive plasma cell infiltration is not entirely specific for this condition, the ratio of them to IgG-positive plasma cells is important to avoid overdiagnosis. Histological findings contradicting a diagnosis of IgG4-related retroperitoneal fibrosis include neutrophilic infiltration, necrosis, discrete granuloma, and necrotizing arteritis.
Figure 1 Histological findings with core needle biopsy: Fibrosis and inflammatory reaction with dense infiltration of abundant lymphocytes and plasma cells.
A: Low magnification; B: High magnification.
Figure 2 Immunopathological findings: infiltrating cells represent lymphocytes and IgG4-positive plasma cells.
A: IgG4 staining; B: IgM staining.
IgG4-RELATED RETROPERITONEAL FIBROSIS: CLINICAL MANIFESTATION
Clinical presentations of IgG4-related retroperitoneal fibrosis are variable. About a half of the patients are believed to be symptom-free. Patients sometimes describe abdominal or back pain and edema of the lower extremities. Once ureters are blocked, symptoms related to hydronephrosis or renal failure may appear.
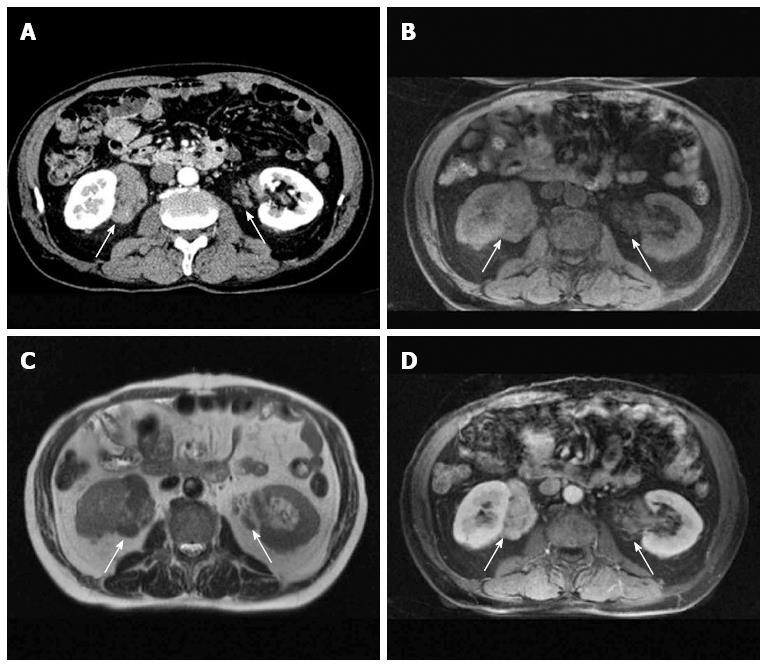
The spectrum of imaging features is also wide, including soft tissue masses sometimes involving the ureters or renal pelvis (Figure 3), aortic wall thickening involving adjacent soft tissue (Figure 4), or plaque-like diffuse fibrosis[22-24]. On computed tomography (CT), the lesions exhibit a soft-tissue density. On magnetic resonance imaging (MRI), they show a low to intermediate signal intensity on T1-weighted images and various signal intensity patterns on T2-weighted images according to the inflammatory activity (Figure 3). Contrast-enhanced images are useful to estimate the degree of fibrosis and inflammatory activity[25,26].
Figure 3 Localized pseudotumors (arrows) in a 67-year-old man with IgG4-related retroperitoneal fibrosis and autoimmune pancreatitis.
A: Contrast-enhanced CT; B: T1-weighted; C: T2-weighted; D: Contrast-enhanced MRI.
Figure 4 Pseudotumor spread in the retroperitoneum surrounding the abdominal aorta and vena cava (arrow).
IgG4-RELATED RETROPERITONEAL FIBROSIS: FUNCTIONAL PROBLEMS
Hydronephrosis related to retroperitoneal fibrosis impairs the renal function, eventually leading to renal insufficiency. Maeta et al[27] reported a rare case of acute renal failure due to IgG4-related retroperitoneal fibrosis. Ureteral obstruction was described in 45%-65% of reported patients with IgG4-related retroperitoneal fibrosis[5,6,12,22,24,27-43]. Yet, assuming that many other patients are not reported, how often IgG4-related retroperitoneal fibrosis is associated with hydronephrosis remains unknown. Interestingly, we realized that the left kidney is more commonly affected by this complication in reported cases[5,6,12,22,24,27,29-42]. Tsuboi et al[28] reported a 62-year-old man with IgG4-related systemic manifestations, who had left hydronephrosis due to a retroperitoneal pseudotumor. Hart et al[12] reported a 67-year-old man who had IgG4-related autoimmune pancreatitis and retroperitoneal fibrosis with hydronephrosis in the left kidney. Two additional cases also had left hydronephrosis[29,30]. Given the fact that most of the patients had IgG4-related autoimmune pancreatitis, the left-sided predominance may be related to the anatomical location of the pancreas. Bilateral hydronephrosis can be also seen at the initial presentation, as described by Miura et al[31] and Takenaka et al[32]. Hydronephrosis is not common in retroperitoneal fibrosis affecting the renal hilum, as reported by Miyajima et al[23].
MANAGEMENT OF IgG4-RELATED RETROPERITONEAL FIBROSIS: PHARMACOLOGICAL THERAPY
The same as for other IgG4-related diseases, steroid therapy is highly effective for IgG4-related retroperitoneal fibrosis[29-31]. However, for patients with ureteral obstruction, how to preserve the renal function is another aspect of treatment. Because of the lack of consensus guidelines for this particular condition, we need to decide on the therapeutic plan (i.e., corticosteroids, ureteral stent) based on the renal function of patients on a case-by-case basis. For patients without severe uremia or fluid retention, oral prednisolone is the most likely treatment of choice. Additional urological intervention such as ureteral stenting may be an option if the obstruction remains even after steroid therapy. Imaging studies involving CT are helpful to assess the effects of steroid therapy[26,37,38].
According to the literature, initial doses vary from 20 mg to 100 mg once daily[28-30,32,33]. A 52-year-old man with IgG4-related pancreatitis and periaortic retroperitoneal fibrosis without urinary tract obstruction was successfully treated with an initial dose of prednisolone of 30 mg[33]. Tsuboi et al[28] reported a 62-year-old man with systemic disease, who had left hydronephrosis due to a pseudotumor, successfully managed with prednisolone of 30 mg. Miura et al[31] reported an 80-year-old man without pancreatic swelling. His bilateral hydronephrosis was treated successfully with prednisolone of 25 mg. A 51-year-old man with systemic manifestations and bilateral incomplete ureteral obstruction was successfully treated with 50 mg of prednisolone[32]. Both the 67-year-old and 79-year-old men reported by Kikuno et al[29] and Nishimura et al[30] respectively, were also successfully treated with prednisolone of 30 mg. Low dose prednisolone therapy (initial dose: 0.5-0.6 mg/kg or 30 mg/body daily) with tapering has been the therapeutic standard with encouraging results (recovery rate greater than 90%), the same as for other manifestations of IgG4-related disease[28,31,43].
MANAGEMENT OF IgG4-RELATED RETROPERITONEAL FIBROSIS: UROLOGICAL INTERVENTION
Marked effects of steroid therapy are usually expected in the first couple of weeks. When patients have advanced uremia, severe fluid retention, or ureteral obstruction with symptoms, however, an emergent ureteral stent or nephrostomy is required[27]. Unilateral interventions may be sufficient for recovery from the life-threatening situation. Ureteral stenting is currently the interventional standard. Hart et al[12] reported a 67-year-old man who had IgG4-related autoimmune pancreatitis and retroperitoneal fibrosis with hydronephrosis of the left kidney. He underwent ureteral stenting for mild elevation of the serum creatinine level (1.6 mg/dL). Another 74-year-old Chinese man with hydronephrosis received ureteral stenting to relieve ureteral obstruction and associated pain[38]. IgG4-related retroperitoneal fibrosis was thereafter diagnosed in this case. The stent was removed after confirming that pseudotumorous retroperitoneal fibrosis responded well to steroid therapy.
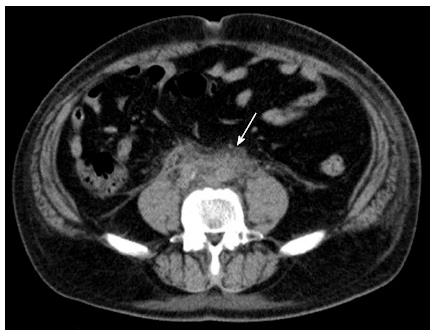
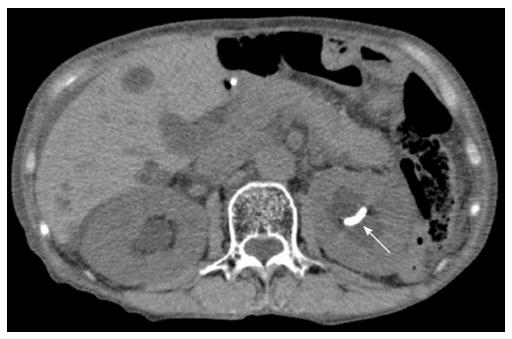
Unilateral nephrostomy needs to be considered for patients with anatomical problems in the lower urinary tract, including severe urethral stenosis and large prostatic hyperplasia; IgG4-related autoimmune pancreatitis is most frequently encountered in middle-aged to elderly men (mean age, 59-68 years, 4 to 7.5-fold higher rate compared to women)[4,7,8,17,18]. In fact, we experienced a patient (79-year-old woman) with histologically proven IgG4-related retroperitoneal fibrosis, where ureteral stenting was not sufficient to alleviate ureteral obstruction and renal failure (Figure 5). She subsequently underwent nephrostomy, followed by steroid therapy. Ureteral stents might be constricted by the severe fibrotic process around the ureter.
Figure 5 Although a ureteral stent was correctly placed into the left renal pelvis (arrow), ipsilateral hydronephrosis did not improve in a 79-year-old woman with IgG4-related retroperitoneal fibrosis.
IgG4-RELATED RETROPERITONEAL FIBROSIS MIMICKING MALIGNANCY
Abe et al[41] reported a 39-year-old man, who showed an atypical clinical manifestation. He was diagnosed with a tumor in the left ureter. He underwent segmental ureterectomy, which led to the diagnosis of an IgG4-related periureteral pseudotumor in the distal ureter. Another 75-year old man who metachronously developed IgG4-related autoimmune pancreatitis and retroperitoneal fibrosis was also reported. He initially presented with left hydronephrosis and had surgery for possible ureteral cancer, and an IgG4-related pseudotumor was histologically diagnosed. Ten months later, he was diagnosed with autoimmune pancreatitis, which was successfully managed with prednisolone[34]. These cases suggest that IgG4-related pseudotumorous retroperitoneal fibrosis is difficult to diagnose, particularly when it is the first or an isolated manifestation. Surgical resection is sometimes unavoidable for such patients.
Similar pseudotumorous lesions can develop in the more proximal urinary tract. Yoshino et al[42] encountered a 71-year-old man, who had an IgG4-related pseudotumor mimicking renal pelvic cancer in his left kidney. In this case, urine cytology obtained by a retrograde catheter in the renal pelvis was negative for malignant cells. His serum IgG4 level was found to be elevated, and he was successfully treated with prednisolone. The diagnosis of IgG4-related pseudotumorous retroperitoneal fibrosis is less difficult if patients have other organ manifestations. However, surgery has been conducted even for such patients[33], suggesting that the clinical management of patients with IgG4-related disease requires close coordination between physicians and urologists.
OTHER ASPECTS OF IgG4-RELATED RETROPERITONEAL FIBROSIS
Pipitone et al[22] suggested the utility of 18-fluorodeoxyglucose (FDG) positron emission tomography (PET) for the diagnosis and assessment of IgG4-related retroperitoneal fibrosis. This has been supported by additional studies[24,26]. On the other hand, the definite diagnosis of IgG4-related retroperitoneal fibrosis usually requires tissue confirmation, but retroperitoneal biopsies are occasionally problematic due to expected adverse events or technical failure. Sampling error is always a possibility for patients with broad plaque-like lesions. Doe et al[40] reported an interesting case: a 77-year-old man was diagnosed with IgG4-related retroperitoneal fibrosis and an elevated serum IgG4 level (398 mg/dL). Retroperitoneal biopsy was not performed because of his marked comorbidity, but lip biopsy revealed the periglandular infiltration of IgG4-positive plasma cells, leading to the diagnosis of IgG4-related disease.
ASSOCIATED CONDITIONS IN THE URINARY BLADDER
There has been no report on urinary bladder involvement in patients with proven IgG4-related disease. Crumley et al[44] retrospectively examined biopsy samples of interstitial cystitis from the aspect of IgG4. Interstitial cystitis is a clinical entity previously called painful bladder syndrome, whose etiology and pathogenesis remain undetermined[45,46]. Of 44 cases examined, 4 (9%) showed a significant increase in IgG4-positive plasma cells (greater than 30/hpf) with an IgG4/IgG ratio greater than 0.5. Those patients were characterized by an older age, severer inflammation, and smaller bladder capacity than the remaining 40 IgG4-negative patients. Serological data were not available because of the retrospective nature of the study. Further studies are necessary to conclude whether or not IgG4-related cystitis is a distinct entity.
ASSOCIATED CONDITIONS IN THE PROSTATE
Several case studies on IgG4-related prostatitis have been reported. Patients almost exclusively presented with lower urinary tract symptoms such as dysuria, pollakisuria, urinary urgency, and a feeling of incomplete emptying[9,10]. The clinical presentation is similar to that in common benign prostatic hyperplasia or chronic prostatitis[47,48]. The diagnosis of IgG4-related prostatitis may not be difficult once prostate biopsy is performed; biopsy of the prostate is an established diagnostic routine[49,50]. However, it depends on whether or not urologists, physicians, and pathologists are aware of this condition.
The first case of IgG4-related prostatitis was described in a case series of IgG4-related pancreatocholangitis reported in 2004[4]. Two years later, Yoshimura et al[9] described a 65-year-old man, in whom IgG4-related prostatitis was retrospectively diagnosed using IgG4 immunostaining 7 years after he received transurethral resection of the prostate to relieve bladder outlet obstruction. Nishimori and colleagues reported 2 additional cases[10]. Both patients were initially diagnosed with common benign prostatic hyperplasia. One patient with IgG4-related pancreatitis showed the improvement of lower urinary tract symptoms with an alpha-adrenoceptor antagonist that is the first-line agent for men with benign prostatic hyperplasia[48]. He was eventually diagnosed with IgG4-related prostatitis following prostate biopsy, which was performed because of an uptake in the prostate on FDG-PET. The other patient had isolated IgG4-related prostatitis, which was diagnosed by tissue examination of the transurethral resection specimen and elevated serum IgG4 level (473 mg/dL). Interestingly, he also showed FDG uptake in the prostate, while his pancreas was atrophic with no FDG uptake. Zaidan et al[51] reported a man with long-standing IgG4-related retroperitoneal fibrosis, who was eventually found to have IgG4-related prostatitis following prostate biopsy. The biopsy was undertaken because of a significant FDG uptake.
Uehara et al[52] histologically examined prostate tissue samples obtained from 6 cases, including one radical prostatectomy specimen. This study well addressed the histological characteristics of IgG4-related prostatitis. The histological features are basically similar to those of IgG4-related disease at other sites. Glands are replaced by the inflammatory process, consisting of lymphoplasmacytic infiltration, occasional eosinophils, and irregular fibrosis. Obliterative phlebitis was noted. IgG4-positive plasma cells were diffusely present in inflamed areas.
It is known that serum levels of prostate-specific antigen (PSA) are markedly elevated in men with bacterial prostatitis[49,50], but whether or not IgG4-related prostatitis is associated with an elevated serum PSA remains unclear because of the limited number of cases. Patel and Szostek[53] reported a man with systemic IgG4-related disease, in whom prostatic involvement was confirmed by biopsy. His serum PSA level was within the normal range. Hart et al[54] reported a 55-year-old man with IgG4-related pancreatitis and prostatitis (the PSA level was normal: 0.67 ng/mL). Interestingly, his symptoms resolved when he was given a course of oral prednisone for monoarticular gout. In our experience, patients sometimes state that corticosteroids given for IgG4-related disease at other sites relieve their lower urinary tract symptoms, which suggests that IgG4-related prostatitis may be underdiagnosed.
In 2006, Taniguchi et al[55] reported a 61-year-old man who presented with retroperitoneal and mediastinal fibrosis, and a mass in the left seminal vesicle. IgG4-related disease was diagnosed based on a high serum IgG4 concentration (583 mg/dL) and tissue examination. All lesions responded well to corticosteroids. This is probably the first reported case suggesting IgG4-related disease at this anatomical site.
In summary, men with IgG4-related pancreatitis sometimes present with IgG4-related prostatitis synchronously or metachronously. Lower urinary tract symptoms are common but not specific among elderly men. FDG-PET may be a useful diagnostic modality for IgG4-related prostatitis. Its urological features, such as efficacy of alpha-adrenoceptor antagonists for the alleviation of urinary symptoms and serum PSA elevation, remain unclear.
ASSOCIATED CONDITIONS IN THE TESTIS AND ACCESSORY ORGANS THEREOF
Bösmüller et al[11] investigated 3 men (23, 25, and 52 years old) with paratesticular fibrous pseudotumors, and suggested that this condition may be a presentation of IgG4-related disease, although information about coexisting associated conditions in other organs was not provided. Hart et al[12] subsequently reported a 67-year-old man who developed a similar condition during observation for IgG4-related autoimmune pancreatitis. Migita et al[56] reported a 74-year-old man with bilateral IgG4-related sialadenitis. He had a history of left orchiectomy for a 4-cm paratesticular mass. A retrospective review of pathological slides confirmed an inflammatory mass with the massive infiltration of IgG4-positive plasma cells. de Buy Wenniger et al[57] reported a 57-year-old man with IgG4-related pancreatitis, who was found to have IgG4-related orchitis 7 years after pancreaticoduodenectomy. His main symptom was left testicular pain, and the left testis alone was affected. Dieckmann et al[45] reported 2 young men with possible IgG4-related orchitis (28 and 18 years old). However, all four patients younger than 30 years (two cases each reported by Bösmüller et al[11] and Dieckmann et al[45]) showed no other organ involvement, which may challenge the diagnosis in young patients. Information on testicular functions such as testosterone levels and spermatogenesis was not provided in any case reports quoted in this section, and so further studies on endocrinological and functional outcomes of this rare condition are warranted.
CONCLUSION
IgG4-related autoimmune pancreatitis is frequently accompanied by relevant lesions in the retroperitoneum and genitourinary tract, leading to various clinical presentations and imaging abnormalities. Although surgical resection is occasionally unavoidable to rule out malignancy, such incidences will decrease as IgG4-related retroperitoneal fibrosis is more widely recognized and imaging findings are well characterized. We need to decide on the therapeutic plan (i.e., corticosteroids, ureteral stent) based on the renal function of patients on a case-by-case basis. Increasing evidence suggests that IgG4-related disease can affect the prostate and testis, and further studies are necessary to better understand reproductive-organ involvement of IgG4-related disease.
ACKNOWLEDGMENTS
We thank Drs. Toru Uehara, Akira Tadokoro, and Hiroo Kuroki for their contribution to the treatment of patients.
P- Reviewer: Liu ZW, Tang WF S- Editor: Qi Y L- Editor: A E- Editor: Ma S