Published online Jun 21, 2014. doi: 10.3748/wjg.v20.i23.7514
Revised: January 26, 2014
Accepted: April 8, 2014
Published online: June 21, 2014
Processing time: 193 Days and 17.6 Hours
A 25-year-old man was admitted with the chief complaints of right flank pain, watery diarrhea, and fever. Blood tests revealed high levels of inflammatory markers, and infectious enteritis was diagnosed. A stool culture obtained on admission revealed no growth of any significant pathogens. Conservative therapy was undertaken with fasting and fluid replacement. On day 2 of admission, the fever resolved, the frequency of defecation reduced, the right flank pain began to subside, and the white blood cell count started to decrease. On hospital day 4, the frequency of diarrhea decreased to approximately 5 times per day, and the right flank pain resolved. However, the patient developed epigastric pain and increased blood levels of the pancreatic enzymes. Abdominal computed tomography revealed mild pancreatic enlargement. Acute pancreatitis was diagnosed, and conservative therapy with fasting and fluid replacement was continued. A day later, the blood levels of the pancreatic enzymes peaked out. On hospital day 7, the patient passed stools with fresh blood, and Campylobacter jejuni/coli was detected by culture. Lower gastrointestinal endoscopy performed on hospital day 8 revealed diffuse aphthae extending from the terminal ileum to the entire colon. Based on the findings, pancreatitis associated with Campylobacter enteritis was diagnosed. In the present case, a possible mechanism of onset of pancreatitis was invasion of the pancreatic duct by Campylobacter and the host immune responses to Campylobacter.
Core tip: A 25-year-old man was admitted with infectious enteritis. During the hospital stay, although the symptom of enteritis was improved, the patient developed epigastric pain and increased blood levels of the pancreatic enzymes, and was diagnosed acute pancreatitis. The patient passed fresh blood stools, and Campylobacter jejuni/coli was detected by culture. Based on the findings, pancreatitis associated with Campylobacter enteritis was diagnosed. Bacteria that cause gastroenteritis can also be causative agents for pancreatitis. When upper abdominal pain or increased levels of pancreatic enzymes not consistent with the course of gastroenteritis are observed, we need to consider concomitant pancreatitis.
-
Citation: Kobayashi R, Matsumoto S, Yoshida Y. Case of acute pancreatitis associated with
Campylobacter enteritis. World J Gastroenterol 2014; 20(23): 7514-7517 - URL: https://www.wjgnet.com/1007-9327/full/v20/i23/7514.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i23.7514
Infection is one of the diverse causes of pancreatitis. Bacteria that cause gastroenteritis can also be causative agents of pancreatitis. We encountered a rare case in which acute pancreatitis occurred during the course of Campylobacter enteritis.
A 25-year-old man was admitted with a 3-d history of right flank pain and watery diarrhea. He had eaten chicken liver and steamed chicken at a restaurant 4 d earlier. On the day prior to admission, he had developed a fever of approximately 38 degrees C, and Clostridium butyricum preparations and acetaminophen had been prescribed at a neighborhood clinic. However, because of the persistence of diarrhea at a stool frequency of more than 20 times per day and fever, the patient was referred and admitted to our hospital for detailed examination. None of his friends who had eaten the same meal with him had similar symptoms.
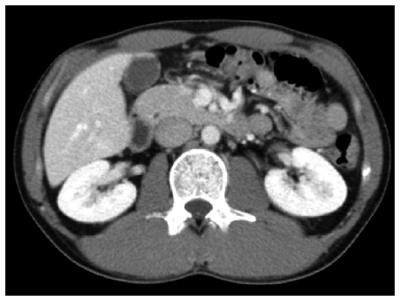
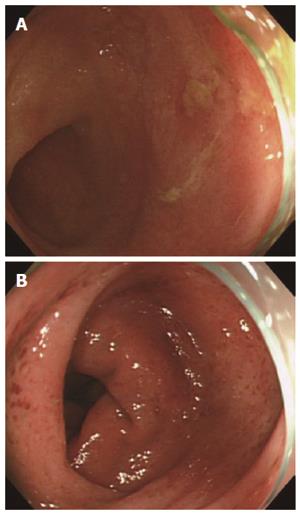
On admission, a fever of 39.1 degrees C and tenderness of the right flank were noted; however, there was no rebound tenderness or muscle guarding. The white blood cell count was elevated to 13120/μL, and the serum C-reactive protein level was increased to 11.58 (Table 1). A stool culture obtained on admission revealed no growth of any significant pathogens. As abdominal ultrasonography (US) revealed thickening of the wall of the ascending colon, infectious enteritis was diagnosed, and conservative therapy with fasting and fluid replacement was undertaken. Although no antimicrobial agent was administered, the fever resolved by day 2 of admission. The frequency of defecation and the white blood cell count began to decrease, and the right flank pain began to subside. On hospital day 4, the stool frequency decreased to approximately 5 times per day, and the right flank pain resolved completely. However, the patient developed epigastric pain. The plasma levels of pancreatic amylase and lipase were elevated to 341 IU/L and 660 IU/L, respectively (Table 2). Computed tomography (CT) revealed mild pancreatic enlargement (Figure 1). Acute pancreatitis was diagnosed, and conservative therapy with fasting and fluid replacement was continued. On the following day, the pancreatic enzyme levels peaked. On hospital day 6, oral intake was resumed. On hospital day 7, the patient passed stools containing fresh blood, and a stool culture yielded growth of Campylobacter jejuni/coli. Lower gastrointestinal endoscopy performed on hospital day 8 revealed diffuse aphthae extending from the terminal ileum to the entire colon (Figure 2). Subsequently, the bloody stools resolved, and the clinical course was favorable. The patient was discharged on hospital day 12.
| WBC | 13120/μL | γ-GTP | 25 U/L |
| Neut | 94.0% | CK | 132 U/L |
| Lymp | 1.0% | P-AMY | 24 U/L |
| Hb | 15.8 g/dL | Lipase | 660 U/L |
| Plt | 22.2 × 104/μL | CRP | 11.58 mg/dL |
| TP | 7.4 g/dL | BUN | 10 mg/dL |
| Alb | 4.5 g/dL | Cr | 1.1 mg/dL |
| T-Bil | 0.66 mg/dL | Na | 133 mmol/L |
| D-Bil | 0.21 mg/dL | K | 3.6 mmol/L |
| AST | 22 U/L | Cl | 97 mmol/L |
| ALT | 13 U/L | Tcho | 89 mg/dL |
| LD | 229 U/L | TG | 106 mg/dL |
| ALP | 222 U/L | BS | 118 mg/dL |
| WBC | 5420/μL | γ-GTP | 28 U/L |
| Neut | 76.0% | CK | 83 U/L |
| Lymp | 14.0% | P-AMY | 341 U/L |
| Hb | 14.8 g/dL | Lipase | 438 U/L |
| Plt | 27.9 × 104/μL | CRP | 4.07 mg/dL |
| TP | 7.0 g/dL | BUN | 7 mg/dL |
| Alb | 4.1 g/dL | Cr | 0.94 mg/dL |
| T-Bil | 0.52 mg/dL | Na | 134 mmol/L |
| D-Bil | 0.19 mg/dL | K | 4.0 mmol/L |
| AST | 24 U/L | Cl | 96 mmol/L |
| ALT | 16 U/L | ||
| LD | 231 U/L | ||
| ALP | 186 U/L |
Infection is one of the diverse causes of pancreatitis. Viruses that are known to cause pancreatitis include mumps virus, coxsackievirus, hepatitis B virus, cytomegalovirus, varicella-zoster virus, herpes simplex virus, and human immunodeficiency virus. The bacteria reported to cause pancreatitis include Mycoplasma, Legionella, and Leptospira species, as well as those causing gastroenteritis, such as Salmonella typhi, Campylobacter jejuni, Yersinia enterocolitica, and Yersinia pseudotuberculosis[1]. Although the mechanisms by which bacteria cause pancreatitis remain unknown, possible mechanisms include the direct spread of inflammation from adjacent organs, such as the small intestine, to the pancreas[2]; invasion of the bile duct[1] and pancreatic duct[3] by bacteria; dissemination through the blood and lymphatic vessels[1]; and immune responses of the host to bacterial invasion of the pancreas[2].
In regard to pancreatitis caused by Campylobacter enteritis, the reported age at onset ranges widely, from 9 to 88 years, and there is no gender difference. The interval from the onset of enteritis to the occurrence of pancreatitis ranges from 3 to 7 d. In terms of the severity, there are many cases of mild pancreatitis. Campylobacter enteritis has been reported to be both treated and not treated with antimicrobial agents[2-8]. However, it remains unclear whether antimicrobial agents are effective for the treatment of pancreatitis associated with Campylobacter enteritis.
In the present case, there was no apparent cause of acute pancreatitis, except for Campylobacter enteritis. The patient drank socially and was not on any regular medication. No gallstones were detected by US or CT. Additionally, there was no evidence of hypertriglyceridemia. Thin-slice CT revealed no apparent abnormalities of the pancreatobiliary junction. Even a single administration of acetaminophen can cause pancreatitis, but according to previous case reports, pancreatitis occurs within 24 h of taking the drug[9]. In our case, because pancreatitis occurred 5 d after the patient had taken acetaminophen, acetaminophen was unlikely to have been the cause of the pancreatitis. Moreover, because the levels of antinuclear antibodies and immunoglobulin G4 were within the normal range, autoimmune pancreatitis was unlikely. Thus, our patient was diagnosed as having pancreatitis associated with Campylobacter enteritis. As for the mechanism of the onset of pancreatitis in this patient, invasion of the bile duct by Campylobacter was unlikely because the blood levels of biliary enzymes were normal. CT revealed no increase in the adipose tissue around the pancreas, and the inflammatory findings around the intestine were also mild. These findings made the direct spread of the inflammation from the intestine to the pancreas also unlikely. Thus, it is assumed that invasion of the pancreatic duct by Campylobacter or an immune response of the host to invasion of the pancreas by Campylobacter was the mechanism of the onset of pancreatitis in our patient.
We encountered a rare case in which acute pancreatitis occurred during the course of Campylobacter enteritis. Bacteria that cause gastroenteritis can also be causative agents of pancreatitis. When upper abdominal pain or increased levels of pancreatic enzymes that are not consistent with the course of gastroenteritis are observed, concomitant pancreatitis needs to be kept in mind.
The patient was admitted with a 3-d history of right flank pain and watery diarrhea, and on hospital day 4, the symptom of enteritis was improved, but the patient developed epigastric pain.
Pancreatitis associated with Campylobacter enteritis was diagnosed.
There was no apparent cause of acute pancreatitis, except for Campylobacter enteritis, because the patient did not have a history of alcohol abuse or regular medication, additionally, gallstones, abnormalities of the pancreatobiliary junction, hypertriglyceridemia, and high levels of antinuclear antibodies and immunoglobulin G4 were not detected.
On admission, the plasma level of pancreatic amylase was not elevated; however, on hospital day 4, when the patient developed epigastric pain, the plasma levels of pancreatic amylase and lipase were elevated.
Lower gastrointestinal endoscopy performed on hospital day 8, which revealed diffuse aphthae extending from the terminal ileum to the entire colon.
We performed conservative therapy with fasting and fluid replacement, no antimicrobial agent was administered for either Campylobacter enteritis or acute pancreatitis.
When upper abdominal pain or increased levels of pancreatic enzymes that are not consistent with the course of gastroenteritis are observed, concomitant pancreatitis needs to be kept in mind.
This was a rare case in which acute pancreatitis occurred during the course of Campylobacter enteritis. Infection is one of the diverse causes of pancreatitis. Many viruses and bacteria can cause acute pancreatitis. But pancreatitis caused by Campylobacter enteritis was rare. So in clinical work, when upper abdominal pain or increased levels of pancreatic enzymes not consistent with the course of gastroenteritis are observed, concomitant pancreatitis needs to be considered in mind.
P- Reviewers: Fujino Y, Rocha R, Sun XD S- Editor: Ma YJ L- Editor: A E- Editor: Zhang DN
| 1. | Parenti DM, Steinberg W, Kang P. Infectious causes of acute pancreatitis. Pancreas. 1996;13:356-371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 155] [Cited by in F6Publishing: 133] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | de Bois MH, Schoemaker MC, van der Werf SD, Puylaert JB. Pancreatitis associated with Campylobacter jejuni infection: diagnosis by ultrasonography. BMJ. 1989;298:1004. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Pönkä A, Kosunen TU. Pancreas affection in association with enteritis due to Campylobacter fetus ssp. jejuni. Acta Med Scand. 1981;209:239-240. [PubMed] [Cited in This Article: ] |
| 4. | Ezpeleta C, de Ursua PR, Obregon F, Goñi F, Cisterna R. Acute pancreatitis associated with Campylobacter jejuni bacteremia. Clin Infect Dis. 1992;15:1050. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Gallagher P, Chadwick P, Jones DM, Turner L. Acute pancreatitis associated with campylobacter infection. Br J Surg. 1981;68:383. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Pitkänen T, Pönkä A, Pettersson T, Kosunen TU. Campylobacter enteritis in 188 hospitalized patients. Arch Intern Med. 1983;143:215-219. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Castilla-Higuero L, Castro-Fernandez M, Guerrero-Jimenez P. Acute pancreatitis associated with Campylobacter enteritis. Dig Dis Sci. 1989;34:961-962. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Bär BM, van Dam FE. [A patient with pancreatitis caused by Campylobacter]. Ned Tijdschr Geneeskd. 1985;129:2123-2125. [PubMed] [Cited in This Article: ] |
| 9. | Badalov N, Baradarian R, Iswara K, Li J, Steinberg W, Tenner S. Drug-induced acute pancreatitis: an evidence-based review. Clin Gastroenterol Hepatol. 2007;5:648-661; quiz 644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 348] [Cited by in F6Publishing: 350] [Article Influence: 20.6] [Reference Citation Analysis (0)] |