Published online Dec 28, 2013. doi: 10.3748/wjg.v19.i48.9405
Revised: October 5, 2013
Accepted: November 3, 2013
Published online: December 28, 2013
AIM: To investigate the usefulness of a guide wire and triple lumen needle knife for removing stones in Billroth II (B-II) gastrectomy patients.
METHODS: Endoscopic sphincterotomy in patients with B-II gastrectomy is challenging. We used a new guide wire technique involving sphincterotomy by triple lumen needle knife through a forward-viewing endoscopy. This technique was performed in nine patients between August 2010 and June 2012. Sphincterotomy as described above was performed. Adequate sphincterotomy, successful stone removal, and complications were investigated prospectively.
RESULTS: Sphincterotomy by triple lumen needle knife using guide wire was successful in all nine patients. Sphincterotomy started towards the 4-5 o’clock direction and continued to the upper margin of the papillary roof. Complete stone removal in one session was achieved in all patients. There were no procedure related complications, such as bleeding, pancreatitis, or perforation.
CONCLUSION: In patients with B-II gastrectomy, guide wire using sphincterotomy by triple lumen needle knife through a forward-viewing endoscopy seems to be an effective and safe procedure for the removal of common bile duct stones.
Core tip: Guide wire using sphincterotomy by triple lumen needle knife through a forward-viewing endoscopy seems to be a safe, easy, and effective method for removing common bile duct stones in patients with B-II gastrectomy.
- Citation: Park SB, Kim HW, Kang DH, Choi CW, Yoon KT, Cho M, Song BJ. Sphincterotomy by triple lumen needle knife using guide wire in patients with Billroth II gastrectomy. World J Gastroenterol 2013; 19(48): 9405-9409
- URL: https://www.wjgnet.com/1007-9327/full/v19/i48/9405.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i48.9405
Endoscopic sphincterotomy (EST) is essential for the endoscopic removal of common bile duct (CBD) stones. However, EST is more difficult in an altered anatomy, such as Billroth II (B-II) gastrectomy, in which the major papillae are inverted[1]. To overcome this problem, several techniques and specialized accessories have been devised, including Soehendra sphincterotome[2], Sohma sphincterotome[3], needle knife sphincterotomy guided by a biliary endoprosthesis[4,5], S-shape sphincterotome[6], and papillary balloon dilation[7,8]. These methods may be more difficult to control and frequently produce complications[5-7].
Large balloon papillary dilation after minor EST with newly developed papillotomes, such as rotatable papillotome[9] and scissors papillotome[10], has been reported for the removal of CBD stones in B-II gastrectomy. The triple lumen needle knife, which is capable of accepting a guidewire in one channel while simultaneously injecting and/or cutting in other lumens, is used primarily for precut sphincterotomy or fistulotomy in difficult cases of deep cannulation of the bile duct. These characteristics allow the simultaneously maintenance of the guide wire in CBD and sphincterotomy without the assistance of other accessories. Additionally, a guide wire positioned in the CBD can make sphincterotomy by triple lumen needle knife easier.
Herein, we detail our technique and present experiences of guide wire sphincterotomy using a triple lumen needle knife through forward-viewing endoscopy in patients with B-II gastrectomy.
From August 2010 to June 2012, endoscopic retrograde cholangiopancreatography (ERCP) for removal of CBD stones was performed on 469 patients. Of these patients, 20 with B-II gastrectomy underwent ERCP. Eleven patients who had previous EST procedures (n = 5), failure to reach major papilla (n = 4), and needle knife fistulotomy due to difficult cannulation (n = 2) were excluded. The remaining nine patients (6 men and 3 women; mean age 66.3 years) were enrolled. The same endoscopist performed all procedures. All patients provided written informed consent for their participation and the study was approved by the Institutional Review Board of Pusan National University Yansan Hospital.
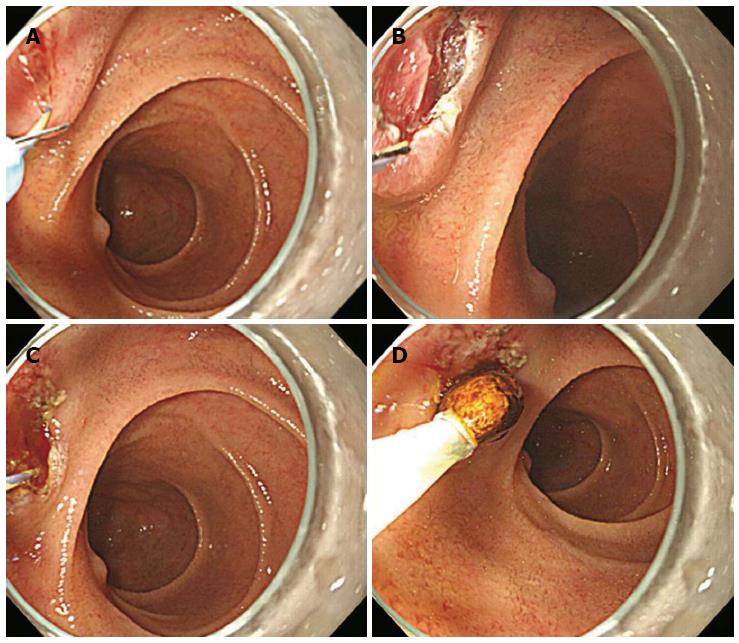
All ERCP procedures were performed under conscious sedation and coverage using prophylactic antibiotics with a model GIF-H260 cap-attached forward-viewing endoscopy apparatus (Olympus Optical, Tokyo, Japan). A transparent cap (Distal Attachments D-201-11804; Olympus) was attached to the tip of the endoscope. Selective cannulation of the CBD was achieved using a cannulation catheter with a straight tip. A 0.025-inch guide wire (Jagwire; Boston Scientific, Natick, MA) was advanced through the catheter into the CBD. The catheter was then removed, and a triple lumen needle knife (Microknife™ XL; Boston Scientific) was introduced into the major papilla over the guide wire. The needle tip was controlled with a length of 2-3 mm (Figure 1A), and sphincterotomy was performed along the guide wire as a guidance mark directed at 4-5 o’clock with sophisticated maneuver of the needle knife and endoscopy (Figure 1B). The model PSD-30 electrosurgical unit (Olympus) was used at a setting of blended one current with a power setting of 30 W/s for both the cutting and coagulation currents (cut: coagulation ratio of 3:1). During sphincterotomy, the pattern of cutting in the current method closely resembles the action of a pair of cutting scissors. Although the direction of the needle tip was toward the 1-2 o’clock direction, sphincterotomy toward the 4-5 o’clock direction was possible because the guide wire acted as a guide when the needle knife approached the bile duct pathway. At this time, the cap enabled us to perform safe and effective sphincterotomy by keeping a visual field during the procedure. After sphincterotomy to the upper margin of the papillary roof (Figure 1C), a stone retrieval basket or balloon catheter was used to extract CBD stones (Figure 1D). In cases when EST was insufficient in extracting the stone, papillary balloon dilation or mechanical lithotripsy was used in an attempt to removal the stone. To assess the efficacy and safety of this technique, we evaluated the sphincterotomy of the desired direction, use of balloon dilation or mechanical lithotripsy, successful stone removal, and complications after ERCP.
ERCP with B-II gastrectomy was performed in 20 patients by the same endoscopist. Nine patients (6 men and 3 women) underwent EST using a guide wire and triple lumen needle knife sphincterotomy. The mean age of patients was 66.3 (range, 56 -85) years. The mean size and number of stones were 7.89 (range, 5-12) and 1.78 (range, 1-4) mm, respectively (Table 1).
| Stone | ||||||||
| Patient No. | Age (yr) | Sex | Size, mm | No. | Procedure sessions | Balloon dilation (size, mm) | Stone removal | Complications |
| 1 | 63 | F | 12 | 4 | 1 | 12 | Success | None |
| 2 | 69 | M | 5 | 2 | 1 | 0 | Success | None |
| 3 | 56 | M | 6 | 2 | 1 | 0 | Success | None |
| 4 | 68 | F | 10 | 2 | 1 | 0 | Success | None |
| 5 | 67 | M | 5 | 1 | 1 | 0 | Success | None |
| 6 | 65 | M | 8 | 1 | 1 | 0 | Success | None |
| 7 | 65 | M | 10 | 1 | 1 | 0 | Success | None |
| 8 | 59 | F | 10 | 2 | 1 | 0 | Success | None |
| 9 | 85 | M | 5 | 1 | 1 | 0 | Success | None |
Sphincterotomy in the 4-5 o’clock direction and to the upper margin of the papillary roof were successful in all nine patients (100%). Complete endoscopic stone removal was achieved in a single session in all patients. Papillary balloon dilatation was performed in only one patient owing to the large CBD stones (12 mm diameter) and stenosis in the distal CBD they exhibited. No mechanical lithotripsy was performed in any patient (Table 1). Serum amylase and lipase were measured before and after the procedure (4 and 24 h, respectively). Complete blood count and a liver function test were performed the morning after the procedure. There were no complications, such as bleeding, pancreatitis, or perforation.
Diagnostic and therapeutic ERCP in patients with B-II gastrectomy can be hindered by difficulties in the identification and intubation of the afferent loop, negotiation of abrupt turns in the afferent loop, cannulation, and adequate sphincterotomy of papilla due to inverted position[11-14]. In particular, the standard pull-type sphincterotome cannot cut toward the 6 o’clock position[15,16]. To overcome this problem, several devices and techniques have been developed using the push-type papillotome, such as the Sohma[3] and Soehendra sphincterotomes[2]. These refinements allow proper orientation of the wire for the CBD and needle knife with guided techniques using a nasobiliary drain[17], cannula, or endoprosthesis[5]. However, effective push-type sphincterotomes or needle knives are, as yet, not as readily available as the standard pull-type sphincterotome.
Recently devised methods to resolve these problems rely on large balloon papillary dilation after minor EST with newly developed papillotomes[18-21], such as the rotatable papillotome[9] and scissors papillotome[10]. These methods are user-friendly, but difficult to use in performing major EST.
Another problem is the difficulty of handling the side-viewing duodenoscope through the afferent loop in a retrograde maneuver; the result is a high rate of failed procedures and serious complications that include perforation of the small bowel[22-24]. The side-viewing duodenoscope has the advantages of allowing an en-face view of papilla and an elevator to adjust the direction of accessories. However, the apparatus is not useful in B-II anastomosis and increases the risk of perforation while passing the tortuous jejunum[14] and in cases of previous jejunal enteroanastomosis (Braun’s anastomosis)[25].
This method contrasts with existing methods in three ways. First, a triple lumen needle knife was used instead of a push-type sphincterotome or rotatable papillotome. The obvious advantage of this knife is the simultaneous use of the needle knife and guide wire through the same device, which provides an indication of where and how deeply to cut, as well as avoiding blind or inappropriate cutting under direct vision of the cutting device and the presence of a clear guide. This enables a large sphincterotomy that can still be safely performed even when done by a less experienced endoscopist. Actually, sphincterotomy in all patients reached the upper margin of the papillary roof and most CBD stones were removed without papillary balloon dilatation or mechanical lithotripsy, although most were small. These findings clearly showed different results compared with other studies[9,10]. In the current study, papillary large balloon dilation was performed in one patient as a rescue method due to a large CBD stone and distal CBD stricture, but mechanical lithotripsy was not necessary. Additionally, bleeding, pancreatitis and perforation after sphincterotomy did not occur in all patients.
Secondly, conventional guide wire was used instead of nasobiliary drain, a cannula, or endoprosthesis. A guide wire already inserted in the bile duct can reduce the time of removal and subsequent reintroduction of the endoscope or insertion of a plastic stent. Also, this technique is cost-effective compared with endoprosthesis-guided sphincterotomy using a plastic stent, as a guide wire permits directed movement in the bile duct and control of the depth of incision, similar to the role of a plastic stent in endoprosthesis-guided sphincterotomy.
Thirdly, a forward-viewing endoscope was used instead of the side-viewing version. The forward-viewing endoscope in patients with Billroth II gastrectomy makes selective bile duct cannulation easier, as the endoscope and cannula are in line with the CBD[13,26]. Therefore, the lack of an elevator in forward-viewing endoscopes is only a slight disadvantage, and not a major factor in determining the success rate of cannulation and subsequence procedure. Also, a forward-viewing endoscope makes it easier to introduce the afferent loop and find the correct route, as well as making it easier to control for negotiating the acute angles of the anastomoses than side-viewing endoscope. These advantages were related with low complication rates in another study[14], and no complications, such as perforation, were noted in the current study.
Despite the several advantages of the current method, some problems remain. If the endoscopic approach to major papilla is difficult, biliary cannulation and sphincterotomy are also difficult. Therefore, for effective application of this technique, the endoscopy tip must be approached near the major papilla.
In patients with B-II gastrectomy, we do not yet know which type of sphincterotomy is superior. The several techniques and accessories each have their own drawbacks. Currently, treatment strategy guided by personal preference or level of experience with specific techniques may be necessary. Our results support the use of the guide wire and triple lumen needle knife technique previously described as one option in patients with B-II gastrectomy. The technique is especially attractive when less experienced endoscopists perform sphincterotomy in patients with B-II gastrectomy.
In conclusion, guide wire using sphincterotomy by triple lumen needle knife through a forward-viewing endoscopy seems to be a safe, easy, and effective method for removing CBD stones in patients with B-II gastrectomy. Further studies may be needed to compare the safety and efficacy of the technique in order to confirm our findings.
Endoscopic sphincterotomy is more difficult in an altered anatomy; the authors suggested a new technique by guide wire and triple lumen needle knife.
Recently introduced methods have their limitations due to their difficultly in being controlled. Guide wire technique involving sphincterotomy by triple lumen needle knife through a forward-viewing endoscopy can be used more easily.
The authors demonstrated the effectiveness and safety of removing common bile duct (CBD) stones in patients with Billroth II (B-II) gastrectomy, although those that were removed were small in size.
Guide wire using sphincterotomy by triple lumen needle knife through a forward-viewing endoscopy are a feasible and effective intervention for removing CBD stones in patients with B-II gastrectomy.
This is a clinical study to evaluate the efficiency of a new technique for removing common bile duct stones in patients with gastrectomy. This is an important and novel topic in clinics.
P- Reviewers: Csendes A, Jawad MA, Wang Z S- Editor: Zhai HH L- Editor: Rutherford A E- Editor: Liu XM
| 1. | Al-Kawas FH, Geller AJ. A new approach to sphincterotomy in patients with Billroth II gastrectomy. Gastrointest Endosc. 1996;43:253-255. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Soehendra N, Kempeneers I, Reynders-Frederix V. [A new papillotoma for the Billroth II stomach]. Dtsch Med Wochenschr. 1980;105:362-363. [PubMed] [Cited in This Article: ] |
| 3. | Rosseland AR, Osnes M, Kruse A. Endoscopic sphincterotomy (EST) in patients with Billroth II Gastrectomy. Endoscopy. 1981;13:19-24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Siegel JH, Cohen SA, Kasmin FE, Veerappan A. Stent-guided sphincterotomy. Gastrointest Endosc. 1994;40:567-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | van Buuren HR, Boender J, Nix GA, van Blankenstein M. Needle-knife sphincterotomy guided by a biliary endoprosthesis in Billroth II gastrectomy patients. Endoscopy. 1995;27:229-232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Hintze RE, Veltzke W, Adler A, Abou-Rebyeh H. Endoscopic sphincterotomy using an S-shaped sphincterotome in patients with a Billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:74-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 60] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 117] [Cited by in F6Publishing: 121] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Jang HW, Lee KJ, Jung MJ, Jung JW, Park JY, Park SW, Song SY, Chung JB, Bang S. Endoscopic papillary large balloon dilatation alone is safe and effective for the treatment of difficult choledocholithiasis in cases of Billroth II gastrectomy: a single center experience. Dig Dis Sci. 2013;58:1737-1743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Kim GH, Kang DH, Song GA, Heo J, Park CH, Ha TI, Kim KY, Lee HJ, Kim ID, Choi SH. Endoscopic removal of bile-duct stones by using a rotatable papillotome and a large-balloon dilator in patients with a Billroth II gastrectomy (with video). Gastrointest Endosc. 2008;67:1134-1138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Choi HJ, Moon JH, Ko BM, Kim YJ, Cheon YK, Cho YD, Lee MS, Shim CS. Endoscopic stone removal using a scissors papillotome followed by papillary balloon dilation in patients with Billroth II gastrectomy - a case series. Endoscopy. 2009;41:993-996. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 11. | Lin LF, Siauw CP, Ho KS, Tung JC. ERCP in post-Billroth II gastrectomy patients: emphasis on technique. Am J Gastroenterol. 1999;94:144-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Dolay K, Soylu A. Easy sphincterotomy in patients with Billroth II gastrectomy: a new technique. Turk J Gastroenterol. 2008;19:109-113. [PubMed] [Cited in This Article: ] |
| 13. | Safrany L, Neuhaus B, Portocarrero G, Krause S. Endoscopic sphincterotomy in patients with Billroth II gastrectomy. Endoscopy. 1980;12:16-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 37] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Kim MH, Lee SK, Lee MH, Myung SJ, Yoo BM, Seo DW, Min YI. Endoscopic retrograde cholangiopancreatography and needle-knife sphincterotomy in patients with Billroth II gastrectomy: a comparative study of the forward-viewing endoscope and the side-viewing duodenoscope. Endoscopy. 1997;29:82-85. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 93] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007;66:612-615. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 16. | Lee TH, Hwang JC, Choi HJ, Moon JH, Cho YD, Yoo BM, Park SH, Kim JH, Kim SJ. One-Step Transpapillary Balloon Dilation under Cap-Fitted Endoscopy without a Preceding Sphincterotomy for the Removal of Bile Duct Stones in Billroth II Gastrectomy. Gut Liver. 2012;6:113-117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Ricci E, Bertoni G, Conigliaro R, Contini S, Mortilla MG, Bedogni G. Endoscopic sphincterotomy in Billroth II patients: an improved method using a diathermic needle as sphincterotome and a nasobiliary drain as guide. Gastrointest Endosc. 1989;35:47-50. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Itoi T, Sofuni A, Itokawa F. Large dilating balloon to allow endoscope insertion for successful endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy (with video). J Hepatobiliary Pancreat Sci. 2010;17:725-728. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Itoi T, Ishii K, Itokawa F, Kurihara T, Sofuni A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010;22 Suppl 1:S98-S102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Park SY, Park CH, Yoon KW, Cho SB, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Endoscopic large-diameter balloon dilation after fistulotomy for the removal of bile duct stones in a difficult cannulation. Gastrointest Endosc. 2009;69:955-959. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Choi CW, Choi JS, Kang DH, Kim BG, Kim HW, Park SB, Yoon KT, Cho M. Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol. 2012;27:256-260. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Gregl A, Schaal HJ, Müller I, Peiper HJ. [Mammography in the diagnosis and treatment of non-puerperal mastitis (author’s transl)]. Rofo. 1979;130:342-347. [PubMed] [Cited in This Article: ] |
| 23. | Wilkinson ML, Engelman JL, Hanson PJ. Intestinal perforation after ERCP in Billroth II partial gastrectomy. Gastrointest Endosc. 1994;40:389-390. [PubMed] [Cited in This Article: ] |
| 24. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 105] [Cited by in F6Publishing: 118] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 84] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Fujita K, Myojo S, Yoshida S, Kawase Y. Endoscopic sphincterotomy using a pull-type sphincterotome with an attached stabilizer in patients with Billroth II gastrectomy. Endoscopy. 2011;43 Suppl 2 UCTN:E47-E48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |