Published online Dec 21, 2012. doi: 10.3748/wjg.v18.i47.7127
Revised: October 29, 2012
Accepted: November 6, 2012
Published online: December 21, 2012
Gastric intramural hematoma is a rare injury of the stomach, and is most often seen in patients with underlying disease. Such injury following endoscopic therapy is even rarer, and there are no universally accepted guidelines for its treatment. In this case report, we describe a gastric intramural hematoma which occurred within 6 h of endoscopic mucosal resection (EMR). Past medical history of this patient was negative, and laboratory examinations revealed normal coagulation profiles and platelet count. Following EMR, the patient experienced severe epigastric pain and vomited 150 mL of gastric contents which were bright red in color. Subsequent emergency endoscopy showed a 4 cm × 5 cm diverticulum-like defect in the anterior gastric antrum wall and a 4 cm × 8 cm intramural hematoma adjacent to the endoscopic submucosal dissection lesion. Following unsatisfactory temporary conservative management, the patient was treated surgically and made a complete recovery. Retrospectively, one possible reason for the patient’s condition is that the arterioles in the submucosa or muscularis may have been damaged during deep and massive submucosal injection. Thus, endoscopists should be aware of this potential complication and improve the level of surgery, especially the skills required for submucosal injection.
- Citation: Sun P, Tan SY, Liao GH. Gastric intramural hematoma accompanied by severe epigastric pain and hematemesis after endoscopic mucosal resection. World J Gastroenterol 2012; 18(47): 7127-7130
- URL: https://www.wjgnet.com/1007-9327/full/v18/i47/7127.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i47.7127
Gastric intramural hematoma is an uncommon disorder. Previously reported cases were caused by coagulopathy, trauma, aneurysm, peptic ulcer disease, pancreatitis, endoscopic therapy or spontaneous hematomas[1-3]. However, gastric intramural hematoma after endoscopic intervention is even rarer. Here, we describe a gastric intramural hematoma accompanied by severe epigastric pain and hematemesis which occurred within 6 h of endoscopic mucosal resection (EMR).
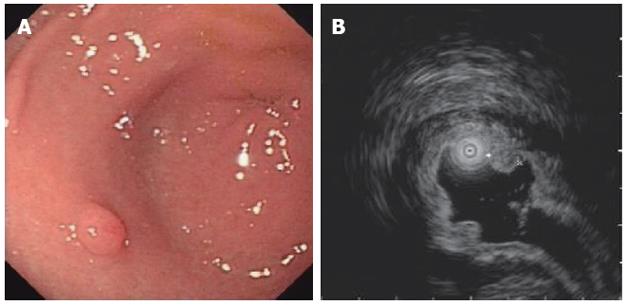
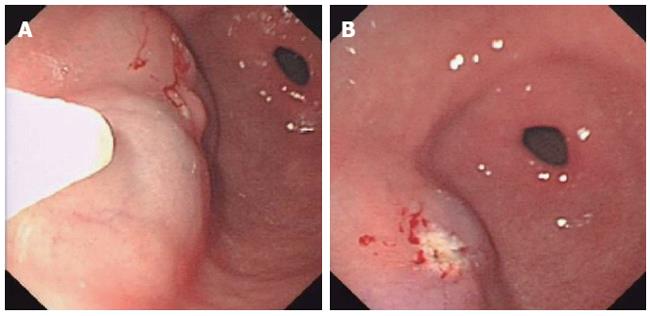
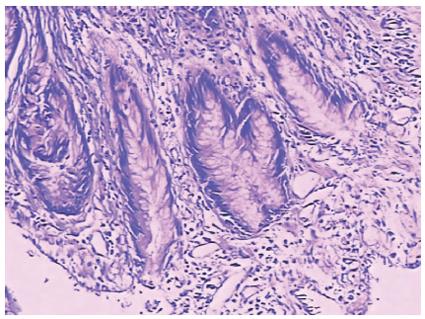
A 33-year-old man had dull epigastric pain for 3 mo, and endoscopy showed a 0.4 cm × 0.5 cm polypoid protrusive lesion in the stomach antrum (Figure 1A). He was admitted for endoscopic treatment. He had no noteworthy medical history, and laboratory examinations showed the following: white blood cell count 8.14 × 109/L, hemoglobin 151 g/L, platelet count 206 × 109/L, prothrombin time 9.8 s, and activated partial thromboplastin time 26.7 s. Endoscopic ultrasonography showed that the lesion was localized in the mucosal layer (Figure 1B). Following discussion with the patient and his wife, EMR was carried out. He was given a submucosal 5-mL saline injection, and the nidus was not uplifted satisfactorily. The operator then slowly injected another 10 mL saline into the distal lesion until the result was satisfactory (Figure 2A). The lesion was successfully removed by high-frequency electrocoagulation, and a white wound was observed (Figure 2B). The removed lesion was sent for pathologic examination which later revealed tubular adenoma and negative Helicobacter pylori infection (Figure 3). The patient’s condition was stable after surgery. He received 40 mg omeprazole intravenously, and walked into the ward.
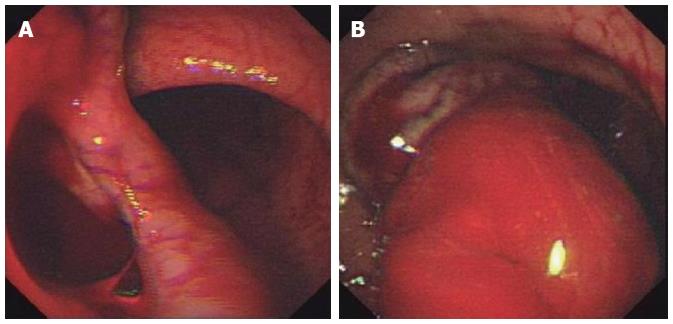
Half an hour after surgery, the patient experienced sudden persistent epigastric pain and paroxysmal colic without nausea or vomiting. He received an injection of anisodamine. Bedside ultrasonography of the abdomen did not reveal any apparent abnormalities, and the levels of serum lipase and amylase were normal. Although his pain was slightly reduced, he continued to have intermittent upper abdominal pain. Two hours later, he vomited 150 mL of gastric contents which were bright red in color. After vomiting, his epigastric pain was slightly reduced, and his vital signs were stable. Emergency plain film of the abdomen (KUB) did not reveal radiological evidence of a perforated viscus, and emergency endoscopy showed a 4 cm × 5 cm diverticulum-like defect (Figure 4A) on the anterior gastric antrum wall, there was also a 4 cm × 8 cm intramural hematoma on the greater curvature side of the lower gastric body adjacent to the EMR wound, and active bleeding was observed (Figure 4B). Gastrointestinal decompression was performed. After 4 h observation, the patient still had intense paroxysmal pain, and 100 mL of blood was drained from the stomach. He underwent emergency laparotomy under endoscopic guidance, and approximately 300 mL intragastric blood was found. There was a 4 cm × 5 cm × 8 cm intramural hematoma on the distal anterior gastric wall, and the gastric wall was intact with no evidence of perforation. An incision was made in the gastric wall, and the hematoma in the stomach and gastric wall was evacuated manually. The area of suspicious bleeding in the gastric wall was sutured, and no source of active bleeding was identified. The operators sutured the EMR wound, and a subhepatic drain was inserted.
Recovery was uneventful and the patient was allowed oral intake three days after surgery. There was no evidence of gastric leak upon commencing diet, and the subhepatic drain was removed one week later. The patient was well at discharge. At the one-year follow-up, he was well and without complications.
Recently, EMR and endoscopic submucosal dissection (ESD) have been widely used. The most common complications of these endoscopic techniques are bleeding and perforation. Intraoperative and postoperative gastric intramural hematomas are clinically rare. EMR and ESD have been used in our hospital for 5 years, and this is the first case of postoperative gastric intramural hematoma. To date, there is only one reported case of intraoperative gastric intramural hematoma, which occurred during ESD[4].
The pathological changes related to hematoma are damaged vessels and blood is confined to the space around the vessels. In previously reported cases, gastric intramural hematomas can result from coagulopathy, trauma, aneurysm, peptic ulcer disease, pancreatitis, repeated vomiting or spontaneous hematomas[1,2]. However, the past medical history of our patient was entirely negative, and laboratory examinations showed normal coagulation profiles and platelet count.
It is well known that there are few blood vessels in the gastric mucosal layer, while the submucosa and muscularis contain many blood vessels. Before lesion excision, ESD or EMR operators should inject hypertonic saline mixed with methylene blue around the lesion, to lift the lesion and completely separate the mucosal layer and muscularis. Thus, the wound would be confined to the submucosa, the muscularis would not be damaged, and complications would be very infrequent. In our case, the probable reasons for gastric intramural hematoma were that the very deep submucosal injection (retrospectively, lifting of the mucosal layer was slightly unsatisfactory, and the muscularis may have been injected), massive submucosal injection (15 mL), and arterioles in the submucosa or muscularis may have been damaged during submucosal injection. The blood from the damaged arterioles was confined between the submucosa and muscularis and formed a hematoma. As the hematoma grew, the mucosal layer was torn and the patient experienced epigastric pain. As the pressure increased, blood entered the gastric cavity from the EMR wound, and the patient vomited bright red gastric contents.
There is no established standard therapy for gastric intramural hematoma. In previous reports, most patients recovered following conservative management; however, surgery or arterial embolization may be necessary, depending on the patient’s status[1,3]. Although there was no radiographic evidence of perforation in our patient, he had severe epigastric pain and vomited blood. In order to avoid serious complications, a laparotomy was selected instead of conservative treatment in this patient.
Reported cases of gastrointestinal intramural hematoma following endoscopic procedures are very few and mostly confined to the esophagus[5]. This type of gastric intramural hematoma is extremely rare, however, several authors have reported the incidence of gastric intramural hematoma following endoscopic therapy[3,4,6]. Gastric intramural hematoma is dangerous, and can cause misery for the sufferer. When carrying out endoscopic procedures, endoscopists should be aware of this potential complication. In addition, endoscopists should improve the level of surgery, especially the skills required for submucosal injection.
Peer reviewer: Fauze Maluf-Filho, MD, Hospital das Clínicas, São Paulo University School of Medicine, 488 Olegario Mariano, São Paulo 05359, Brazil
S- Editor Song XX L- Editor A E- Editor Zhang DN
| 1. | Imaizumi H, Mitsuhashi T, Hirata M, Aizaki T, Nishimaki H, Soma K, Ohwada T, Saigenji K. A giant intramural gastric hematoma successfully treated by transcatheter arterial embolization. Intern Med. 2000;39:231-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Dhawan V, Mohamed A, Fedorak RN. Gastric intramural hematoma: a case report and literature review. Can J Gastroenterol. 2009;23:19-22. [PubMed] [Cited in This Article: ] |
| 3. | Keum B, Chun HJ, Seo YS, Kim YS, Jeen YT, Lee HS, Um SH, Kim CD, Ryu HS. Gastric intramural hematoma caused by argon plasma coagulation: treated with endoscopic incision and drainage (with videos). Gastrointest Endosc. 2012;75:918-919. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Yang CW, Yen HH. Large gastric intramural hematoma: unusual complication of endoscopic submucosal dissection. Endoscopy. 2011;43 Suppl 2 UCTN:E240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Lukman MR, Jasmi AY, Niza SS. Massive dissecting intramural duodenal haematoma following endoscopic haemostasis of a bleeding duodenal ulcer. Asian J Surg. 2006;29:98-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Sadio A, Peixoto P, Cancela E, Castanheira A, Marques V, Ministro P, Silva A, Caldas A. Intramural hematoma: a rare complication of endoscopic injection therapy for bleeding peptic ulcers. Endoscopy. 2011;43 Suppl 2 UCTN:E141-E142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |