Published online Dec 7, 2012. doi: 10.3748/wjg.v18.i45.6686
Revised: September 3, 2012
Accepted: September 12, 2012
Published online: December 7, 2012
Sister Mary Joseph’s nodule (SMJN) refers to a metastatic tumor of the umbilicus. It is a rare entity which arises from a malignancy in the intra-abdominal cavity. We herein describe a patient who presented with SMJN as his first sign of pancreatic cancer. It is an even more unusual case of SMJN. We therefore, suggest that pancreatic cancer should be included in the differential diagnosis when an umbilical mass is found. With the progress made in surgical procedures and other modalities, an early diagnosis will dramatically improve the prognosis of the patients.
- Citation: Bai XL, Zhang Q, Masood W, Masood N, Tang Y, Cao CH, Fu QH, Zhang Y, Gao SL, Liang TB. Sister Mary Joseph’s nodule as a first sign of pancreatic cancer. World J Gastroenterol 2012; 18(45): 6686-6689
- URL: https://www.wjgnet.com/1007-9327/full/v18/i45/6686.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i45.6686
Umbilical tumors are rare and 30% of them are metastatic[1]. Sister Mary Joseph’s nodule (SMJN) refers to a metastatic lesion of the umbilicus originating from intra-abdominal or pelvic malignant diseases. The most common primary sites of the metastasis are stomach, ovaries, colon, rectum and pancreas. Pancreas accounts for 7%-9% of the SMJN cases[2]. Almost 90% of the cases arise from the body and tail of the pancreas, but not the head[2].
We herein describe a male patient with pancreatic cancer who presented with SMJN as his first clinical sign. We also reviewed the published literatures on this disease from PubMed. Only 20 cases (including our case) of SMJN with pancreatic cancer as the first symptom and sign have been reported in English. The aim of this report is to provide new insight into the identification of pancreatic cancer presenting as SMJN.
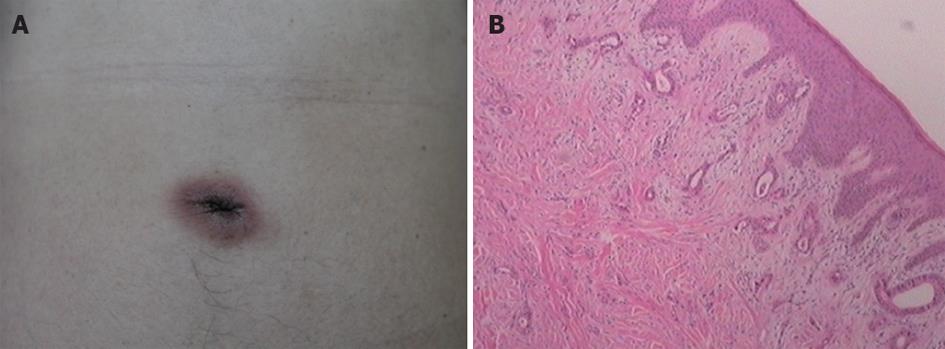
The patient is a 40-year-old man who presented with swelling, redness and induration at umbilicus. The patient was first diagnosed with eczema at a local hospital and was treated without improvement. After six months, the patient consulted a dermatologist at our hospital. Physical examination showed an inflamed umbilicus with a nodule of 2 cm × 1.5 cm without ulcer (Figure 1A). An umbilical skin biopsy was taken and sent for pathologic examination. The pathology was suggestive of adenocarcinoma infiltrating dermis and epidermis (Figure 1B). Immunohistochemistry (IHC) showed cytokeratin (CK) (AE1/AE3) +++, carcinoembryonic antigen +++, and CK7 +. A metastatic adenocarcinoma was suspected based on all these findings.
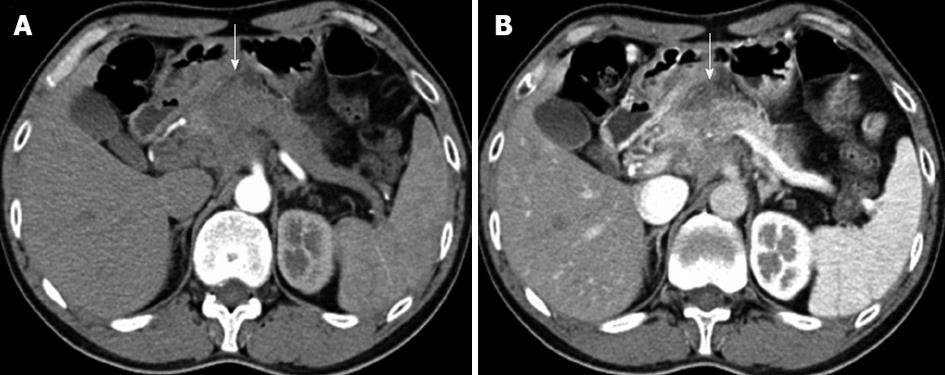
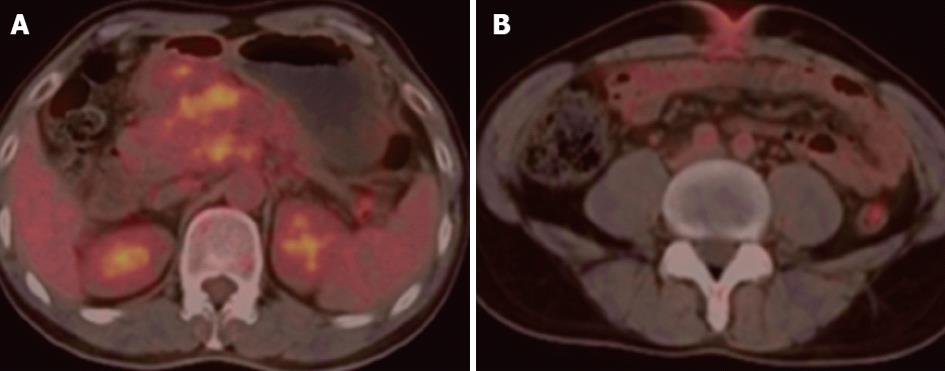
Serum marker of carbohydrate antigen 19-9 (CA19-9) was elevated (202.1 U/mL). Other tumor markers were all in the normal range. An abdominal multi-detector computed tomography (MDCT) revealed a tumor at the neck of the pancreas with retroperitoneal lymph nodes enlargement as well as an umbilical soft tissue mass (Figure 2). An abdominal computed tomography (CT) angiography also showed involvement of retroperitoneal lymph nodes, superior mesenteric artery and vein, celiac trunk, proximal splenic artery, splenic vein and part of portal vein. A fluorodeoxyglucose (FDG) positron emission tomography-CT (PET-CT) scan demonstrated a mass located at the neck and body of pancreas with increased FDG uptake, with a maximal standardized uptake value (SUV) of 3.69, and thus malignancy was suspected. The umbilical mass with a maximal SUV of 2.85 was also detected and a metastatic malignancy was diagnosed by PET-CT (Figure 3).
Preoperative abdominal CT angiography showed the tumor encasing celiac trunk and superior mesenteric artery, which, however, did not cause the occlusion or the stricture of theses arteries. According to our previous experience, the patient may still have a chance of resection. An exploratory laparotomy was then performed. Mild abdominal ascites was present. A hard mass of 8 cm at the neck and body of pancreas was discovered, with invasion of celiac trunk, superior mesenteric artery, superior mesenteric vein and portal vein. Several enlarged mesenteric lymph nodes and an umbilical mass of 2 cm × 1.5 cm as well as tiny diffused seeding nodules were observed. Diaphragmatic tumor invasion was visible. A biopsy was taken and a frozen section was sent for pathology. Adenocarcinoma infiltrating the striated diaphragmatic muscle tissues was confirmed. Surgical resection was abandoned because of distant metastasis of the cancer. The patient refused chemotherapy, and died four months later.
When a clinician observes an umbilical mass, his/her differential diagnosis should include both benign and malignant tumors. Benign tumors can be caused by a number of factors, including polyps, papilloma, myoma, fibroma, hemangioma, dermoid cyst, teratoma, pyogenic granuloma, omphalith, or endometriosis[1]. Malignant lesions account for 38% of all umbilical tumors, including both primary and secondary cancers[1]. These can be differentiated by means of biopsy collection and histopathological examination[3]. Cytology can not distinguish between primary and secondary malignancies[4].
The incidence of metastatic tumor originating from intra-abdominal malignancy to the umbilicus (SMJN) is very low. The most common primary sites of SMJN in men are stomach, followed by colon, rectum, pancreas and others[3]. In women, the most common origins are the ovaries, followed by stomach, colon, rectum, pancreas and others[2]. Pancreas is the fourth or fifth most common primary site of SMJN. The percentage of SMJN arising from pancreas ranges from 7% to 9%, among which SMJN presenting as the first sign of pancreatic cancer is even unusual[2,5]. To our knowledge after literature review, only 20 such cases, including our case, have been reported in English[6-11].
The metastatic routes of the pancreatic cancer to the umbilicus are thought to be by direct invasion from the peritoneum, through lymphatic or blood vessels and along embryonic remnants[6]. Generally, the prognosis of pancreatic cancer with SMJN is poor. The mean survival is 6-11 mo[6]. However, with early diagnosis and surgical intervention, a prolonged survival of 18 years was reported[6]. Currently, with the improvement of surgery, the resection rate of advanced pancreatic cancer has been increased. Moreover, with advances made in multidiscipline therapeutical modalities including chemotherapy, radiotherapy, targeted molecular therapy, immunotherapy, and others, the survival of the patients has also been improved.
It has been reported that resection of SMJN and the primary cancer of pancreas combined with other therapeutic modalities has improved the prognosis of the patients[9]. Therefore, an appropriate diagnostic algorithm is very important for early detection and rational treatment.
As mentioned above, for patients with umbilical nodules as the first clinical manifestation, biopsy should be performed first if the diagnosis is uncertain[3,4]. Almost all the cases of SMJN from pancreatic cancer reported in the literature are adenocarcinomas[4]. IHC staining for CK 7 and 19 are very important in diagnosing adenocarcinomas of pancreas[5]. Serum tumor markers such as CA19-9 should be examined and elevation of CA19-9 is considered as a strong evidence of the disease. Once SMJN deriving from pancreatic cancer is suspected, contrast-enhanced MDCT or magnetic resonance imaging (MRI) on pancreas should be done. Contrast-enhanced MDCT or MRI is sensitive enough to display the pancreas mass and its involvement in the adjacent organs and vessels. PET-CT is also recommended to detect other distant metastasis[12,13]. However, PET-CT is not sensitive to the identification of tiny seeding nodules in the intra-abdominal cavity. As in this case, PET-CT failed to display intra-abdominal diffusion.
An earlier diagnosis could have caught the tumor in its early phase, hence improving the prognosis of the patient. This paper is to remind physicians and surgeons of the importance of keeping in mind pancreatic cancer as one of their initial differential diagnosis when an umbilical nodule is presented. The recommended diagnostic algorithm is hopefully useful for the early detection of pancreatic cancer which appears as SMJN as its first sign.
Peer reviewers: Ji Kon Ryu, Professor, Department of Internal Medicine, Seoul National University College of Medicine, 28 Yeongeon-dong, Jongno-gu, Seoul 110-744, South Korea; Andrada Seicean, MD, PhD, Third Medical Clinic Cluj Napoca, University of Medicine and Pharmacy Cluj Napoca, 15 Closca Street, 400039 Cluj-Napoca, Romania
S- Editor Gou SX L- Editor A E- Editor Li JY
| 1. | Barrow MV. Metastatic tumors of the umbilicus. J Chronic Dis. 1966;19:1113-1117. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 88] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Yendluri V, Centeno B, Springett GM. Pancreatic cancer presenting as a Sister Mary Joseph's nodule: case report and update of the literature. Pancreas. 2007;34:161-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D. Umbilical metastasis or Sister Mary Joseph’s nodule. Int J Dermatol. 1998;37:7-13. [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 90] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 4. | Zhang Y, Selvaggi SM. Metastatic islet cell carcinoma to the umbilicus: diagnosis by fine-needle aspiration. Diagn Cytopathol. 2003;29:91-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Jun DW, Lee OY, Park CK, Choi HS, Yoon BC, Lee MH, Lee DH. Cutaneous metastases of pancreatic carcinoma as a first clinical manifestation. Korean J Intern Med. 2005;20:260-263. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Tokai H, Matsuo S, Azuma T, Haraguchi M, Yamaguchi S, Kanematsu T. Pancreatic cancer with umbilical metastasis (Sister Mary Joseph’s Nodule). Acta Med Nagasaki. 2005;50:123-126. [Cited in This Article: ] |
| 7. | Miyahara M, Hamanaka Y, Kawabata A, Sato Y, Tanaka A, Yamamoto A, Ueno T, Nishihara K, Suzuki T. Cutaneous metastases from pancreatic cancer. Int J Pancreatol. 1996;20:127-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Crescentini F, Deutsch F, Sobrado CW, Araújo S. Umbilical mass as the sole presenting symptom of pancreatic cancer: a case report. Rev Hosp Clin Fac Med Sao Paulo. 2004;59:198-202. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Ozaki N, Takamori H, Baba H. Sister Mary Joseph's nodule derived from pancreatic cancer. J Hepatobiliary Pancreat Sci. 2011;18:119-121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Limmathurotsakul D, Rerknimitr P, Korkij W, Noppakun N, Kullavanijaya P, Rerknimitr R. Metastatic mucinous cystic adenocarcinoma of the pancreas presenting as Sister Mary Joseph's nodule. JOP. 2007;8:344-349. [PubMed] [Cited in This Article: ] |
| 11. | Pranjali K, Prabhash K, Karanth VN, Kane S, Nair R, Parikh PM. Umbilical metastasis: an unusual presentation of pancreatic adenocarcinoma. Indian J Dermatol Venereol Leprol. 2007;73:199-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 12. | Pakzad F, Groves AM, Ell PJ. The role of positron emission tomography in the management of pancreatic cancer. Semin Nucl Med. 2006;36:248-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Kauhanen SP, Komar G, Seppänen MP, Dean KI, Minn HR, Kajander SA, Rinta-Kiikka I, Alanen K, Borra RJ, Puolakkainen PA. A prospective diagnostic accuracy study of 18F-fluorodeoxyglucose positron emission tomography/computed tomography, multidetector row computed tomography, and magnetic resonance imaging in primary diagnosis and staging of pancreatic cancer. Ann Surg. 2009;250:957-963. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 232] [Cited by in F6Publishing: 209] [Article Influence: 14.9] [Reference Citation Analysis (0)] |