Published online Jun 21, 2012. doi: 10.3748/wjg.v18.i23.2973
Revised: September 26, 2011
Accepted: February 27, 2012
Published online: June 21, 2012
AIM: To investigate the effectiveness of head compensatory postures to ensure safe oropharyngeal transit.
METHODS: A total of 321 dysphagia patients were enrolled and assessed with videofluoromanometry (VFM). The dysphagia patients were classified as follows: safe transit; penetration without aspiration; aspiration before, during or after swallowing; multiple aspirations and no transit. The patients with aspiration or no transit were tested with VFM to determine whether compensatory postures could correct their swallowing disorder.
RESULTS: VFM revealed penetration without aspiration in 71 patients (22.1%); aspiration before swallowing in 17 patients (5.3%); aspiration during swallowing in 32 patients (10%); aspiration after swallowing in 21 patients (6.5%); multiple aspirations in six patients (1.9%); no transit in five patients (1.6%); and safe transit in 169 patients (52.6%). Compensatory postures guaranteed a safe transit in 66/75 (88%) patients with aspiration or no transit. A chin-down posture achieved a safe swallow in 42/75 (56%) patients, a head-turned posture in 19/75 (25.3%) and a hyperextended head posture in 5/75 (6.7%). The compensatory postures were not effective in 9/75 (12%) cases.
CONCLUSION: VFM allows the speech-language the-rapist to choose the most effective compensatory posture without a trial-and-error process and check the effectiveness of the posture.
- Citation: Solazzo A, Monaco L, Del Vecchio L, Tamburrini S, Iacobellis F, Berritto D, Pizza NL, Reginelli A, Di Martino N, Grassi R. Investigation of compensatory postures with videofluoromanometry in dysphagia patients. World J Gastroenterol 2012; 18(23): 2973-2978
- URL: https://www.wjgnet.com/1007-9327/full/v18/i23/2973.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i23.2973
Swallowing is a coordinated activity that enables solids and liquids to pass uninterrupted from the mouth to the stomach. Dysphagia occurs when this process is altered by organic or functional alterations at the level of swallow initiation or esophageal emptying[1].
Oropharyngeal dysphagia can manifest as one or more symptoms that are specific for oropharyngeal dysfunction, which help the clinician distinguish it from esophageal dysphagia. Typical symptoms include the inability to chew, a delayed or absent swallow initiation, a bolus delay located in the neck, nasal regurgitation, a need to swallow repeatedly to clear food or fluid from the pharynx, coughing after aspiration, and dysphonia[2,3].
Oropharyngeal dysphagia is usually a manifestation of a systemic disease rather than a disease specific to the oropharynx. This manifestation occurs in one-third of all stroke patients and has a 20%-50% prevalence in conditions such as Parkinson’s disease, Alzheimer’s disease, and amyotrophic lateral sclerosis[3-5].
Videofluoroscopy (VFS) is the gold standard in the study of oropharyngeal dysphagia because it provides information on the presence and severity of the major categories of dysfunction, including the presence, timing and severity of aspiration[6,7].
Videofluoromanometry (VFM) correlates fluoroscopic events with manometric data. For example, the narrow upper esophageal sphincter (UES) opening can be distinguished from uncoordinated UES relaxation, and the weak propulsive pharyngeal forces can be distinguished from an increased outflow resistance. Moreover, VFM is especially useful for subsequent treatment planning[2].
Characterization of a swallowing disorder allows the patient to adopt compensatory swallowing postures, change their diet to permit safe oral feeding, and delay the use of percutaneous endoscopic gastrostomy in degenerative diseases[8]. The aim of our study was to evaluate the effectiveness of compensatory postures to ensure safe oropharyngeal transit with videofluoromanometric guidance.
From January 2008 to December 2010, 321 dysphagia patients (171 male, 150 female, aged 18-87 years, mean age: 57 years) were enrolled in this study. All patients gave their written consent. The past medical history, present symptoms, and alimentary status were obtained from all patients. All patients underwent a morphofunctional logopedic evaluation according to recent guidelines[9,10].
Through the VFM assessment, the dysphagia patients were classified as follows: safe transit; penetration without aspiration; aspiration before, during, or after swallowing; multiple aspirations and no transit. The patients with aspiration or no transit were investigated to determine whether compensatory postures could correct the swallowing disorder. Based on manometric data, a chin-down posture, head-turned posture or hyperextended head posture was tested to obtain safe swallowing. Patients with multiple aspirations were excluded from the search for compensatory postures. These patients, who are often in an advanced disease stage, do not follow the operator commands during the VFM assessment and do not co-operatively assume the compensatory postures. Additionally, these subjects may only somewhat benefit from these compensatory postures[11]. The VFM study consisted of a parallel execution of VFS and manometry. A simultaneous manometric evaluation analyzed the tongue base pressure (the contact pressure between the posterior tongue thrust and the pharyngeal wall), UES tone (resting pressure, contraction pressure and residual pressure) and the bolus transit coordination, which are useful for selecting the compensatory postures[12,13] (Table 1).
| Normal values measured with VFM | |
| Tongue base pressure | 130 ± 70 mmHg |
| UES | |
| Resting pressure | 90 ± 30 mmHg |
| Contraction pressure | 240 ± 80 mmHg |
| Residual pressure | < 10 mmHg |
| Relaxation duration | 1.5 ± 0.4 s |
| Bolus progression | > 4 cm/s |
| Pharyngeal pressure | 60 ± 20 mmHg |
A Dyno Compact computerized system (MENFIS Biomedica s.r.l., Bologna, Italy) was used. This system was equipped with the following: (1) A graphics card for managing radiographic images; and (2) AVIUS-dedicated software, which enables digital-quality recording (PAL/NTSC, composite video or S-video) of the VFS study in AVI format with a 320 × 240 resolution and 25 Hz acquisition frequency. The delay introduced by the image digitization process was approximately 200 ms; therefore, for analytical purposes, the images could be considered synchronized with the manometric recordings. The concurrent pressure measurements were performed with a manometry catheter with endoluminal five-channel, solid-state microtransducers 2 cm apart at an angle of 120°-90°. The catheter was inserted through the nasal cavity into the stomach. The value recorded was used for the calibration of 0. Afterwards, a pull through was performed and the catheter was withdrawn to allow for the positioning of the transducers. Transducer 1 was placed at Passavant’s ridge to evaluate the correct closure of the rhinopharynx during swallowing and phonation. Transducers 2, 3 and 4 were placed in the pharynx. Transducer 5 was placed at the UES, and the correct placement was determined by the appearance of the characteristic M wave. During image acquisition, the video images and manometric trace were displayed in real time as a full screen image on the personal computer monitor. A cursor indicated the exact correspondence between the video images and the traces. Following the acquisition, the video and manometric trace could be analyzed during real-time reproduction or at reduced or increased speed, or it could be paused for a frame-by-frame analysis. The examinations were acquired with the patient standing or seated if the patient was unable to remain standing.
VFM began with a baseline evaluation (without contrast) to study the motility of the vocal chords and soft palate. The VFM proceeded with barium contrast medium (Prontobario HD suspension, Bracco SpA, Milan; 250% w/v) at a dose of 5-15 mL that was optimized for the patient to evaluate swallowing, with particular attention paid to aspiration. This was made possible by previous evaluation by a speech therapist. The patients were asked to hold the bolus in their mouth for several seconds and to swallow when asked by the operator. All phases of the process were video-recorded first in the anteroposterior and then the laterolateral view[9,14]. If an impaired bolus transit or aspiration in the airways was detected, an evaluation of the ideal bolus size and monitoring the effectiveness of the compensatory postures were used to investigate correcting the dysfunction.
The compensatory posture was selected for each patient based on the specific swallowing dysfunction that was considered to have caused the aspiration. For an effective oropharyngeal bolus transit while swallowing, the following compensatory postures were tested. The chin-down posture involved tucking the chin to the neck. The change in head position inverted the epiglottis into a more protective position over the airway entry, which reduced the airway entrance space and increased the size of the vallecular spaces[12,15,16]. The head-turned posture narrowed the ipsilateral piriform sinus and sent the bolus to the contralateral sinus. In addition, it determined the decrease in UES pressure, delayed its closure during swallowing, and optimized the bolus propulsion[17,18]. The hyperextended head posture facilitated the bolus transit using the force of gravity. This posture is indicated for reduced pharyngeal peristalsis[4].
VFM in 169 (52.6%) of 321 enrolled patients showed safe transit of the contrast medium. In 71/321 cases (22.1%), penetration of the contrast medium into the laryngeal lumen without aspiration below the glottic level was observed, and we did not suggest compensatory postures for these patients. In 5/321 (1.5%) cases, there was no transit.
In 76/321 patients (23.7%), aspiration was observed. In 70/76 (92.1%) patients, VFM revealed a single aspiration, and in 17/70 (24.3%) cases, aspiration occurred before swallowing, in 32/70 (45.7%) during swallowing, and in 21/70 (30%) after swallowing. In 6/76 cases (7.9%), there were multiple aspirations, and compensatory postures were not sought in these patients.
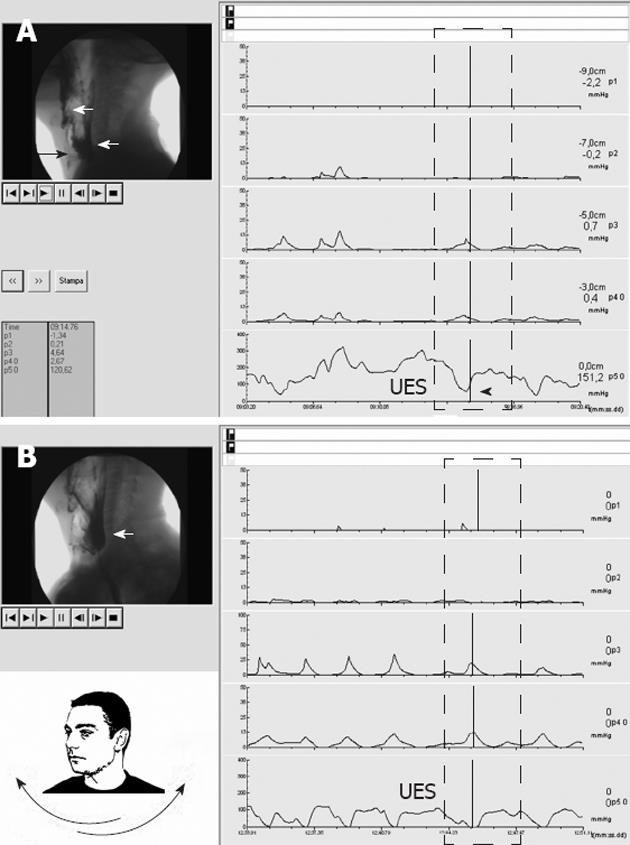
Compensatory postures (Figures 1 and 2) through VFM guidance were tested in the 70 patients with a single aspiration and the five with no transit (Table 2). Among the aspiration cases, 24 (34%) had no spontaneous reflex cough. The 17 patients with aspiration before swallowing suffered from disorders of the oral phase, such as a deficit of lip closure (17.6%), reduced lifting of the soft palate (41.2%), and reduced (29.4%) or disorganized tongue movement (11.8%). The tongue-palate contact was incomplete in 4/17 (23.5%), with leakage and aspiration before voluntary swallowing due to a fraction of the bolus moving into the pharynx and being aspired without manometric alterations. In 8/17 cases (47%), the manometric evaluation showed that the tongue base pressure was < 60 mmHg during swallowing. In all 17 patients, a total resolution of the disorder was obtained by adopting the chin-down posture.
| ALS | Stroke | MS | PD | Post-surgery | AD | Others | Total | |
| Safe transit | 41 | 21 | 22 | 28 | 3 | 14 | 40 | 169 |
| Penetration without aspiration | 22 | 14 | 8 | 10 | - | 7 | 10 | 71 |
| Aspiration before swallowing | 4 | 5 | 1 | 3 | 1 | 3 | - | 17 |
| Aspiration during swallowing | 12 | 5 | 3 | 5 | 4 | 3 | - | 32 |
| Aspiration after swallowing | 10 | 2 | 2 | 3 | 2 | 2 | - | 21 |
| Multiple aspirations | 4 | - | - | - | - | 2 | - | 6 |
| No transit | 1 | - | - | 2 | - | 2 | - | 5 |
| Total | 94 | 47 | 36 | 51 | 10 | 33 | 50 | 321 |
Aspiration during swallowing occurred in 32 (45.7%) cases. Eighteen of these (56.3%) were related to a reduced laryngeal closure (10/32) or elevation (8/32), and 14 were related to a UES disorder, with a residual pressure during relaxation of > 10 mmHg (9/14, 28.1%) and an early closure of the UES compared to the end of the pharyngeal contraction (5/14, 15.6%).
In 14/18 (78%) patients with reduced laryngeal closure or elevation, the chin-down posture (Figure 2) resolved the aspiration, whereas in 10/14 (71%) patients with UES disorders, the aspiration was corrected with the head-turned posture.
The compensatory postures were not effective in 8/32 (25%) patients. In the 21 cases of aspiration after swallowing, the bolus was inhaled due to stagnant contrast medium in the pharynx. The contrast medium was noted in 5/21 (23.8%) cases at the piriform sinuses, in 4/21 (19.1%) at the glossoepiglottic valleys, and in 12 (57.1%) at both locations. Aspiration after swallowing in 4/21 (19.1%) cases resulted from incomplete release of the UES, with a residual pressure of > 10 mmHg. In 4/21 (19.1%) cases, the resting pressure of the UES was > 150 mmHg. In 1/21 (4.8%) cases, the pharyngeal dysfunction and stagnation of contrast medium was unilateral. The chin-down posture solved the aspiration in 11/21 cases (52.4%), and the head-turned posture was useful in 9/21 patients (42.9%). In 1/21 (4.7%) cases, there was no discomfort reduction.
In the five cases of dysphagia with no transit, the disorder was characterized by alterations in the initiation of the swallowing reflex without a peristaltic wave from the tongue base; all of these cases benefited from the hyperextended head posture (Table 3).
| ALS | Stroke | MS | PD | Post-surgery | AD | Others | Total | |
| Swallowing disorders | ||||||||
| Aspiration before swallowing | 4 | 5 | 1 | 3 | 1 | 3 | - | 17 |
| Aspiration during swallowing | 12 | 5 | 3 | 5 | 4 | 3 | - | 32 |
| Aspiration after swallowing | 10 | 2 | 2 | 3 | 2 | 2 | - | 21 |
| No transit | 1 | - | - | 2 | - | 2 | - | 5 |
| Compensation postures | ||||||||
| Chin down | 13 | 6 | 5 | 6 | 5 | 7 | 0 | 42 |
| Head turned | 10 | 4 | 1 | 3 | 0 | 1 | 0 | 19 |
| Head hyperextended | 1 | 0 | 0 | 2 | 0 | 2 | 0 | 5 |
| No compensation | 3 | 2 | 0 | 2 | 2 | 0 | 0 | 9 |
Swallowing therapy has the primary goal of maintaining oral feeding and achieving safe and efficient swallowing, which is important to ensure a good quality of life. Different swallowing techniques have been adopted rapidly during the past decade and are used almost worldwide. However, few studies have investigated how each technique affects swallowing[13,15,19].
When treating patients with oropharyngeal dysfunction, an ideal approach to the assessment and treatment is working in a team with a radiologist, gastroenterologist and a speech-language pathologist. In the present study, a multi-specialist assessment team evaluated each enrolled patient to assess the swallowing dysfunction and test the adequacy of therapy to ensure safe transit. VFM provides a parallel acquisition of videofluoroscopic and manometric data and plays a crucial role in therapeutic planning.
We did not employ dietary modifications, including increases in the volume or density of food, for radioprotection reasons, but a single bolus of contrast medium was optimized for the patient.
Three different compensatory postures, including chin down, head turned and head hyperextended, were adopted. Each patient was tested before the posture was deemed appropriate. The compensatory postures restored a safe transit in 66/75 patients (88%). The chin-down posture was effective in 42/66 patients (63.6%). This posture was useful in all patients with aspiration before swallowing because it promoted bolus control in the oral cavity until the swallowing reflex was elicited. In patients with aspiration during swallowing and reduced laryngeal closure or elevation, the chin-down posture protected the airway from aspiration. In patients with aspiration after swallowing, dropping the tongue base and the contrast medium stasis in the pharynx fostered the bolus flow into the esophagus.
The head-turned posture was useful in 19/66 (28.8%) patients with both aspiration during swallowing and aspiration after swallowing with a residual pressure or uncoordinated UES relaxation due to the decrease in UES pressure and increase in UES opening time. This posture was useful also in one patient with stroke and unilateral pharyngeal failure because it excluded the affected side from the bolus transit.
The hyperextended head posture was effective in all five patients without transit. This posture uses gravity to aid swallowing; therefore, this posture is recommended for all cases with impaired lingual propulsion but should be suggested only after verifying that the transit occurs safely[4].
The compensatory postures were not effective in 9/75 patients (12%). This finding was related to a massive aspiration in 3/9 cases, poor compliance due to an advanced stage of disease in 4/9 cases, and surgery in 2/9 cases.
Silent aspiration, defined as aspiration in the absence of reflex cough, should also be mentioned. This event occurred in 24/70 (34.3%) patients with a single aspiration; specifically, three with aspiration before swallowing, 10 during swallowing, and 11 after swallowing. In other studies, this phenomenon occurred in approximately half of those patients who aspirated and was significantly more frequent in those with a history of laryngeal pathology[20].
Silent aspiration has major importance[21] because it promotes the early onset of complications, such as aspiration pneumonia. Aspiration pneumonia is three times more frequent in dysphagia patients than those without[22], and is the most common cause of death in patients with neurological disorders associated with dysphagia[23].
The present study had some limitations, including the use of an intraluminal manometric catheter, which is considered a non-altering device for swallowing, and the poor availability and high cost of this imaging method.
Compared to other studies[13,15], this study included the largest number of patients. The effectiveness of the compensatory postures in the oropharyngeal dysphagia patients was evaluated with combined videofluorography and manometry. In our experience, manometry has extensively evaluated deglutition disorders. Consequently, this method has chosen the better posture and defined the more effective therapeutic strategy.
In conclusion, there is not a single compensatory posture for each type of aspiration. Only VFM accurately defines the pathogenic mechanism of the swallowing deficit; helps the speech-language therapist choose the most effective compensation posture without a trial-and-error process; and checks the effectiveness at the same time. The chin-down, head-turned and head hyperextension postures are efficacious in several swallowing disorders. These postures can be evaluated during the examination itself, are easy to learn, and ensure good patient compliance. This study, complemented by a professional treatment team, guarantees a more accurate diagnosis and greater therapeutic efficacy than the individual modalities for evaluating dysphagia patients.
Choking, aspiration pneumonia, malnutrition and dehydration can complicate dysphagia. An exact characterization of the pathogenetic mechanisms of dysphagia helps define the therapeutic approach to reduce the risk of complications.
Videofluoromanometry (VFM) is the gold standard for swallowing studies and analyzing the mechanisms underlying dysphagia.
There is not a single compensatory posture for each type of aspiration. Only VFM accurately defines the pathogenic mechanism of the swallowing deficit; helps the speech-language therapist choose the most effective compensation posture without a trial-and-error process; and checks the effectiveness at the same time.
VFM explores the effectiveness of the compensatory postures. This method may help manage dysphagia.
This is a novel approach for the assessment of swallowing and the anatomy and physiology of the laryngopharyngeal segment. The authors seem to know the radiological aspects of the subject.
Peer reviewer: Richard A Awad, Professor, Experimental Medicine and Motility Unit, Mexico City General Hospital, Dr. Balmis 148, Mexico DF 06726, Mexico
S- Editor Cheng JX L- Editor Kerr C E- Editor Li JY
| 1. | Merlo A, Cohen S. Swallowing disorders. Annu Rev Med. 1988;39:17-28. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 2. | Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116:455-478. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 349] [Cited by in F6Publishing: 285] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 3. | Cook IJ. Oropharyngeal dysphagia. Gastroenterol Clin North Am. 2009;38:411-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 104] [Cited by in F6Publishing: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | Rofes L, Arreola V, Romea M, Palomera E, Almirall J, Cabré M, Serra-Prat M, Clavé P. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol Motil. 2010;22:851-858, e230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 181] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 5. | Eslick GD, Talley NJ. Dysphagia: epidemiology, risk factors and impact on quality of life--a population-based study. Aliment Pharmacol Ther. 2008;27:971-979. [PubMed] [Cited in This Article: ] |
| 6. | Lo Re G, Galia M, La Grutta L, Russo S, Runza G, Taibbi A, D'Agostino T, Lo Greco V, Bartolotta TV, Midiri M. Digital cineradiographic study of swallowing in patients with amyotrophic lateral sclerosis. Radiol Med. 2007;112:1173-1187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 165] [Cited by in F6Publishing: 168] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 7. | Barbiera F, Condello S, De Palo A, Todaro D, Mandracchia C, De Cicco D. Role of videofluorography swallow study in management of dysphagia in neurologically compromised patients. Radiol Med. 2006;111:818-827. [PubMed] [Cited in This Article: ] |
| 8. | Available from: http//: www.sinpe.it. [Cited in This Article: ] |
| 9. | Cappabianca S, Reginelli A, Monaco L, Del Vecchio L, Di Martino N, Grassi R. Combined videofluoroscopy and manometry in the diagnosis of oropharyngeal dysphagia: examination technique and preliminary experience. Radiol Med. 2008;113:923-940. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Available from: http//: www.asha.org. [Cited in This Article: ] |
| 11. | Ohmae Y, Karaho T, Hanyu Y, Murase Y, Kitahara S, Inouye T. [Effect of posture strategies on preventing aspiration]. Nihon Jibiinkoka Gakkai Kaiho. 1997;100:220-226. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Bülow M, Olsson R, Ekberg O. Supraglottic swallow, effortful swallow, and chin tuck did not alter hypopharyngeal intrabolus pressure in patients with pharyngeal dysfunction. Dysphagia. 2002;17:197-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 63] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Olsson R, Castell JA, Castell DO, Ekberg O. Solid-state computerized manometry improves diagnostic yield in pharyngeal dysphagia: simultaneous videoradiography and manometry in dysphagia patients with normal barium swallows. Abdom Imaging. 1995;20:230-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Solazzo A, Del Vecchio L, Reginelli A, Monaco L, Sagnelli A, Monsorrò M, Di Martino N, Tedeschi G, Grassi R. Search for compensation postures with videofluoromanometric investigation in dysphagic patients affected by amyotrophic lateral sclerosis. Radiol Med. 2011;116:1083-1094. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Rasley A, Logemann JA, Kahrilas PJ, Rademaker AW, Pauloski BR, Dodds WJ. Prevention of barium aspiration during videofluoroscopic swallowing studies: value of change in posture. AJR Am J Roentgenol. 1993;160:1005-1009. [PubMed] [Cited in This Article: ] |
| 16. | Baylow HE, Goldfarb R, Taveira CH, Steinberg RS. Accuracy of clinical judgment of the chin-down posture for dysphagia during the clinical/bedside assessment as corroborated by videofluoroscopy in adults with acute stroke. Dysphagia. 2009;24:423-433. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Logemann JA, Kahrilas PJ, Kobara M, Vakil NB. The benefit of head rotation on pharyngoesophageal dysphagia. Arch Phys Med Rehabil. 1989;70:767-771. [PubMed] [Cited in This Article: ] |
| 18. | Nagaya M, Kachi T, Yamada T, Igata A. Videofluorographic study of swallowing in Parkinson's disease. Dysphagia. 1998;13:95-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 130] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Logemann JA. Dysphagia: evaluation and treatment. Folia Phoniatr Logop. 1995;47:140-164. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 86] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Lundy DS, Smith C, Colangelo L, Sullivan PA, Logemann JA, Lazarus CL, Newman LA, Murry T, Lombard L, Gaziano J. Aspiration: cause and implications. Otolaryngol Head Neck Surg. 1999;120:474-478. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 85] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Ramsey D, Smithard D, Kalra L. Silent aspiration: what do we know? Dysphagia. 2005;20:218-225. [PubMed] [Cited in This Article: ] |
| 22. | Available from: http//: www.spread.it. [Cited in This Article: ] |
| 23. | Restivo DA. La disfagia nelle malattie neurologiche: anatomia, fisiopatologia e diagnostica clinico-strumentale. Neurovegetativo News. 2007;7:1-7. [Cited in This Article: ] |