Copyright
©2011 Baishideng Publishing Group Co.
World J Gastroenterol. Dec 21, 2011; 17(47): 5150-5155
Published online Dec 21, 2011. doi: 10.3748/wjg.v17.i47.5150
Published online Dec 21, 2011. doi: 10.3748/wjg.v17.i47.5150
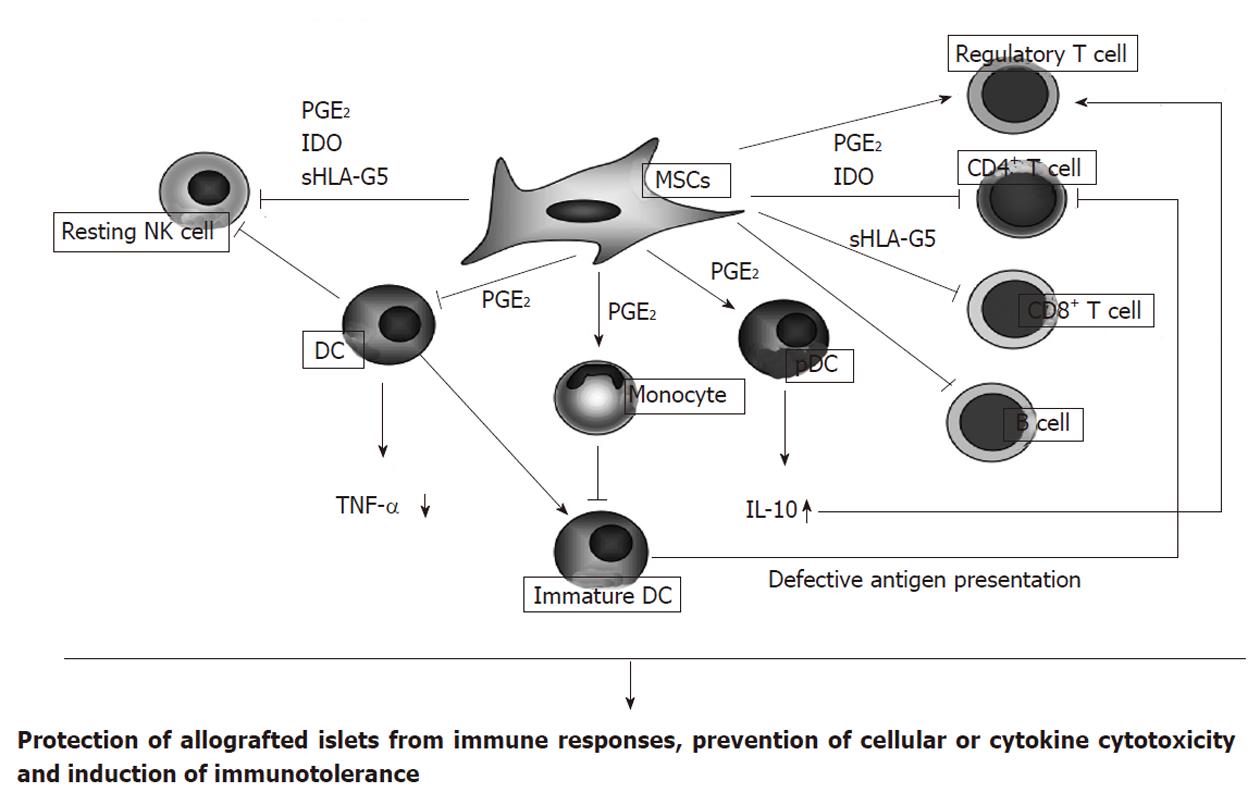
Figure 1 Immunomodulatory effect of mesenchymal stem cells (modified and quoted from Uccelli et al[13]).
Mesenchymal stem cells (MSCs) can inhibit the proliferation and cytotoxicity of resting natural killer (NK) cells via the generation of mediators, including prostaglandin E2 (PGE2), indoleamine 2,3-dioxygenase (IDO) and soluble human leukocyte antigen (sHLA)-G5; MSCs inhibit the differentiation of monocyte to antigen presenting dendritic cells (DCs). MSCs also inhibit TNF-α production by DCs and upregulate IL-10 production by plasmacytoid DCs (pDCs): effects modulated by PGE2; MSCs directly inhibit CD4+ T cell, CD8+ T cell, and B cells that are involved in allogeneic cell rejection by releasing PGE2, IDO, or sHLA-G5. CD4+ T cell inhibition limits B cell proliferation and antibody production whilst CD8+ T cell inhibition prevents cytotoxicity. MSCs induce generation of immunomodulatory regulatory T cells that suppress immune activation, help to maintain homeostasis, and promote self tolerance by production of IL-10 from pDCs and by releasing HLA-G5. Thus, MSCs can promote immunotolerance and facilitate the engraftment of allogeneic islets.
- Citation: Sakata N, Goto M, Yoshimatsu G, Egawa S, Unno M. Utility of co-transplanting mesenchymal stem cells in islet transplantation. World J Gastroenterol 2011; 17(47): 5150-5155
- URL: https://www.wjgnet.com/1007-9327/full/v17/i47/5150.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i47.5150