Published online Jul 28, 2011. doi: 10.3748/wjg.v17.i28.3359
Revised: November 15, 2010
Accepted: November 22, 2010
Published online: July 28, 2011
AIM: To determine whether the outcomes of laparoscopic fenestration (LF) were superior to open fenestration (OF) for congenital liver cysts.
METHODS: Comparative studies published between January 1991 and May 2010 on Medline (Ovid), Emsco, PubMed, Science Direct; Cochrane Reviews; CNKI; Chinese Biomedical Database, VIP and other electronic databases were searched. Randomized controlled trials (RCTs) and retrospective case-control studies on the management of congenital hepatic cysts were collected according to the pre-determined eligibility criteria to establish a literature database. Retrieval was ended in May 2010. Meta-analysis was performed using RevMan 5.0 software (Cochrane library).
RESULTS: Nine retrospective case-control studies involving 657 patients, comparing LF with OF were included for the final pooled analysis. The meta-analysis results showed less operative time [mean difference (MD): -28.76, 95% CI: -31.03 to 26.49, P < 0.00001]; shorter hospital stay (MD: -3.35, 95% CI: -4.46 to -2.24, P < 0.00001); less intraoperative blood loss (MD: -40.18, 95% CI: -52.54 to -27.82, P < 0.00001); earlier return to regular diet (MD: -29.19, 95% CI: -30.65 to -27.72, P < 0.00001) and activities after operation (MD: -21.85, 95% CI: -31.18 to -12.51, P < 0.0001) in LF group; there was no significant difference between the two groups in postoperative complications (odds ratio: 0.99, 95% CI: 0.41 to 2.38, P = 0.98) and cysts recurrence rates.
CONCLUSION: The short-term outcomes of LF for patients with congenital hepatic cysts were superior to open approach, but its long-term outcomes should be verified by further RCTs and extended follow-up.
- Citation: Qiu JG, Wu H, Jiang H, Huang JW, Pankaj P, Xu YL, Wang JZ, Zeng Y. Laparoscopic fenestration vs open fenestration in patients with congenital hepatic cysts: A meta-analysis. World J Gastroenterol 2011; 17(28): 3359-3365
- URL: https://www.wjgnet.com/1007-9327/full/v17/i28/3359.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i28.3359
Hepatic cysts can be divided into two general categories: congenital and acquired. The congenital hepatic cyst has an identifiable epithelium on histological examination, while acquired liver cysts generally arise from post -traumatic hematoma and spontaneous intrahepatic infarction or infection. In the past, hepatic cysts were often discovered at laparotomy, but at present it can be recognized due to increased use of imaging modalities and radiographic studies such as ultrasonography, computer tomography and magnetic resonance imaging.
Hepatic cysts were a more common benign liver disease, many are asymptomatic without any particular intervention, only about 16% of cysts are symptomatic[1]. The symptoms caused by a hepatic cyst are related to the size and location of the cyst. Abdominal pain and abdominal distension are the most frequent complaints and are present in more than 50% of the patients[2]. Other less common complaints include nausea, vomiting, fatigue, and jaundice. Only those with symptoms or infection require surgical treatment.
Before the advent of laparoscopy, open fenestration (OF) was regarded as the most popular method for symptomatic liver cysts. However, with the development of minimally invasive surgery and increasingly wide acceptance for laparoscopy approach in abdominal diseases, the laparoscopic fenestration (LF) has become one of the main management for hepatic cyst[3-5]. Although the use of laparoscopic approach produced some uncertain factors, such as the influence on the cardiorespiratory function caused by the increased abdominal pressure, which increased the incidence of hypertension, arrhythmia, cardiac arrest, pulmonary edema, mediastinal emphysema, pneumothorax and so on[6,7]. Cabon diaoxide gas used for this procedure is hazardous for pulmonary-compromised patients. However, successful practice and satisfactory outcome have been reported about the advantages of laparoscopy[8-10], although these reports were about the experiences from a single center. Therefore, we conducted a systematic review and comprehensive analysis of the relevant literatures about the treatment of hepatic cysts to evaluate the outcomes of patients undergoing LF vs OF.
A search of randomized controlled trials (RCTs) or retrospective case-control studies that compared laparoscopic with OF for patients with congenital hepatic cysts was performed, no matter with or without blinding and concealment of allocation. Retrospective case-control studies and case-reports were included besides RCTs. The number of patients included in all the studies was ≥ 15. All articles should be published in English or Chinese.
Eligibility criteria for all included studies were: (1) explicitly reporting the indications for LF and OF; (2) reporting at least one of the measured outcomes mentioned as follows; (3) comparing the outcomes of LF and OF in patients with congenital hepatic cysts; (4) when two studies were published by the same institution or authors, either one of the higher quality or the most recent article was included; and (5) patients with parasitic liver cysts, liver cancer and intrahepatic bile duct dilation cysts and other cystic diseases were excluded.
Studies were excluded from the analysis if (1) it was impossible to extract the appropriate data from the published articles; (2) there was considerable overlap between authors, institutes, or patients in the published literatures; (3) the measured outcomes were not clearly presented in the literatures; and (4) the laparoscopic and open surgery were performed for other diseases which were companied with liver cysts.
The following outcomes were used to compare LF and OF: (1) operative time; (2) hospital stay; (3) intraoperative blood loss; (4) the time to return to normal diet; (5) the time to return to activities; (6) the incidence of postoperative complications; (7) hospitalization cost; (8) the recurrence rate of hepatic cysts; (9) the time to return to normal liver functions; and (10) the recurrence rate of symptoms.
Both an internet based search and a manual search were used to acquire relevant studies. First, eight electronic databases (Medline; Emsco; PubMed; Science Direct; Cochrane Reviews; Chinese Biomedical Database; CNKI; and VIP) were searched and articles published between January 1991 and May 2010 were collected. The following Mesh search headings were used: ”laparoscopy”, “open fenestration”, “congenital hepatic cysts”, “comparative study” and “systematic review”, and their combinations or similar headings were also searched such as “laparoscopic fenestration”, “minimally invasive surgery”, and “Meta-analysis”. Second, further articles were identified by a manual search of reference lists from retrieved publications. The databases were used again to retrieve the abstracts, and if favorable, the full-text was downloaded for the final review.
Two reviewers independently screened the title and abstract of each publication for this study. Citations with suspected compliance with our eligibility criteria underwent a full review. If either of the two reviewers identified a citation to be potentially relevant, we obtained the full-text article for a full review. The two reviewers independently determined the eligibility of all included publications for a full text evaluation in the screening process, and disagreements were resolved through discussions by the two reviewers, and when this did not resolve the differences, a third person made a final decision on the eligibility of the study.
The following descriptive data from all eligible studies were abstracted by two reviewers independently: authors, methodology, study period, interventions used, participant characteristics, and the measured outcomes. And disagreements were resolved using the same consensus process mentioned above. We also contacted the authors of all eligible studies if there were missing data or inaccurate information.
Meta-analysis was performed in line with recommendations from the Cochrane Collaboration. Heterogeneity was assessed at first using a random-effect model, P < 0.10 as statistically significant heterogeneity. Statistical analysis of continuous variables was carried out using mean difference (MD) as the summary statistics by the Inverse-Variance method, while dichotomous variables were analyzed using odds ratio (OR) by the Mantel-Haenszel method, and both were reported with 95% CI. The MD and OR were considered to be statistically significant at P < 0.05 if the 95% CI did not include the value “1”. OR was defined as the odds of an adverse event occurring in the LF group compared with the OF group, while MDs represent the differences between the two groups in the continuous variables.
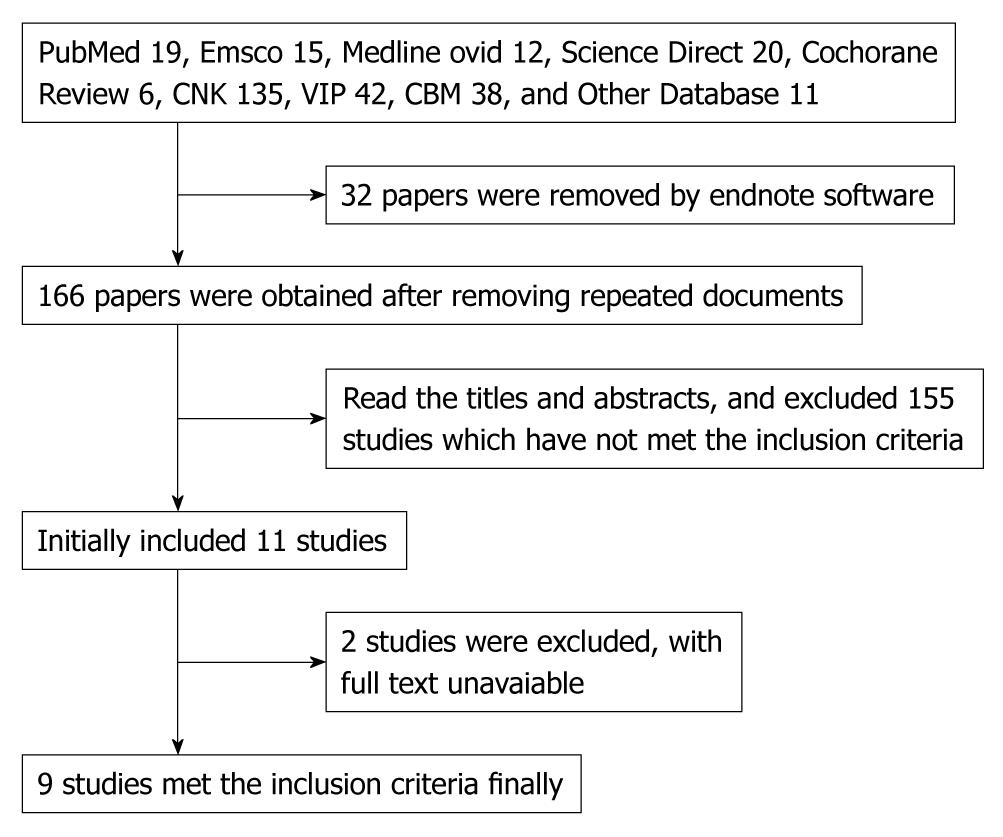
According to the literature searching strategies, 9 case-control studies, involving a total of 657 cases that compared the outcomes of LF with OF in patients with congenital liver cyst, were identified for pooled analysis, including six studies[11-16] published in Chinese and three[17-19] in English. The quality of all included studies was moderate to poor. The specific literature screening process is shown in Figure 1. The general characteristics and methodological quality assessments of all included studies are summarized in Tables 1 and 2.
| Included studies | Design types | Patients | Age (yr) | Gender (M/F) | Site (left/right/bilobar) | Cyst size (cm) | Cyst types (single/multiple/polycystic) | Main complaints | Measured outcomes | ||||||
| OF | LF | OF | LF | OF | LF | OF | LF | OF | LF | OF | LF | ||||
| Yi et al[11] | N-RCT | 117 | 52 | 45 ± 12.8 | 43 ± 9.2 | 43/74 | 21/32 | 21/58/ND | 16/22/ 0 | 9.5 ± 3.4 | 8.9 ± 4.6 | 79/38/ 37 | 38/14/ 11 | A, B, C, D | 1-4, 6, 9 |
| Felizardo et al[12] | N-RCT | 34 | 37 | 52.6 ± 21.8 | 51.1 ± 20.3 | 13/21 | 17/20 | 05/17/ 12 | 04/16/ 17 | 12.8 ± 6.3 | 114 ± 6.7 | 20/14/ND | 19/18/ND | A, B, C, D | 1-3, 4, 8 |
| Chen et al[13] | N-RCT | 19 | 17 | 44.2 | 41.1 | 23/13 | ND | ND | ND | ND | ND | ND | A, B, C, D | 1, 2, 3, 7 | |
| Qiu et al[14] | N-RCT | 29 | 22 | ND | ND | 22/29 | ND | ND | ND | ND | ND | ND | A, B, C, D | 1-5, 7 | |
| Li et al[15] | N-RCT | 40 | 46 | 18-83 (45) | ND | ND | ND | ND | ND | ND | ND | A, B, C, D | 3, 4, 5 | ||
| Guo et al[16] | N-RCT | 27 | 31 | 42 ± 11.2 | 45 ± 9.8 | 09/18 | 12/19 | 08/11/ND | 09/13/ND | 8.4 ± 4.7 | 9.9 ± 5.8 | 19/18/ 21 | 09/09/ 09 | A, B, C | 1-3, 6, 7 |
| Mazza et al[17] | N-RCT | 37 | 66 | 19-87 (62.5) | ND | ND | ND | ND | ND | 24/13/ND | 46/20/ND | A, B, C, D | 3, 4, 5 | ||
| Gigot et al[18] | N-RCT | 5 | 19 | 45 | 57 | 05/0 | 18/01 | 01/04/0 | 12/05/02 | 7-17 (10) | 8-30 (13) | 03/02/0 | 10/06/03 | A, B, C, D | 3, 4 |
| Treckmann et al[19] | N-RCT | 17 | 42 | 28-86 (62) | 07/52 | 05/08/04 | 25/09/08 | 6-20 (11.2) | 6-18 (10.8) | 11/03/ND | 38/04/ND | A, B, C, D | 1, 4, 5 | ||
| Included studies | Allocation method | Homogeneity analysis | Identification of prognostic factors | Control of bias |
| Yi et al[11] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age, sex, cyst location, types, size | No |
| Felizardo et al[12] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age cyst location, size, type | No |
| Chen et al[13] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age, sex, clinical complaints | No |
| Qiu et al[14] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Sex, main clinical complaints | No |
| Li et al[15] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age, cyst location, type, size | No |
| Guo et al[16] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age, sex, cyst location, type, size | No |
| Mazza et al[17] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Reported the age, cyst type, main complaints | No |
| Gigot et al[18] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age, sex, cyst location, type, size | No |
| Treckmann et al[19] | By doctors and patients | All the included cases come from the same research center, with good homogeneity | Age, sex, cyst location , type, size | No |
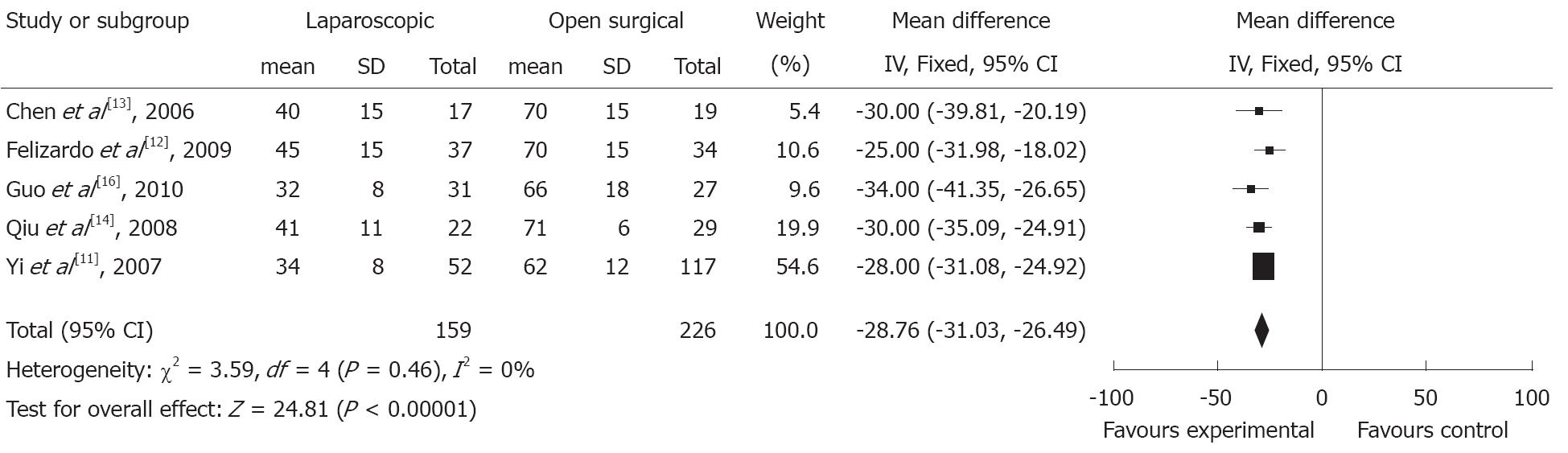
Operative time: Six studies[11-14,16,19] reported on the operative time, but one study[19] did not provide sufficient information in mean ± SD, so meta-analysis of five studies indicates that the operative time was significantly shorter in LF group than in OF group (MD: -28.76, 95% CI: -31.03 to -26.49, P < 0.00001). But this finding was not associated with significant heterogeneity between studies (P = 0.46, I2 = 0%) (Figure 2).
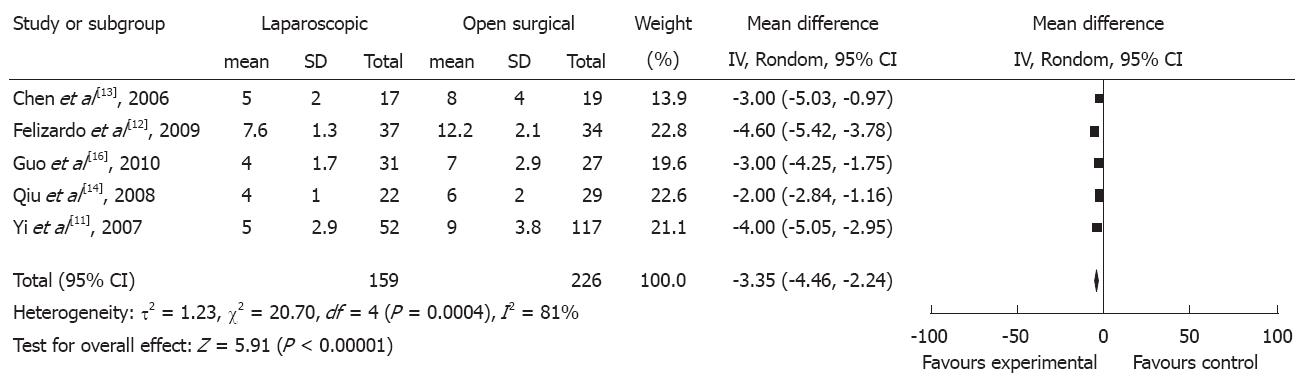
Hospital stay: Eight studies[11-18] reported on the duration of postoperative hospitalization, but three[16-18] of them did not provide specific time data. Meta-analysis of the remaining five studies indicates that the hospital stay is significantly shorter in the LF group than in the OF group (MD: -3.35, 95% CI: -4.46 to -2.24, P < 0.0001) and there is statistically significant heterogeneity between the groups in all available studies for pooled analysis (P = 0.0004, I2 = 81%) (Figure 3).
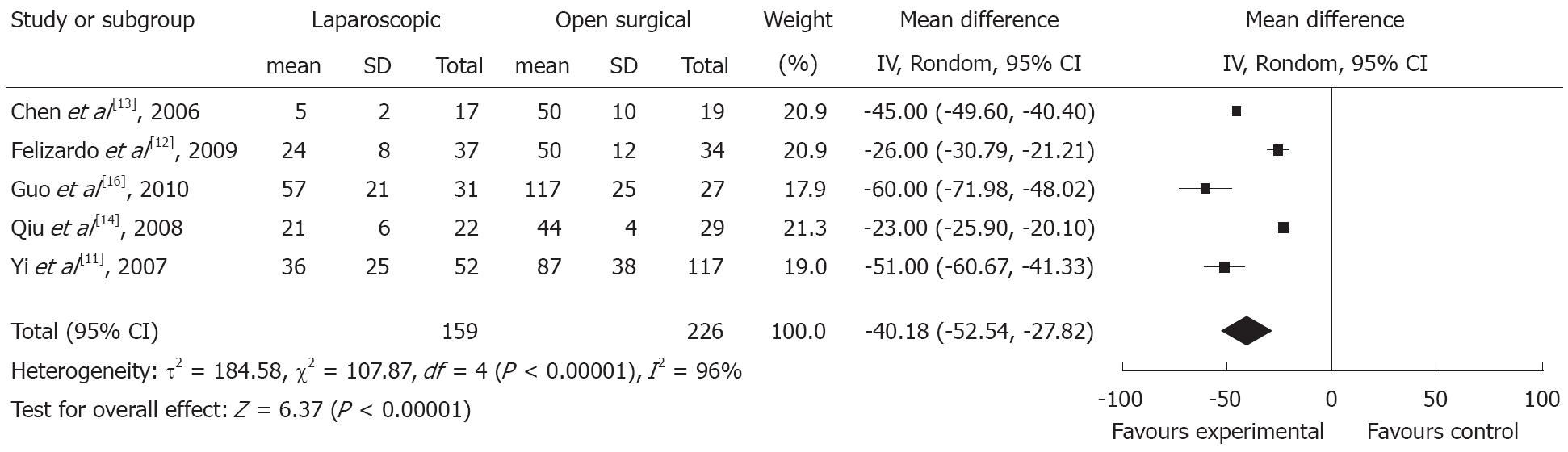
Intraoperative blood loss: Five studies[11-14,16] reported on intraoperative blood loss. The intraoperative blood loss is significantly lower in the LF than in the OF group (MD: -40.18, 95% CI: -52.54 to -27.82, P < 0.00001) and this finding was associated with significant heterogeneity between studies (P < 0.00001, I2 = 96%) (Figure 4).
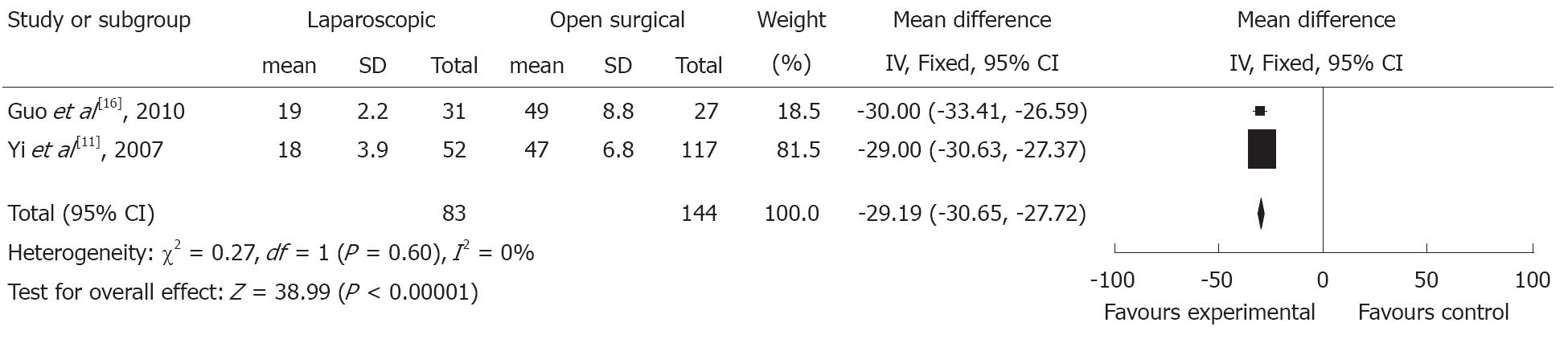
Time to return to normal diet: Two studies[11,16] reported on the specific data about the time to return to normal gastrointestinal function. Meta-analysis of the two studies shows that the time to return to normal gastrointestinal function is significantly earlier in the LF group (MD: -29.19, 95% CI: -30.65 to -27.72, P < 0.00001), but this finding was not associated with significant heterogeneity between studies (P = 0.6, I2 = 0%) (Figure 5).
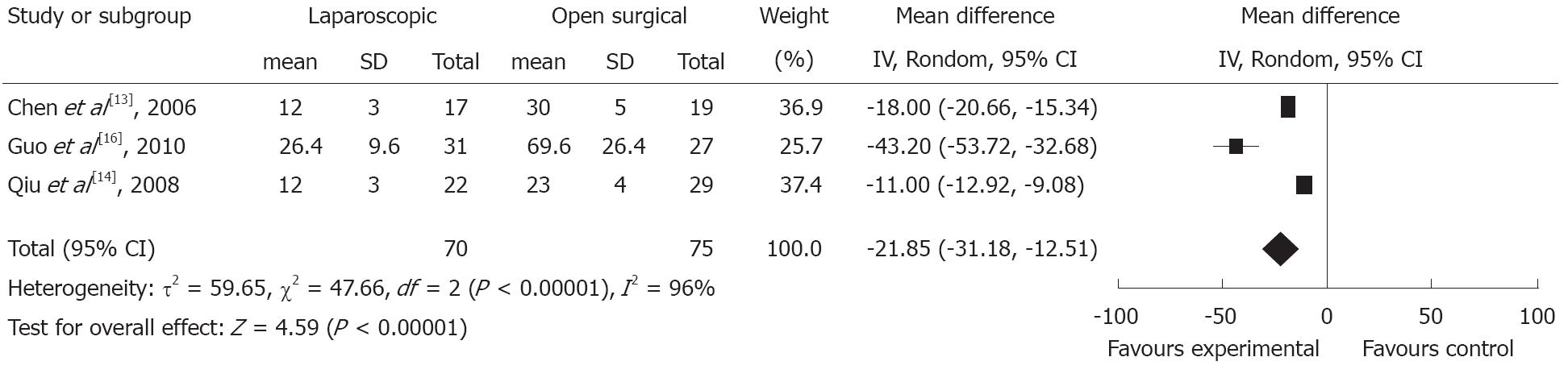
Time to return to normal activities: Three studies[13,14,16] reported on the time to return to normal activities in patients after operation. Meta-analysis of the three studies shows that the time to return to normal activities is significantly shorter in LF group than in OF group (MD: -21.85, 95% CI: -31.18 to -12.51, P < 0.0001) and this finding was associated with significant heterogeneity between studies for calculated analysis (P < 0.00001, I2 = 96%) (Figure 6).
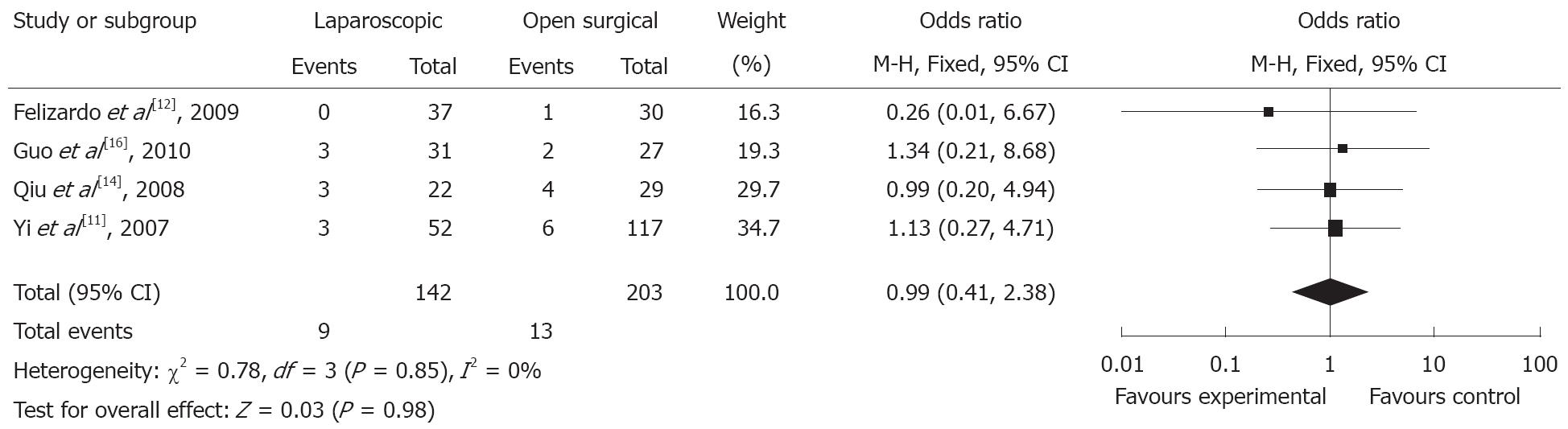
Incidence of postoperative complications: Seven studies reported on the incidence of postoperative complications, but three[17-19] of them did not provide detailed information, we, therefore, extracted the data from four studies[11,12,14,15] and the meta-analysis shows that there is no significant difference in the incidence of postoperative complications between the two groups (OR: 0.99, 95% CI: 0.41 to 2.38, P = 0.98) and this finding was not associated with significant statistical heterogeneity between all available studies (P = 0.85, I2 = 0%) (Figure 7).
Recurrence rates of cysts: Four studies[14,15,17,19] reported on the recurrence rates of cysts through a follow-up from 3 mo to 1 year. However, three[15,17,19] of these studies did not provide sufficient information, but all the four studies showed no significant difference in the recurrence rate of cyst after operation between the two groups.
Postoperative recurrence rates of symptoms: Two studies[14,19] reported on the cyst recurrence rates after operation, but only one study[14] provided a detailed number of relapse. None of the two studies showed significant difference in the recurrence rates of symptoms after operation between LF and OF group.
Time to return to normal liver functions: Only one study[12] compared the time to return to normal liver function after operation and suggested that the liver function was normalized earlier in the LF than in the OF group (P < 0.01).
Hospitalization cost: Only one study[12] reported on the hospitalization costs and suggested that there was no significant difference between the two groups (P = 0.91).
A significant heterogeneity between the two groups was observed in the operative time, intraoperative blood loss, time to return to diet, time to return to activities and duration of hospital stay.
In this systematic review and meta-analysis, we attempted to collect the best evidence-based proofs with respect to LF and OF in patients with congenital hepatic cysts. A total of nine retrospective case-control studies that compared the outcomes of the two approaches for congenital hepatic cysts were identified for final pooled analysis. The methodological quality of all the nine studies was moderate to poor, and some publications have certain methodological deficiencies, such as not mentioning the allocation methods, smaller sample size as well as not adopting methods to reduce the bias in the statistical analysis. All these factors will affect the final reliability of the conclusions from this meta-analysis.
The conventional therapeutic options for congenital hepatic cyst were either percutaneous aspiration or open surgery, while percutaneous aspiration was accompanied by a high recurrence rate[20]. It has been reported the recurrence rate of hepatic cyst after drainage was up to 100%[21], while open approach was always associated with significant morbidity and mortality postoperatively. Since the first performance of LF in a 73-year-old patient who presented with symptomatic uncomplicated liver cysts in 1991[22], an increasing number of successful reports on the management of laparoscopy have been published, including laparoscopic management for complex and parasitic cysts. Currently, laparoscopy is considered as a standard treatment for uncomplicated hepatic cysts. Parasitic liver cysts are not the review scope of this paper.
In this paper, we systematically reviewed the relevant literatures and conducted a meta-analysis of the measured outcomes of LF vs OF for congenital hepatic cysts, which demonstrated that symptom relief, recurrence rates, hospitalization cost, postoperative complications of the LF appear to be similar to the OF group, but the operative time, hospital stay, intraoperative bleeding and time to return to normal gastrointestinal functions and activities seem to be lower, it appears to be a safe and feasible alternative to open surgery for the management of congenital hepatic cyst, however, up to now, only a small number of comparative, non-randomized studies have been published which limited the extrapolation of the results to the clinical setting.
This meta-analysis of nonrandomized studies may have several limitations that must be taken into account when considering its results. First, there are fewer clinical RCTs of laparoscopic vs open approach in congenital hepatic cyst patients. Furthermore, due to the absence of blinding and high risk of bias, the overall methodological quality of all included studies was judged by the peers. Finally, the results from non-randomized controlled trails need to be evaluated, thus restricting its application in clinical practice.
This review included nine non-randomized controlled clinical trials, and a total of 657 patients were analyzed. The results demonstrated that the short-term outcomes of laparoscopic management seem to be successful in patients with congenital liver cysts if preoperative diagnosis is accurate. However, up to now, there are only a small number of comparative, nonrandomized studies published and many authors merely documented the technical feasibility of the procedure and did not present the follow-up outcomes. Therefore, the above-mentioned outcomes should be used with caution, and extended follow-ups are required to assess the long-term survival rates before any definitive conclusions can be drawn.
An increasing number of studies have reported the benefits of laparoscopic fenestration (LF) for hepatic cyst patients, however, the majority of studies merely documented the technical feasibility of this procedure and did not compared its outcomes to conventional open gastric resection. In this paper, therefore, a systematic review and meta-analysis were performed to search for the best evidence for LF in the management of patients with congenital hepatic cysts.
From a technical point of view, hepatic cysts may be treated interventionally by aspiration or surgical fenestration, enucleation and formal hepatic resection. Laparoscopic surgery is the most popular approach because this technique is safe, resulting in a shorter hospital stay and an early return to normal activities.
This review suggests that the short-term outcomes of LF were superior to open approach for patients with congenital hepatic cysts. To our knowledge, this is the first systematic review using the meta-analysis to study the benefit of LF in the management of congenital hepatic cysts.
The LF for congenital liver cysts is feasible and effective, with superior short-term outcomes as compared with the open fenestration (OF). Although randomized controlled trials with measured outcomes are not available, laparoscopic treatment of uncomplicated parenchymal liver cysts is considered as a standard treatment.
This is a technically good study of OF vs LF.
Peer reviewer: David Lawson Morris, Professor, UNSW, Department of Surgery, St George Hospital, Kogarah, NSW 2217, Australia
S- Editor Tian L L- Editor Ma JY E- Editor Zheng XM
| 1. | Caremani M, Vincenti A, Benci A, Sassoli S, Tacconi D. Ecographic epidemiology of non-parasitic hepatic cysts. J Clin Ultrasound. 1993;21:115-118. |
| 2. | Klotz HP, Schlumpf R, Weder W, Largiadèr F. Minimal invasive surgery for treatment of enlarged symptomatic liver cysts. Surg Laparosc Endosc. 1993;3:351-353. |
| 3. | Gloor B, Ly Q, Candinas D. Role of laparoscopy in hepatic cyst surgery. Dig Surg. 2002;19:494-499. |
| 4. | Katkhouda N, Mavor E. Laparoscopic management of benign liver disease. Surg Clin North Am. 2000;80:1203-1211. |
| 5. | Pitale A, Bohra AK, Diamond T. Management of symptomatic liver cysts. Ulster Med J. 2002;71:106-110. |
| 6. | Sharma KC, Kabinoff G, Ducheine Y, Tierney J, Brandstetter RD. Laparoscopic surgery and its potential for medical complications. Heart Lung. 1997;26:52-64; quiz 65-67. |
| 7. | Gagner M, Rogula T, Selzer D. Laparoscopic liver resection: benefits and controversies. Surg Clin North Am. 2004;84:451-462. |
| 8. | Cappellani A, Zanghì A, Di Vita M, Menzo EL, Conti P. Nonparasitic cysts of the liver: laparoscopic treatment and long-term results. Ann Ital Chir. 2002;73:85-88; discussion 89. |
| 9. | Morino M, De Giuli M, Festa V, Garrone C. Laparoscopic management of symptomatic nonparasitic cysts of the liver. Indications and results. Ann Surg. 1994;219:157-164. |
| 10. | Que F, Nagorney DM, Gross JB, Torres VE. Liver resection and cyst fenestration in the treatment of severe polycystic liver disease. Gastroenterology. 1995;108:487-494. |
| 11. | Yi XW, Huang J, Guo WC, Lu CY, Chen ZY, Liu ZH. The clinical analysis of laparoscopic fenestration in treatment of congenital hepatic cyst. Chuanbei Yixueyuan Xuebao. 2007;22:236-238. |
| 12. | Felizardo M, Ding YM, Wang CT, Liu YL, Wang B, Chen XY, Zhang AM. Comparative study on laparoscopic and open fenestration. Zhongguo Weichuang Waike Zazhi. 2009;9:999-1001. |
| 13. | Chen WB, Wu SL, Tan MY. Comparative study of laparoscopic and open fenestration in liver cyst. Guangdong Yixue. 2006;27:1073-1074. |
| 14. | Qiu W, Wang GY. Congenital liver cyst compared the efficacy of laparoscopy and laparotomy fenestration in congenital liver cyst. Jilin Yixue. 2008;29:2189-2190. |
| 15. | Li FG, Yang JY, Lin QY, Yan LN. Experience of therapy for 196 patients with symptomatic congenital cyst of liver. Sichuan Yixue. 2005;26:263-265. |
| 16. | Guo WC, Huang J, Yi XW, Lu CY, Lu LJ. The clinical analysis of laparoscopic fenestration and abdominal fenestration in the treatment of congenital hepatic cyst. Weichangbingxue he Ganbingxue Zazhi. 2010;4:24-28. |
| 17. | Mazza OM, Fernandez DL, Pekolj J, Pfaffen G, Sanchez Clariá R, Molmenti EP, de Santibañes E. Management of nonparasitic hepatic cysts. J Am Coll Surg. 2009;209:733-739. |
| 18. | Gigot JF, Metairie S, Etienne J, Horsmans Y, van Beers BE, Sempoux C, Deprez P, Materne R, Geubel A, Glineur D. The surgical management of congenital liver cysts. Surg Endosc. 2001;15:357-363. |
| 19. | Treckmann JW, Paul A, Sgourakis G, Heuer M, Wandelt M, Sotiropoulos GC. Surgical treatment of nonparasitic cysts of the liver: open versus laparoscopic treatment. Am J Surg. 2010;199:776-781. |
| 20. | Saini S, Mueller PR, Ferrucci JT, Simeone JF, Wittenberg J, Butch RJ. Percutaneous aspiration of hepatic cysts does not provide definitive therapy. AJR Am J Roentgenol. 1983;141:559-560. |
| 21. | Gigot JF, Legrand M, Hubens G, de Canniere L, Wibin E, Deweer F, Druart ML, Bertrand C, Devriendt H, Droissart R. Laparoscopic treatment of nonparasitic liver cysts: adequate selection of patients and surgical technique. World J Surg. 1996;20:556-561. |
| 22. | Z’graggen K, Metzger A, Klaiber C. Symptomatic simple cysts of the liver: treatment by laparoscopic surgery. Surg Endosc. 1991;5:224-225. |