Copyright
©2008 The WJG Press and Baishideng.
World J Gastroenterol. Feb 21, 2008; 14(7): 1027-1033
Published online Feb 21, 2008. doi: 10.3748/wjg.14.1027
Published online Feb 21, 2008. doi: 10.3748/wjg.14.1027
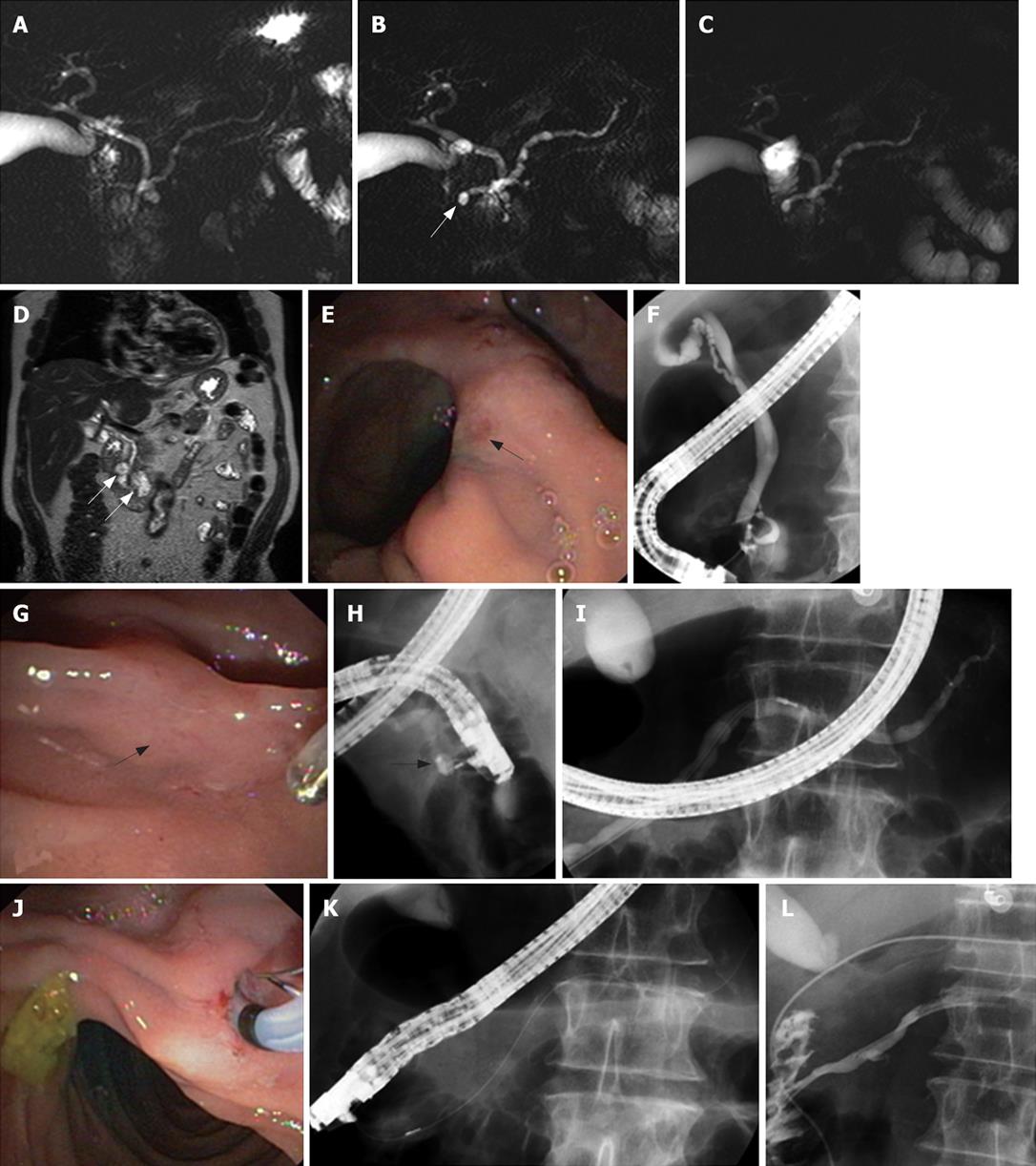
Figure 2 An 80-year-old man presented with 3 attacks of acute pancreatitis over 5 yr.
There was no history of alcohol abuse, smoking, nor medications. There were no gallbladder stones at transabdominal ultrasound and no common bile duct stones at endoscopic ultrasonography. Unenhanced (A) and secretin-enhanced magnetic resonance cholangiography (B) 3 min after secretin injection and C: 10 min after secretin injection). Ectasia of the minor papilla (Santorinicele) (arrow in B) is seen only after secretin administration. Dilatation of the main pancreatic duct persists 10 min after secretin stimulation (C), suggesting obstruction at the level of the minor papilla. Coronal view on T2-weighted magnetic resonance imaging (D) shows 2 paraduodenal diverticula (arrows in D). The major papilla is located on a fold between 2 diverticula (arrow in E), whereas the minor papilla is extremely difficult to locate even after secretin injection and methylene blue staining (arrow in G). During ERCP, cannulation of the major papilla allows opacification of a normal common bile duct and a short ventral pancreatic duct (F). Cannulation of the minor papilla using the needle, in the long scope position, allows opacification of a cystic dilatation of the distal part of the dorsal pancreatic duct (Santorinicele, arrow in H). The main dorsal pancreatic duct is dilated (maximal diameter: 8.3 mm after correction for magnification) (I). Endoscopic minor papillotomy is performed with a standard pull-type sphincterotome (J-K) and subsequently a 6 Fr nasopancreatic catheter is inserted for 24 h (L). After sphincterotomy, contrast medium flows freely alongside the nasopancreatic catheter into the duodenum.
- Citation: Delhaye M, Matos C, Arvanitakis M, Devière J. Pancreatic ductal system obstruction and acute recurrent pancreatitis. World J Gastroenterol 2008; 14(7): 1027-1033
- URL: https://www.wjgnet.com/1007-9327/full/v14/i7/1027.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.1027