Published online Mar 7, 2007. doi: 10.3748/wjg.v13.i9.1460
Revised: December 28, 2006
Accepted: January 27, 2007
Published online: March 7, 2007
Angiolipoma is a rare vascular variant of the benign lipomatous tumors and is generally seen in subcutaneous tissues. We report a 70-year-old female with abdominal distension not related to rectal small polypoid mass with peduncule described as angiolipoma by histologically, and review the literature.
- Citation: Kacar S, Kuran S, Temucin T, Odemis B, Karadeniz N, Sasmaz N. Rectal angiolipoma: A case report and review of literature. World J Gastroenterol 2007; 13(9): 1460-1465
- URL: https://www.wjgnet.com/1007-9327/full/v13/i9/1460.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i9.1460
Lipomas, lipomatosis, lipoblastoma, lipoblastomatosis, angiolipomas, myolipomas, chondroid lipomas, spindle cell lipomas, and pleomorphic lipomas are the benign adipose tissue tumors[1]. Angiolipoma is one of the rare subcutaneous tissue tumors with its characteristic histology consisting of mature adipose tissue and interspersed proliferated vascular component[1-3]. It accounts for 5%-17% of lipomas[2,4,5], and is rarely seen in the gastrointestinal system (GIS). The locations of gastrointestinal angiolipoma according to the current literature are oropharyngeal region[4,6-8], esophagus[9], stomach[10-13], duodenum[14,15], small intestine[3,16-18], ileocecal valve[19-21], colon[14,22-24] and liver[25-28]. Angiolipomas localized in the gastrointestinal tract, characterized as submucosal solitary sessile[10,11,18,20] or endoluminal polypoid lesions[9,12,14,23,24], are diagnosed generally by postoperative histopathologic evaluation or after polypectomy. Radiologic techniques such as barium radiographs, enteroclysis, abdominal ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) can demonstrate the lesion in the gastrointestinal tract before histopathologic diagnosis[24].
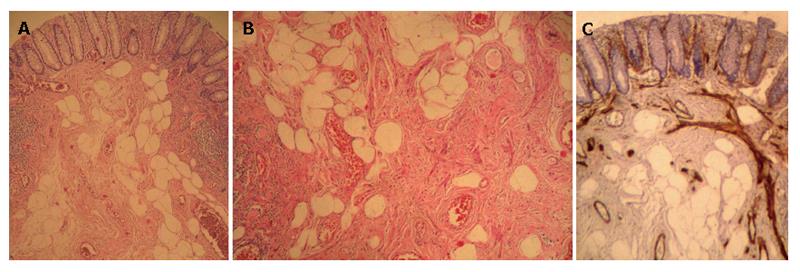
A 70-year-old woman admitted to the hospital with complaints of abdominal distension and constipation. She had no abdominal pain, rectal bleeding or weight loss. Her total blood count, serum biochemistry, sedimentation rate and abdominal ultrasound were normal. A polyp (1 cm in diameter) with lobulated and degenerated hyperemic mucosa and normal peduncle was seen at proximal rectum. Polypectomy was performed by endoscopic polypectomy snare and no complication occurred. Angiolipoma was diagnosed after histopathologic evaluation in mature adipose tissue and proliferous blood vessels (Figure 1). There was no fibrin thrombus and no muscle structure in histologic examination with HMB45 (monoclonal mouse anti-human melanosome, Dako, USA) and anti-smooth muscle antibody (mouse anti-human primary alpha-smooth muscle actin, Dako, USA) tissue stainings. There were no other lesions in total colonoscopy and esophagogastroduodenoscopy. No photograph of the polyp was taken before resection because externally there was no special difference in adenomatous polyps with degenerated surface mucosa.
Angiolipomas are benign lipomatous lesions, which were first defined by Bowen[29] in 1912 and differentiated from lipomas histopathologically by Howard in 1960[30]. The lipomatous benign lesions are seen as musculoskeletal masses especially in soft tissues and bones[1,2]. They are generally subcutaneous and capsulated, about 50% patients feel painful on palpation, and seen in young adult males in their 2nd or 3rd decades of life[1,2,24]. They are also localized in neck[4,31], maxillofacial region[32-35] and non-subcutaneous tissues such as epidural[36], spinal[37-39], and suprasellar tissues[40]. Lipomas are seen more frequently, but angiolipomas are rare lesions[1,5]. Gastrointestinal angiolipoma is also a rare pathological condition[1,24]. The other uncommon localizations of angiolipomas are the renal tissue[41-44], adrenal tissue[45,46], breast[47], thyroid glands[48], parotid gland[49], mediastinum[50], orbits[51], myocardium[52] and scrotum[53].
In the musculoskeletal system, angiolipomas are 70% multiple and 10% familial[5]. It can have an autosomal dominant penetrance[1,22]. The mode of inheritence in GIS is still not clear[54].
Histologically, it is comprised of mature adipose tissue and proliferated vascular tissues. It can be classified as predominantly lipomatous or angiomatous type, based on the ratio of adipose tissue and vascular tissue composition[1,2,5]. Fibrin thrombus due to microtraumas is generally seen in angiomatous lesions[5,11,20,23,48]. Angiolipomas localized in muscle and cutaneous tissue can have two different behavior patterns: infiltrative or non-infiltrative[5]. But the gastrointestinal cases defined in the literature have been non-infiltrating and showed no recurrence during follow-up periods (Table 1).
| Literature | Localization | Case(age/sex) | Polyp size | Polyp peduncle | Symptom | Preoperativediagnosticimagingmethods(exceptendoscopicprocedure) | Therapy | Follow-up(F/U)/recurrence |
| Jensen EH et al[9] 2006 | Esophagus | 85 yr/M | 39 mm x 25 mm | Pedunculated large polyp | A 2-mo dysphagia to solids foods, complete esophageal obstruction; had prolapsed to the level of the GE junction | CT , EUS | Anterior esophagotomy, transsection of polyp using an endoscopic stapling device (open surgical excision) | No F/U |
| DeRidder Ph et al[10] (1989) | Stomach | 59 yr/M | 6 mm | Submucosal well demarcated mass | Chronic occult GI bleeding | Laparotomy- excision | 12 mo/No recurrence | |
| McGregor DH et al[11] (1993) | Stomach | 69 yr/M | 50 mm x 40 mm x 20 mm | Gastric submucosal mass on great curvature, without peduncle | Chronic hemorrhage and severe anemia | Exploratory laparotomy, mass resection | 30 mo/No recurrence | |
| Hunt J et al[12] (1996) | Stomach | 27 yr/F | 80 mm x 55 mm x 45 mm | Large polypoid mass with large peduncle | Suggestive of intussusception through the pylorus, acute GI hemorrhage | Exploratory laparotomy, distal partial gastrectomy, Billroth I gastric reconstruction, resection of polyp | not given/ No recurrence | |
| Mohl W et al[14] (2004)2 | Duodenum, Colon | The first was 66 yr/M, the second was 75 yr/F (2 pts with 1 duodenal and colonic A-L other duodenal A-Ls) | 1st-10 mm located near papilla of Vater, and colon 2nd-23 mm at the upper duodenal knee | Both with peduncle | 1st acute, 2nd chronic GI bleeding Upper GI bleeding due to duodenal A-L | Endoscopic snare polypectomy for 2 duodenal and for 1 colonic A-Ls | not given/ No recurrence | |
| Jung IS et al[15] (2004) | Duodenum | 60 yr/F | 35 mm x 4 mm | With peduncle | Dyspepsia for 6 mo | EUS | Endoscopic polypectomy | No F/U |
| Kaneko T et al[16] (1996)1 | Meckel’s diverticulum accompanied A-L | Intussusception | ||||||
| Ferrozzi F et al[3] (1998) | Ileal | With tuberous sclerosis | CT | |||||
| Manner M et al[17] (2001) | Proximal ileum | 71 yr/F | 38 mm | With peduncle | Occult bleeding, ileoileal intussusception | US, CT | Small bowel resection | |
| Kwak HS et al[18] (2003) | Small bowel/ proximal ileum | 75 yr/M | 30 mm | Intraluminal lobulated polypoid mass with peduncle | Epigastric discomfort, loss of appetite, weight loss | Enteroclysis, MRI | Surgery | No F/U |
| Aouad K et al[19] (2000) | (Bauhin valve) ileocecal valve | Gastrointestinal hemorrhage | ||||||
| Kato K et al[20] (1999)1 | Ileocecal valve | 69 yr/M | 52 mm x 50 mm x 40 mm | Without peduncle, a submucosal smooth surface mass A-L | 3-d right lower quadrant abdominal pain | Contrast enhanced abdominal CT | Laparoscopy-assisted ileocecostomy, and a side-to- side anastomosis extracorporeally (a minimally invasive laparoscopic technique) | 5 yr/No recurrence |
| Saroglia G et al[21] (1996) | Ileocecal valve | 55 yr/M | 55 mm | Submucousal mass | Invagination | Barium contrast graphy | Surgery | No F/U |
| Vandamme J et al[22] (1964) | Descending colon | 43 yr/M | 150 mm x 40 mm | With peduncle | GI bleeding and non painful sub- obstruction by invagination | Barium contrast graphy | Surgery, colon resection | not given/ No recurrence |
| Okuyama T et al[23] (2002) | Sigmoid colon | 49 yr/M | 65 mm x 23 mm | Pedunculated polyp with smooth surface | Asymptomatic, during routine exam positive fecal blood | Double contrast enema, enhanced CT | Hemostatic clip and endoscopic electro- surgical polypectomy | No F/U |
| Chen YY et al[24] (2005) | Transvers colon | 70 yr/M | 50 mm | With peduncle | Colonic obstruction | US, Abdominal CT, Colonic barium enema, colonoscopic examination | Surgical segmental resection | 2 yr/No recurrence |
| Kacar S et al | Rectum | 70 yr/F | 10 mm | With peduncle | Asymptomatic | - | Polypectomy performed by endoscopic polypectomy snare | 6 mo/No recurrence Under F/U |
Eight maxillofacial angiolipomas had been reported in the literature until 1989[7] and 17 head and neck angiolipomas until 1999[4]. There are also cases in the literature of oropharyngeal angiolipomas including tongue, cheek mucosa and palate[4,6-8].
Angiolipomas localized in the GIS or liver. Although hepatic localization of lipomatous tumors is seen more frequently than gastrointestinal tract, hepatic angiolipomas are also rare lesions in this group[27,28,55,56]. Most lipomatous lesions of the liver[55,56] and hepatic angiolipomas are associated with tuberous sclerosis complex[26].
Seven cases of angiolipoma hade been reported in the gastrointestinal tract in the literature up to 2005[24]. To the best of our knowledge, 17 cases of gastrointestinal angiolipoma have been reported to date (1 esophageal[9], 3 gastric[10-12], 2 duodenal[14,15], 4 small bowel[3,16-18], 3 ileocecal valve[19-21], and 4 colonic)[14,22-24]. Based on these reports, our case would be the first angiolipoma defined in the rectum.
There are syndromes accompanying angiolipomas, such as familial angiolipomatosis, which is rare and benign with mostly autosomal dominant inheritance and multiple angiolipomas of the extremities and trunk[57]. Birt-Hogg-Dube syndrome is an autosomal-dominant condition characterized by fibrofolliculomas, trichodiscomas, and acrochordons[58]. There is only one ileal angiolipoma-associated tuberous sclerosis in the literature[3]. Hunt et al[12] described a case with solitary gastric Peutz-Jeghers polyp and angiolipoma presenting as acute hemorrhage.
Angiolipamas are diagnosed generally as single lesions in the gastrointestinal tract, but Mohl et al[14] described a case of both colonic and duodenal angiolipoma. Angiolipomas in the gastrointestinal tract, as shown in Table 1, can be sessile[10,11,18,20] or pedunculated polypoid lesions[9,12,14,23,24], and the cases in the literature are generally diagnosed based on abdominal pain, obstruction, invagination, intussusception, and acute or chronic bleeding.
Diagnosis of GIS angiolipomas can be made radiologically via contrast barium enema, enteroclysis, abdominal ultrasound, endoscopic ultrasound, abdominal tomography, or MRI before the polypectomy or resection if the lesion is large[9,15,17,18,20,23,24]. Large lesion size and the symptom are the main factors in the radiologic diagnosis, but final diagnoses are done histologically. There is filling-defect in gastrointestinal lumen detected by barium enema[24] and enteroclysis[18], hyperechoic lesion in transabdominal ultrasonography[17,24], submucosal lesion in gastrointestinal wall in endosonography[9], hyperechoic lesion in CT[3,9,14,17,20,23], and central high signal intensity with peripheral iso-signal intensity on T1-weighted in-phase images in MRI[18].
Surgical resection is preferred to endoscopic resection in the case of broad-based or pedunculated large polyps due to risk of perforation and bleeding[9,10,11,12,17,18,20,24]. For pedunculated polyps, injection of epinephrine, or use nylon loop or metal hemostatic clip are suggested before polypectomy to decrease the risk of postoperative bleeding[14,23]. These patients can be treated by standard polypectomy. The level of urgency is also an important factor when choosing the most optimal treatment. In the case of intussusception[16,21], obstruction[9,24] or acute bleeding[12,19,22], emergent surgery is generally suggested. In some cases, minimally invasive laparoscopic techniques can be performed successfully. A cecal lesion was treated successfully with laparoscopy-assisted ileocecostomy and a five-year follow-up showed no recurrence in this patient[22].
Our patient was diagnosed by histopathologic evaluation after snare polypectomy of a single, small polyp with thin peduncle in the rectum. There was no complication after polypectomy. The peduncle was histologically normal. There were proliferated blood vessels and mature adipose tissue in the submucosa and no fibrin thrombus was found. Mature adipose tissue and proliferated blood vessels are the diagnostic components as defined in the literature. Fibrin thrombus in the vascular component is a common finding[5,11,20,23]. The histopathological findings of the cases in the literature are given in Table 2.
| Literature | Histopathological findings under light microscope |
| Jensen EH et al[9] | A submucosal polypoid mass, consisting of benign lipomatous tissue mixed with vascular channels, consistent with benign angiolipoma |
| DeRidder et al[10] | Submucosa contained a well demarcated nodule composed of flat, extending from the under surface of the muscularis mucosa to the deep margin of biopsy. There were separate, well developed small arteries and veins |
| McGregor D et al[11] | A circumbscribed, lobular, pinkish-tan soft ovoid mass showing proliferation of mature adipose tissue and vascular tissue surrounded by a thin to focally thick fibrous capsule in the submucosa, no definite fibrin trombi |
| Hunt J et al[12] | A solitary Peutz-Jeghers-type polyp showing typical glandular epithelium, overriding a 5 cm gastric angiolipoma |
| Mohl W et al[14] | 2 submucosal duodenal angiolipomas, one with large central vessel and one colonic angiolipoma |
| Yung IS et al[15] | A submucosal lesion composed of mature adipose tissue and small vessels with fibrin thrombi within the vascular channels |
| Manner M et al[17] | An angiolipoma with 20% vascular component and mucosal ulceration |
| Kwak HS et al[18] | Mature, higly vascular adipose tissue consistent with angiolipoma |
| Kato K et al[20] | A circumbscribed proliferation of mature adipose and vascular tissue surrounded by a thin to focally thick fibrous capsule in the submucosa, with fibrin thrombi in small capillaries |
| Saroglia G et al[21] | Mature adipose and vascular tissue |
| Vandamme J et al[22] | Angiolipoma with multiple small vessels and adipose tissue |
| Okuyama T et al[23] | Encapsulated by a thin layer of connective tissue, arising in the submucosa and composed of mature adipose tissue and proliferating capillaries, many fibrin thrombi in capillary lumen |
| Chen YY et al[24] | Encapsulated by a thin layer of connective tissue arising from the submucosa, histologically was comprised of mature adipose tissue and proliferative blood vessels |
| Kacar S et al | Proliferated submucosal blood vessels and mature adipose tissue. There was no fibrin thrombus |
The polyp was not responsible for the dyspeptic symptoms and constipation in our patient. Although the polyp could have caused rectal bleeding, no bleeding occurred in our patient. The lesion was thus considered as asymptomatic. The sigmoid angiolipoma in literature[23] was asymptomatic, but 65 mm in diameter. Our case is the first rectal, small, asymptomatic angiolipoma diagnosed incidentally in the gastrointestinal tract.
Although angiolipomas are benign lesions among adipose tissue neoplasms, additional staining techniques are required to distinguish from malignant lipomatous forms like angioliposarcoma[27,28]. The resection material of our patient was stained by HMB45 and anti-smooth muscle antibody, and found negative for muscle fibers. The differential diagnosis was made between angiomyolipoma and angioliposarcoma.
In conclusion, it is important to remember that submucosal, sessile, or polypoid lesions in the gastrointestinal tract with or without symptoms can be an angiolipoma, a lipomatous tumor, although it is quite rare.
S- Editor Liu Y L- Editor Ma JY E- Editor Zhou T
| 1. | Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. From the archives of the AFIP: benign musculoskeletal lipomatous lesions. Radiographics. 2004;24:1433-1466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 368] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 2. | Punia RS, Jain P, Amanjit H, Singh R. Subcutaneous angiolipomas: a clinicopathological study of 12 cases. Indian J Pathol Microbiol. 2005;48:197-198. [PubMed] |
| 3. | Ferrozzi F, Rubino S, Uccelli M. Ileal angiolipoma in a patient with multisystemic manifestations of tuberous sclerosis: diagnosis with computerized tomography. Radiol Med. 1998;96:403-405. [PubMed] |
| 4. | Vigili MG, Micozzi M, Moreschini G, Colacci AC, Masci P, Silvagni C. Oropharyngeal angiolipoma: a case study. Acta Otorhinolaryngol Ital. 1999;19:348-351. [PubMed] |
| 5. | Choong KK. Sonographic appearance of subcutaneous angiolipomas. J Ultrasound Med. 2004;23:715-717. [PubMed] |
| 6. | Flaggert JJ, Heldt LV, Keaton WM. Angiolipoma of the palate. Report of a case. Oral Surg Oral Med Oral Pathol. 1986;61:333-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Lin SC, Wang TY, Hahn LJ. Angiolipoma of the tongue: report of a case. Ann Dent. 1989;48:37-38. [PubMed] |
| 8. | Brahney CP, Aria AA, Koval MH, Najjar TA. Angiolipoma of the tongue: report of case and review of literature. J Oral Surg. 1981;39:451-453. [PubMed] |
| 9. | Jensen EH, Klapman JB, Kelley ST. Angiolipoma of the esophagus: a rare clinical dilemma. Dis Esophagus. 2006;19:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | DeRidder PH, Levine AJ, Katta JJ, Catto JA. Angiolipoma of the stomach as a cause of chronic upper gastrointestinal bleeding. Surg Endosc. 1989;3:106-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | McGregor DH, Kerley SW, McGregor MS. Case report: gastric angiolipoma with chronic hemorrhage and severe anemia. Am J Med Sci. 1993;305:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Hunt J, Tindal D. Solitary gastric Peutz-Jeghers polyp and angiolipoma presenting as acute haemorrhage. Aust N Z J Surg. 1996;66:713-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Ferrozzi F, Tognini G, Bova D, Pavone P. Lipomatous tumors of the stomach: CT findings and differential diagnosis. J Comput Assist Tomogr. 2000;24:854-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Mohl W, Fischinger J, Moser C, Remberger K, Zeuzem S, Stallmach A. Duodenal angiolipoma -- endoscopic diagnosis and therapy. Z Gastroenterol. 2004;42:1381-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Jung IS, Jang JY, Ryu CB, Hong SJ, Kim JO, Cho JY, Lee JS, Lee MS, Jin SY, Shim CS. Angiolipoma of the duodenum diagnosed after endoscopic resection. Endoscopy. 2004;36:375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Kaneko T, Karasawa Y, Inada H, Tamura Y, Yamamura N, Iijima Y, Nagata A, Oohata T, Shirota H, Nakamura T. An adult case of intussusception due to inverted Meckel's diverticulum accompanied by angiolipoma. Nihon Shokakibyo Gakkai Zasshi. 1996;93:260-265. [PubMed] |
| 17. | Manner M, Scholz E, Wehrmann M, Stickel W. Invagination caused by angiolipoma of the small intestine--a rare cause of occult gastrointestinal hemorrhage. Chirurg. 2001;72:305-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Kwak HS, Kim CS, Lee JM. Small intestinal angiolipoma: MR imaging appearance. Abdom Imaging. 2003;28:515-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Aouad K, Texier P, Bloch F, De Labriolle-Vaylet C, Bouillot JL. Benign angiolipoma of the Bauhin valve causing severe digestive tract bleeding. Gastroenterol Clin Biol. 2000;24:686-688. [PubMed] |
| 20. | Kato K, Matsuda M, Onodera K, Sakata H, Kobayashi T, Kasai S. Angiolipoma of the colon with right lower quadrant abdominal pain. Dig Surg. 1999;16:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Saroglia G, Coverlizza S, Roatta L, Leli R, Fontana D. Angiolipoma of the cecum. Minerva Chir. 1996;51:59-62. [PubMed] |
| 22. | Vandamme J. Angiolipoma of the colon. Acta Gastroenterol Belg. 1964;27:750-757. [PubMed] |
| 23. | Okuyama T, Yoshida M, Watanabe M, Kinoshita Y, Harada Y. Angiolipoma of the colon diagnosed after endoscopic resection. Gastrointest Endosc. 2002;55:748-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Chen YY, Soon MS. Preoperative diagnosis of colonic angiolipoma: a case report. World J Gastroenterol. 2005;11:5087-5089. [PubMed] |
| 25. | Strotzer M, Paetzel C, Feuerbach S. Multiple hepatic angiolipomas: a case report and review of literature. Eur Radiol. 1999;9:259-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Huber C, Treutner KH, Steinau G, Schumpelick V. Ruptured hepatic angiolipoma in tuberous sclerosis complex. Langenbecks Arch Chir. 1996;381:7-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 27. | Zhang SH, Cong WM, Xian ZH, Wu WQ, Dong H, Wu MC. Morphologic variants and immunohistochemical features of hepatic angiomyolipoma. Zhonghua BingLiXue ZaZhi. 2004;33:437-440. [PubMed] |
| 28. | Tsui WM, Ng IO, Colombari R, Pea M. Hepatic angiomyolipomas. Histopathology. 1993;22:602-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Bowen JT. Multiple subcutaneous hemangiomas, together with multiple lipomas, occurring in enormous numbers in an otherwise healthy, muscular subject. Am J Med Sci. 1912;144:189-192. [RCA] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82:924-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 236] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 31. | Saydam L, Bozkurt MK, Ugur MB, Ozcelik T, Kutluay L. Angiolipoma of the neck: a case report. Ear Nose Throat J. 2005;84:375-377. [PubMed] |
| 32. | Hamakawa H, Hino H, Sumida T, Tanioka H. Infiltrating angiolipoma of the cheek: a case report and a review of the literature. J Oral Maxillofac Surg. 2000;58:674-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Ali MH, el-Zuebi F. Angiolipoma of the cheek: report of a case. J Oral Maxillofac Surg. 1996;54:213-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Shohet JA, Simpson B, Coleman JR, Geiger XJ. Angiolipoma presenting as a nasal mass. Otolaryngol Head Neck Surg. 1998;118:848-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Pfannenstiel TJ, Boseley M, Roach L. A case of paranasal sinus angiolipoma. Laryngoscope. 2003;113:1080-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Hattori H. Epidural angiolipoma is histologically distinct from its cutaneous counterpart in the calibre and density of its vascular component; a case report with review of the literature. J Clin Pathol. 2005;58:882-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Petrella G, Tamburrini G, Lauriola L, Di Rocco C. Spinal epidural angiolipoma complicated by an intratumoral abscess. Case report. J Neurosurg. 2005;103:166-169. [PubMed] |
| 38. | Konya D, Ozgen S, Kurtkaya O, Pamir NM. Lumbar spinal angiolipoma: case report and review of the literature. Eur Spine J. 2006;15:1025-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 39. | White NJ, Cochrane DD, Beauchamp R. Paraparesis caused by an angiolipomatous hamartoma in an adolescent with Proteus syndrome and scoliosis. J Neurosurg. 2005;103:282-284. [PubMed] |
| 40. | Shuangshoti S, Wangsuphachart S. Angiolipoma of suprasellar region. J Med Assoc Thai. 1995;78:631-634. [PubMed] |
| 41. | Ewalt DH, Diamond N, Rees C, Sparagana SP, Delgado M, Batchelor L, Roach ES. Long-term outcome of transcatheter embolization of renal angiomyolipomas due to tuberous sclerosis complex. J Urol. 2005;174:1764-1766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 42. | de Perrot M, Licker M, Robert J, Nicod L, Spiliopoulos A. Successful combined lung and kidney transplantation for pulmonary lymphangioleiomyomatosis and renal angiolipomas. Eur Respir J. 1998;12:1479-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Verna C, Mosso L, Moncelli G, Monaco A. Renal angiolipoma associated with bilateral double ureter. A clinical case. Minerva Urol Nefrol. 1997;49:39-44. [PubMed] |
| 44. | Alvo M, Passalacqua W, Castro P, Wash A. Tuberous sclerosis with probable bilateral renal angiolipoma. Rev Med Chil. 1988;116:934-937. [PubMed] |
| 45. | Ramacciato G, Lombardi M, Amodio PM, Mercantini P, Petrocca S, Stipa F, Di Giacomo G, Bellagamba R, Puce E, Ziparo V. Laparoscopic adrenalectomy: a worthwhile procedure performed in a general surgery department. Am Surg. 2003;69:427-433. [PubMed] |
| 46. | Maurea S, Mainolfi C, Wang H, Varrella P, Panico MR, Klain M, Rossi R, Cremona F, Bazzicalupo L, Salvatore M. Positron emission tomography (PET) with fludeoxyglucose F 18 in the study of adrenal masses: comparison of benign and malignant lesions. Radiol Med. 1996;92:782-787. [PubMed] |
| 47. | Morakkabati-Spitz N, Schild HH, Leutner CC, von Falkenhausen M, Lutterbey G, Kuhl CK. Dynamic contrast-enhanced breast MR imaging in men: preliminary results. Radiology. 2006;238:438-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 48. | Palazzo JP, Coté SA. Primary angiolipoma of the thyroid gland: a case report. Int J Surg Pathol. 2005;13:305-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Reilly JS, Kelly DR, Royal SA. Angiolipoma of the parotid: case report and review. Laryngoscope. 1988;98:818-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | Gámez García P, de Pablo Gafas A, Salas Antón C, Santolaya Cohen R, Madrigal Royo L, Varela de Ugarte A. Mediastinal dumbbell angiolipoma. Arch Bronconeumol. 2002;38:545-546. [PubMed] |
| 51. | Feinfield RE, Hesse RJ, Scharfenberg JC. Orbital angiolipoma. Arch Ophthalmol. 1988;106:1093-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 52. | Kiaer HW. Myocardial angiolipoma. Acta Pathol Microbiol Immunol Scand A. 1984;92:291-292. [PubMed] |
| 53. | Rajagopalan S. An unusual pediatric scrotal lump. Indian J Pediatr. 2005;72:801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 54. | Sciot R, Akerman M, Dal Cin P, De Wever I, Fletcher CD, Mandahl N, Mertens F, Mitelman F, Rosai J, Rydholm A. Cytogenetic analysis of subcutaneous angiolipoma: further evidence supporting its difference from ordinary pure lipomas: a report of the CHAMP Study Group. Am J Surg Pathol. 1997;21:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 55. | Ji Y, Zhu X, Xu J, Zhou J, Tan Y, Wang J, Fan J, Zhou Y. Hepatic angiomyolipoma: a clinicopathologic study of 10 cases. Chin Med J (Engl). 2001;114:280-285. [PubMed] |
| 56. | Hirasaki S, Koide N, Ogawa H, Ujike K, Shinji T, Tsuji T. Tuberous sclerosis associated with multiple hepatic lipomatous tumors and hemorrhagic renal angiomyolipoma. Intern Med. 1999;38:345-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Cina SJ, Radentz SS, Smialek JE. A case of familial angiolipomatosis with Lisch nodules. Arch Pathol Lab Med. 1999;123:946-948. [PubMed] |
| 58. | Chung JY, Ramos-Caro FA, Beers B, Ford MJ, Flowers F. Multiple lipomas, angiolipomas, and parathyroid adenomas in a patient with Birt-Hogg-Dube syndrome. Int J Dermatol. 1996;35:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 2.4] [Reference Citation Analysis (0)] |