Published online Aug 28, 2007. doi: 10.3748/wjg.v13.i32.4316
Revised: April 23, 2007
Accepted: April 30, 2007
Published online: August 28, 2007
AIM: To examine how the introduction of endoscopy to gastric cancer screening affected survival prognosis in a regional population.
METHODS: The subjects comprised 4261 residents of Kamigoto, Nagasaki Prefecture, who underwent gastric X-ray examination for gastric cancer screening from 1991 to 1995, and all 7178 residents who underwent endoscopic examination for the same purpose from 1996 to 2003. The analysis evaluated trends in age-adjusted gastric cancer mortality rates and standard mortality ratios (SMRs) among the Kamigoto residents.
RESULTS: According to demographic statistics, the 1995 and 2000 age-adjusted gastric cancer mortality rates in Nagasaki Prefecture (per 100 000 population) were 42.6 and 37.3 for males and 18.6 and 16.0 for females, while the corresponding rates in Kamigoto before and after the introduction of endoscopic screening were respectively 51.9 and 28.0, and 26.6 and 6.9. The data obtained in this study were divided into those for two periods, 1990-1996 and 1997-2006, and SMRs were calculated separately for males and females. For the first period, the SMR was 1.04 (95% CI 0.50-1.58) for males and 1.54 (95% CI 0.71-2.38) for females, while for the second period the SMR was 0.71 (95% CI 0.33-1.10) for males and 0.62 (95% CI 0.19-1.05) for females.
CONCLUSION: Following the introduction of endoscopic examination, gastric cancer death rates decreased in Kamigoto.
- Citation: Matsumoto S, Yamasaki K, Tsuji K, Shirahama S. Results of mass endoscopic examination for gastric cancer in Kamigoto Hospital, Nagasaki Prefecture. World J Gastroenterol 2007; 13(32): 4316-4320
- URL: https://www.wjgnet.com/1007-9327/full/v13/i32/4316.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i32.4316
Endoscopic examination is gaining acceptance as a means of gastric cancer screening. The importance of gastric endoscopy is its improvement of post-treatment QOL for the growing number of patients for whom endoscopic mucosal resection (EMR) is indicated, and its most anticipated effect is improvement of survival prognosis.
However, evaluation of the effects of endoscopic examination on survival prognosis is incomplete, and a March 2006 report by the Japan Research Group on the Establishment of Appropriate Methodology and Evaluation in Cancer Screening concluded that a level of "I" for endoscopy as part of gastric cancer screening, i.e., implementation in mass screening, could not be recommended.
In the Kamigoto treatment area examined in this study, gastric X-ray examination was replaced by endoscopy as a means of gastric cancer screening in 1996. This study examined how the introduction of endoscopy to gastric cancer screening affected survival prognosis of residents of this area.
Regional screening in the Kamigoto treatment area has long been performed by Kamigoto Hospital in partnership with the Kamigoto town office. Of a target screening population of 7400 people, 3200 have been screened, at a rate of approximately 700-1000 screenings per year. Recruiting of applicants for endoscopic screening is performed through public notices and through activities with outpatients, and screening is free of charge to Kamigoto residents age 40 years or older. A significant number of screenings are performed as part of annual or biennial checkups, though the exact number of such screenings is unknown.
Kamigoto Hospital is a 186-bed general hospital that performs approximately 3000 upper gastrointestinal endoscopies annually. Olympus endoscopes (GIF-Q200, GIF-Q240, GIF-XQ240) are used. Although intramuscular injection of anti-cholinergic agent is given immediately before endoscopy, sedation is not generally performed. Sterilization conforms to the Guidelines of the Japan Gastroenterological Endoscopy Society, and peracetic acid preparation is used as a disinfectant.
At Kamigoto Hospital, eight physicians perform endoscopic examinations, including five internists and three surgeons. Four of them are physicians who completed residency training less than four years ago and thus have less experience performing endoscopic examinations. Diagnosis is made solely by the performing physician. Gastric cancer is diagnosed on the basis of histological examination of forceps biopsy specimens in Kamigoto Hospital.
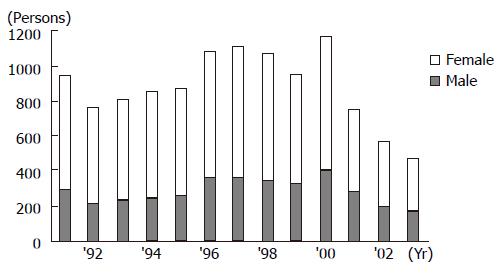
In 1996, the Kamigoto area replaced its conventional gastric barium X-ray examination for gastric cancer screening by endoscopic examination. The subjects of this study included 4261 patients (1246 males, 3015 females) who underwent gastric X-ray examination for gastric cancer screening from 1991 to 1995, and 7178 patients (2432 males, 4746 females), consisting of all individuals who underwent endoscopic screening from 1996 to 2003. In addition, the regional screening included screening offered by local government only, and did not include screening offered by work site. The mean screening rate for the gastric X-ray examination group was 26.6% and the mean rate for the endoscopy group was 28.2%.
To investigate whether reduction of gastric cancer mortality resulted from the introduction of endoscopic examination, gastric cancer cases detected by screening were evaluated in relation to various characteristics of the subjects and by evaluation of outcome (life or death), date of death, and cause of death in patients with gastric cancer for Kamigoto residents, in cooperation with the Kamigoto town office.
Following the introduction of endoscopic examination, a decrease was observed in the number of screened individuals (Figure 1). People aged 60 years or older made up 70% of the endoscopic examination group, with this age group exhibiting a slight increase over time in proportion of all individuals screened.
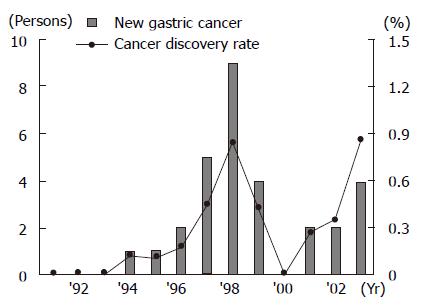
Among the 4261 individuals who underwent gastric X-ray examination, 2 (0.05%) cases of gastric cancer were discovered, compared to a Kamigoto population rate of 9.4/year per 100 000 population, and the mean gastric cancer detection rate was 0.05%. Among the 7178 individuals who underwent endoscopic examination, 28 (0.4%) cases of gastric cancer were discovered, compared to 48.8/year per 100 000 population, and the mean gastric cancer detection rate was 0.4%.
After the introduction of endoscopic screening, the number of gastric cancer cases detected tended to increase (Figure 2). In the gastric X-ray examination group, the 2 cases noted above were detected during initial screening. In the endoscopic examination group, 13 (46.4%) cases were detected during an annual checkup, 3 (10.7%) cases were detected during a biennial checkup, and 4 (14.3%) cases were detected during initial screening.
Table 1 shows the composition of gastric cancer cases detected during screening. Indications for EMR (endoscopic mucosal resection) conformed to the March 2001 Gastric Cancer Treatment Guidelines of the Japanese Gastric Cancer Association. In the gastric X-ray examination group, 1 (0.02%) case of early gastric cancer, 1 (0.02%) case reaching invasive depth M (mucosal layer), and no cases of cancers indicated for EMR were observed. In the endoscopic examination group, the corresponding numbers were 25 (0.35%) cases, 20 (0.28%) cases, and 12 (0.17%) cases. Of the cases detected in the endoscopic examination group, 25 of the 28 (89.3%) were early cancer, suggesting that endoscopy increased the rate of early gastric cancer detection, and 11 of the 28 (39.3%) underwent EMR, 17 of the 28 (60.7%) underwent definitive surgery and no inoperable case was noted. In one case in the gastric X-ray examination group, the patient subsequently died of gastric cancer, though as of December 2006 gastric cancer death was detected in one case and no recurrences had been noted in the endoscopic examination group (Table 1).
| X-ray (n = 4261) | Endoscope (n = 7178) | |
| Gastric cancer detection | 2 | 28 |
| Early-stage | 1/2 | 25/28 (89.3%) |
| Invasion depth (m) | 1/2 | 20/28 (71.4%) |
| Indication for EMR1 | 0/2 | 12/28 (42.9%) |
| Gastric cancer recurrence | 1 | 0 |
| Gastric cancer death | 1 | 1 |
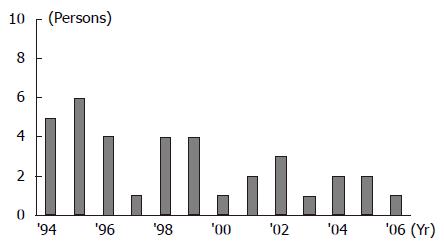
The mean number of gastric cancer deaths in Kamigoto fell from a rate of 5.0/year for the 3-year period from 1994 to 1996 preceding the introduction of endoscopic examination to a rate of 2.1/year for the 10-year period from 1997 to 2006 (Figure 3). Thirty-four (94.4%) cases of these gastric cancer deaths involved unscreened individuals. Since all cases of gastric cancer death in 1996 were detected in fiscal year 1995, they were included in the first period.
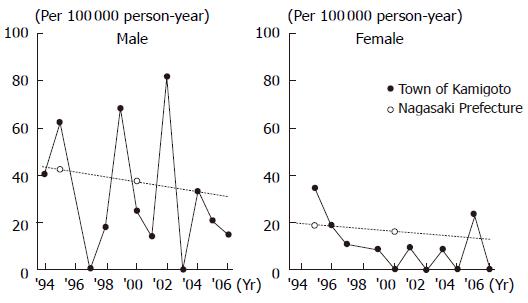
To more accurately characterize findings for Kamigoto, we used data for Nagasaki Prefecture to compare age-adjusted death rates derived from the year-on-year trend in gastric cancer deaths. However, results could not be calculated for males in 1996 or for females in 1994 and 1998 due to lack of confirmation of age at time of death. According to demographic statistics, the age-adjusted gastric cancer death rates (per 100 000 population) for Nagasaki Prefecture were 42.6 for males and 18.6 for females in 1995, and 37.3 for males and 16.0 for females in 2000. In Kamigoto, the corresponding mean values for the 3-year period from 1994 to 1996 preceding the introduction of endoscopic examination were 51.9 for males and 26.6 for females, while mean values for the 10-year period from 1997 to 2006 following the introduction of endoscopic examination were 28.0 for males and 6.9 for females (Figure 4).
SMR (standard mortality ratios) were then determined from the Nagasaki Prefecture data. The data were divided into two groups, representing the 7-year period from 1990 to 1996 and the 10-year period from 1997 to 2006. As noted above, since all cases of gastric cancer death in 1996 were detected in fiscal year 1995, they were included in the first period. For the first period, the 1995 Kamigoto population and the 1995 Nagasaki Prefecture gastric cancer death rates (per 100 000 population) were used; for the second period, the corresponding figures for 2000 were used. The mean SMR values were calculated separately for males and females. For the first period, the results were 1.04 (95% CI: 0.50-1.58) for males and 1.54 (95% CI: 0.71-2.38) for females, while for the second period they were 0.71 (95% CI: 0.33-1.10) for males and 0.62 (95% CI: 0.19-1.05) for females (Table 2).
A gastric X-ray examination costs ¥3000 per person, while an endoscopic examination costs ¥11 000 per person. Endoscopic examinations are thus more costly, but the cost incurred per gastric cancer case after discovery was ¥6 391 500 for the gastric X-ray examination group and ¥2 819 928 for the endoscopic examination group, making the cost-benefit ratio superior for the endoscopic examination group (Table 3).
| X-ray | Endoscope | |
| Total number (a) | 4261 | 7178 |
| Cost (b) | ¥3000 | ¥11 000 |
| No. gastric cancers (n) | 2 | 28 |
| Gross cost (a × b) | ¥12 783 000 | ¥78 958 000 |
| Cost to detect one case of gastric cancer (a × b/n) | ¥6 391 500 | ¥2 819 928 |
In the subject groups considered in this study, no case of incidental disease and endoscopy-related infection discovered by endoscopic examination and requiring medical intervention has yet been discovered.
The number of gastric cancer cases discovered annually in Japan is 103 685 (estimated, 1999), and the number of deaths from gastric cancer is 49 535 (confirmed, 2003), placing gastric cancer first in Japan among cancers in terms of number of new cases and second only to lung cancer in terms of deaths. In Nagasaki Prefecture in 2000, gastric cancer morbidity was 130.1/100 000 for males and 57.5/100 000 for females, compared to mean values of 95.2/100 000 for males and 55.9/100 000 for females in Kamigoto for the 6-year period from 1998 to 2003. Thus, morbidity was significantly lower in males in Kamigoto than in males in Nagasaki Prefecture.
Numerous studies have reported that gastric endoscopy is more effective than gastric X-ray examination in discovering small lesions and for qualitative diagnosis, and similarly for assessing gastric cancer detection rates and early gastric cancer ratios. However, according to the fiscal year 2003 Compendium of National Statistics from Gastroenterology Mass Survey, 5 975 956 individuals underwent gastric X-ray examination as part of gastric mass screening, compared to 68 923 who underwent endoscopy, showing that gastric X-ray examination still tends to be used for screening. Gastric cancer detection rate was 0.1% in the gastric X-ray examination group, compared to 0.24% in the endoscopy examination group[1]. In our study, the significant increase in gastric cancer detection after the introduction of endoscopic screening may reflect the aging of our study’s participants.
The finding that gastric X-ray screening reduced gastric cancer death rates among both men and women was obtained in case-controlled research by Oshima et al[2], Fukao et al[3], and Abe et al[4], and by a meta-analysis by Tsubono et al (males OR: 0.39, 95% CI: 0.29-0.52; females OR: 0.50, 95% CI: 0.34-0.72)[5]. Mizoue et al[6] also carried out multicenter, cooperative research in a large-scale research cohort comprising 30 771 screening group subjects and 56 541 control group subjects who were followed for 8 years. Males demonstrated a 46% reduction in death rate (RR: 0.54, 95% CI: 0.41-0.70), females exhibited a 26% reduction in death rate (RR: 0.74, 95% CI: 0.52-1.07), and among those with a prior history of gastric cancer in either parent, further reduction in death rate was noted (RR: 0.32, 95% CI: 0.12-0.87). A cohort studied by Lee et al[7] comprising 15 189 screening group subjects and 26 961 control group subjects was followed for 13 years and exhibited a 48% reduction in death rate (RR: 0.52, 95% CI: 0.36-0.74). Research by Arisue et al[8] compared a gastric cancer high-screening region to a low-screening region, and demonstrated a reduction in death rate of 30.2% among males and 36.5% among females in the high-screening region (P < 0.05). Reductions of death rate of 14.1% among males and 22.6% among females were observed in the low-screening region (P < 0.05).
With regard to reduction of gastric cancer death rate by endoscopic examination, Riecken et al[9] performed multiple endoscopic screenings from 1989 to 1999 among a Chinese cohort comprising 4394 residents of Linqu County, a gastric cancer cluster area. During a follow-up period extending to 2000, 85 individuals developed gastric cancer, of whom 29 (34%) were found to have early-stage cancer, while 58 (68%) had cancer discovered on screening. Gastric cancer SMRs among these subjects during follow-up were 1.01 (95% CI: 0.72-1.37), and 1.13 (95% CI: 0.77-1.57) for males and 0.65 (95% CI: 0.26-1.32) for females. The SMRs for two groups representing subjects from 1989-1994 (initial cohort) and those from 1995-2002 (interventional trial cohort) did not differ, at 0.97 (95% CI: 0.50-1.66) for the initial cohort and 1.08 (95% CI: 0.72-1.55) for the interventional trial cohort, and the study reported no observation of reduction of death rates. Other than the Riecken study, no studies have evaluated survival prognosis.
Rather than compare a screening group and a non-screening group, our study examined screened individuals and used two methods to analyze outcomes before and after the introduction of endoscopic screening: a direct method, involving age-adjusted death rate, and an indirect method, involving SMR. In each case, Kamigoto subject data were compared to those from Nagasaki Prefecture. Age-adjusted death rates for the Kamigoto females were clearly lower than those for Nagasaki Prefecture. Results for the Kamigoto males were also lower overall, but also reflect poor stability of death rates, a weakness of the direct method attributable to inclusion of a small subject group. We, therefore, also evaluated results by SMR, which is applicable to analysis at the city-, town-, and village-unit levels. Analysis was performed using gastric cancer death rates for Kamigoto and for Nagasaki Prefecture, and a notable reversal was observed at the point at which endoscopic screening was introduced. Although it would be premature to conclude that endoscopic screening decreased gastric cancer deaths, this conclusion has begun to be supported by follow-up data obtained 10 years after this introduction.
Issues requiring further attention include detailed identification of high-risk gastric cancer groups, screening intervals, geriatric screening, and screening rates. Detection of H pylori infection, measurement of serum pepsinogen, and other methods have come into use in gastric cancer screening and are expected to provide screening markers for gastric cancer.
Increase in screening rate is also a factor determining the effectiveness of gastric cancer screening, and efforts to increase screening rates require the creation of an organized system for screening, as opposed to opportunistic screening. Partnership with local governments is crucial for development of an organized screening system. Since the introduction of gastric endoscopy screening in Kamigoto, the mean screening rate there has been 28.2%, and efforts to communicate these research results, promote screening, and undertake interventions are expected to further increase this rate.
In the Kamigoto area, endoscopic screening was implemented in an organized fashion. In the future, we intend to further increase the screening rate in partnership with local governments. The introduction of endoscopic screening increased early gastric cancer detection rates and EMR cases in particular. Since age-adjusted gastric cancer mortality and SMR in Kamigoto also declined after the introduction of endoscopic screening, the results of this study suggest that endoscopic screening probably decreased gastric cancer deaths. We believe our results provide further evidence that use of endoscopic examination for gastric cancer screening should be recommended.
An abstract of this paper was presented at the Current Issues in Upper Gastrointestinal Endoscopy Symposium at the 70th General Meeting of the Japan Gastroenterological Endoscopy Society (DDW-Japan Kobe).
S- Editor Zhu LH L- Editor Alpini GD E- Editor Liu Y
| 1. | Fiscal year 2003 Compendium of National Statistics from Gastroenterology Mass Survey. Tokyo: Japanese Society of Gastroenterology Mass Survey, National Statistics Committee (in Japanese) 2005; 96-109. |
| 2. | Oshima A, Hirata N, Ubukata T, Umeda K, Fujimoto I. Evaluation of a mass screening program for stomach cancer with a case-control study design. Int J Cancer. 1986;38:829-833. [RCA] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 107] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Fukao A, Tsubono Y, Tsuji I, HIsamichi S, Sugahara N, Takano A. The evaluation of screening for gastric cancer in Miyagi Prefecture, Japan: a population-based case-control study. Int J Cancer. 1995;60:45-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Abe Y, Mitsushima T, Nagatani K, Ikuma H, Minamihara Y. Epidemiological evaluation of the protective effect for dying of stomach cancer by screening programme for stomach cancer with applying a method of case-control study--a study of a efficient screening programme for stomach cancer. Nihon Shokakibyo Gakkai Zasshi. 1995;92:836-845. [PubMed] |
| 5. | Tsubono Y, Hisamichi S. Case-control studies of screening for gastric cancer in Japan (in Japanese). Nippon Shokaki Syudankenshin Gakkai Zasshi (Jpn J Gastroenterol Mass Survey). 1999;37:182-185. |
| 6. | Mizoue T, Yoshimura T, Tokui N, Hoshiyama Y, Yatsuya H, Sakata K, Kondo T, Kikuchi S, Toyoshima H, Hayakawa N. Prospective study of screening for stomach cancer in Japan. Int J Cancer. 2003;106:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 97] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki S, Tsugane S. Gastric cancer screening and subsequent risk of gastric cancer: a large-scale population-based cohort study, with a 13-year follow-up in Japan. Int J Cancer. 2006;118:2315-2321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Arisue T, Tamura K, Yoshida Y, Tebayashi A, Yamaguchi Y, Ikeda S, Ohtuka S. Comparisons of the changes in the mortality from stomach cancer between the model areas of mass screening for stomach cancer and the control areas (in Japanese).. Nippon Shokaki Syudankenshin Gakkai Zasshi (Jpn J Gastroenterol Mass Survey). 1986;73:26-32. |
| 9. | Riecken B, Pfeiffer R, Ma JL, Jin ML, Li JY, Liu WD, Zhang L, Chang YS, Gail MH, You WC. No impact of repeated endoscopic screens on gastric cancer mortality in a prospectively followed Chinese population at high risk. Prev Med. 2002;34:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |